7-Hydroxymitragynine: A Promising Analgesic From Kratom (Mitragyna speciosa)
Could 7-hydroxymitragynine eventually replace common painkillers?
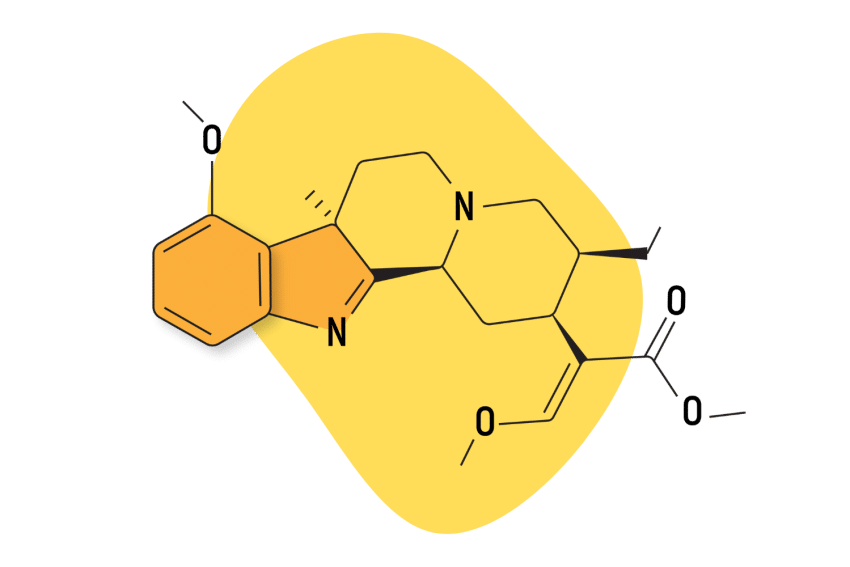
The kratom tree (Mitragyna speciosa) has a wide array of effects thanks to its many alkaloids. 7-hydroxymitragynine is one of the primary alkaloids and a large reason for the plant’s potent painkilling abilities [1].
It isn’t an opioid, but it acts similarly and can cause relaxation, sedation, and euphoria. Research is limited but suggests it’s stronger — and safer than morphine.
7-hydroxymitragynine is estimated to make up about 2% of the alkaloids contained within kratom leaves. The most abundant alkaloid in the plant is mitragynine, which makes up about 60% of the alkaloid content but is much weaker in terms of its effects.
What Does 7-Hydroxymitragynine Do?
7-hydroxymitragynine acts as an opioid in the body. Its primary effects are painkilling, sedating (especially in high doses), and euphoric. It also acts on the adrenergic receptors to increase both mental and physical energy levels.
This alkaloid has an affinity for three types of opioid receptors in the human body: mu-opioid receptors, delta-opioid receptors, and kappa-opioid receptors [2,3].
Opioid receptors are largely responsible for our perception of pain and pleasure. Opiates bind to these receptors to produce feelings of euphoria (pleasure) and reduce negative stimuli (pain).
Here are the primary effects of 7-hydroxymitragynine:
1. Pain Relief
The most notable effect provided by 7-hydroxymitragynine is pain relief — one of the primary uses for kratom. In fact, research shows it’s roughly 13 times more potent than morphine (in terms of binding affinity) [4].
All three opioid receptors mentioned above are linked to how we perceive pain. Compounds in opiates and opiate-like substances — like kratom — bind to these receptors and reduce the number of pain signals traveling to the brain. Pain reduction is a direct result of fewer pain signals traveling through the central nervous system (CNS).
Additionally, these opioid receptors affect how our bodies produce and process dopamine, the “feel good” neurotransmitter.
Mu-opioid receptors increase the production of dopamine in the brain, specifically, and the positive feelings from the bump in dopamine can change how the user perceives the pain signals that continue to travel through the body.
2. Anxiety Relief & Sedation
The reason humans feel anxiety isn’t well understood, but experts believe that the neurotransmitter gamma-aminobutyric acid (GABA) has a lot to do with it.
It’s believed that GABA can reduce the CNS signals transmitted to the brain. Overall, a quieter CNS means fewer feelings of anxiety. For this reason, controlling GABA is the primary target of depressants like benzodiazepines.
7-hydroxymitragynine has an agonistic effect on GABA receptors, meaning it increases the impact GABA has on its receptors. This effect reduces signals within the brain and spinal cord, thereby reducing anxiety and racing thoughts [5].
3. Mood Elevation
Dopamine is the body’s way of regulating pleasure and motivation, so a surge of dopamine can make someone experience intense feelings of euphoria and satisfaction.
Mu-opioid receptors are believed to be responsible for regulating dopaminergic signals.
7-hydroxymitragynine has been shown to bind to mu-opioid receptors [6]. Much like an opiate induces feelings of pleasure and happiness, kratom can make the user feel euphoric through this interaction.
When this alkaloid is present in the body, mu-opioid receptors trigger the production of dopamine in the ventral tegmental area (VTA) of the brain. This produces positivity, motivation, and positive feelings in the user [7].
Where Is 7-Hydroxymitragynine Found In Nature?
This alkaloid is only found in the kratom plant and its close relatives. Kratom (Mitragyna speciosa) is indigenous to Indonesia and surrounding tropical countries.
There are currently no other known natural sources of 7-hydroxymitragynine.
What Is a Typical Dose of 7-Hydroxymitragynine?
7-hydroxymitragynine is found in very small concentrations in the kratom plant but can be concentrated in the form of extracts.
Studies have shown that the pure extract of 7-Hydroxymitragynine doesn’t offer the same benefits as plant samples that contain other active alkaloids as well. Therefore, the best way to take 7-Hydroxymitragynine is to use the raw herb.
It’s difficult to offer a specific dose of 7-Hydroxymitragynine when used in raw plant form, as every sample is unique. Alkaloid ratios vary according to growing conditions, altitude, post-harvest process, and more.
It’s more common to dose kratom alkaloids based on the weight of the raw kratom leaf powder being consumed.
For example, standard kratom doses are as follows:
- For stimulation and nootropic effects: 1 to 2 grams
- For balanced stimulation and anxiety relief: 2 to 4 grams
- For pain relief and sedation: 5 to 8 grams
These doses vary due to several factors, including the user’s experience, body weight, and the powder’s potency, among other things.
In general, plants that have a higher 7-hydroxymitragynine are preferred for managing pain and mood or for their sedative actions.
Which Kratom Strains Are Highest In 7-Hydroxymitragynine?
Red-veined kratom has the highest 7-hydroxymitragynine levels on average — compared to a green vein or white vein.
Unfortunately, the concentration of 7-hydroxymitragynine among samples of a singular strain can vary. Some vendors test alkaloid levels, allowing you to see what percentages are in the specific batch. Without the tests, there’s no way to know for sure.
There are a handful of strains that tend to test the highest in 7-hydroxymitragynine — such as:
- Red Maeng Da Kratom
- Red Borneo Kratom
- Red Bali Kratom
- Green Bali Kratom
There is some debate about whether or not the three primary kratom colors — red, white, and green — actually exist, but the common consensus is that they do and are noticeably different.
While red-vein kratom is considered to have the highest 7-OH-mitragynine (and is, therefore, the best for pain and anxiety relief), some green and white strains have high concentrations of this alkaloid, too, and can provide similar effects.
How Long Does 7-Hydroxymitragynine Last In the Body?
The effects of 7-hydroxymitragynine usually kick in within about 30 minutes and remain active for two to five hours.
Like most other alkaloids, 7-hydroxymitragynine is processed by the liver, with the biological half-life sitting between two and three hours. The duration can range depending on consumption methods, whether or not kratom was taken with food or other substances, and individual differences in liver metabolism.
Is 7-Hydroxymitragynine Addictive?
Kratom, in general, can be addictive, just as any substance with physiological effects can be.
It’s also likely, given the effects 7-hydroxymitragynine has on opioid receptors.
Some users may become psychologically dependent on 7-hydroxymitragynine due to the surge of dopamine or the decrease in perceived pain, anxiety, or insomnia.
As kratom increases in popularity in the US, more and more is understood about how addictive and habit-forming it can be. Most people agree that limiting use to just a few days a week and once per day on those days will help avoid dependency. A common recommendation is to take a week off from using kratom at least once per month to reduce the risk of addiction.
Is 7-Hydroxymitragynine Safe?
Aside from addiction, there are some potential health risks associated with using kratom. These include liver and kidney issues, adrenal fatigue, and cloudy thoughts or decision-making.
Generally speaking, though, most people agree that mild to moderate use of 7-hydroxymitragynine is relatively safe, provided the user follows guidelines to help prevent addiction.
Final Thoughts: 7-Hydroxymitragynine
Along with the other alkaloids in kratom, 7-hydroxymitragynine shows promise as a potentially medicinal compound. As long as it’s used responsibly and carefully so as to avoid dependency, it can provide a variety of beneficial effects, including pain relief and anxiety reduction.
Not only can 7-hydroxymitragynine potentially be helpful in treating these conditions but it has also been used successfully to help those addicted to opioids wean off of them.
Kratom is considered significantly safer for continued use than opioids, which means replacing hard drug use with the natural herb can be massively beneficial. Since 7-hydroxymitragynine mimics a weak opioid, it has also been used to reduce the symptoms associated with opioid withdrawal.
References
- Spetea, M., & Schmidhammer, H. (2019). Unveiling 7-Hydroxymitragynine as the Key Active Metabolite of Mitragynine and the Promise for Creating Novel Pain Relievers<? ACS-CT-END-Insert?>.
- Matsumoto, K., Horie, S., Ishikawa, H., Takayama, H., Aimi, N., Ponglux, D., & Watanabe, K. (2004). Antinociceptive effect of 7-hydroxymitragynine in mice: Discovery of an orally active opioid analgesic from the Thai medicinal herb Mitragyna speciosa. Life sciences, 74(17), 2143-2155.
- Suhaimi, F. W., Yusoff, N. H., Hassan, R., Mansor, S. M., Navaratnam, V., Müller, C. P., & Hassan, Z. (2016). Neurobiology of Kratom and its main alkaloid mitragynine. Brain research bulletin, 126, 29-40.
- Matsumoto, K., Horie, S., Ishikawa, H., Takayama, H., Aimi, N., Ponglux, D., & Watanabe, K. (2004). Antinociceptive effect of 7-hydroxymitragynine in mice: Discovery of an orally active opioid analgesic from the Thai medicinal herb Mitragyna speciosa. Life sciences, 74(17), 2143-2155.
- Nusantara, G. B., & Tuba, S. (2022). Resilience State Security and the Role Sedative Agents in Military Pharmacy for State Defense in Future War. Budapest International Research in Exact Sciences (BirEx) Journal, 4(2), 131-137.
- Pathan, H., & Williams, J. (2012). Basic opioid pharmacology: an update. British Journal of Pain, 6(1), 11-16.
- Kosten, T. R., & George, T. P. (2002). The neurobiology of opioid dependence: implications for treatment. Science & practice perspectives, 1(1), 13.