3-hydroxyphenazepam: The Ultimate Harm Reduction Guide
You won’t find 3-hydroyphenazepam at your local pharmacy — this drug is a research chemical only found on designer drug markets. Here’s what we know about this substance so far.
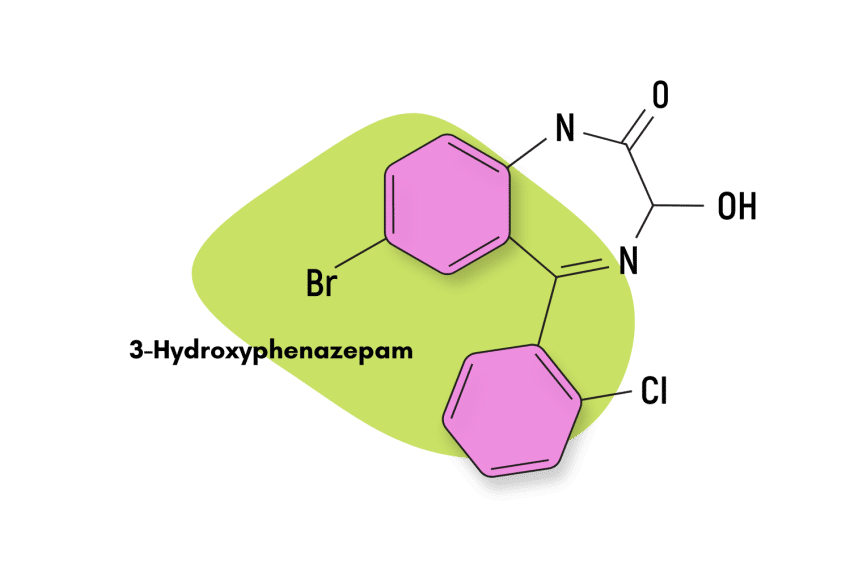
3-hydroxyphenazepam is a classical 1,4-benzodiazepine that hasn’t received approval as a medication. It’s exclusively sold as a designer benzodiazepine drug (DBZD) and an alternative to conventional benzodiazepines like alprazolam (Xanax) or clonazepam (Klonopin).
This compound is an active metabolite of phenazepam and a byproduct of the prodrug cinazepam [1].
3-hydroxyphenazepam displays all the pharmacological properties usually associated with benzodiazepines. However, according to the scant research available, it acts mainly as a sedative and anticonvulsant [2].
3-hydroxyphenazepam Specs
| Status | Research chemical |
| Common Dosage | Unspecified |
| PubChem ID | 125820 |
| CAS# | 70030-11-4 |
IUPAC Name: 7-Bromo-5-(2-chlorophenyl)-3-hydroxy-1,3-dihydro-2H1,4-benzodiazepine-2-one
Other Names: None
Metabolism: Cinazepam and its metabolites —including 3-hydroxyphenazepam —were almost entirely (> 90%) eliminated in urine and feces during the period of study (5-10 days), which means that no significant accumulation of the drug in the body occurred.
Duration of Effects: Unknown
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does 3-hydroxyphenazepam Work?
As a classical 1,4-benzodiazepine, 3-hydroxyphenazepam is known to exert its pharmacological effects through the classical GABA-mediated pathway [3]. This effect inhibits or slows electrical activity in the brain and results in the characteristic “relaxing” effects the drug is known for. This is the same mechanism of action shared by the lion’s share of benzodiazepine drugs on the market today.
Although little research has been conducted into the pharmacological specifics of 3-hydroxyphenazepam, some knowledge allows us to know more about how this compound exerts its effects.
For instance, research has shown significant differences in how 3-hydroxyphenazepam and cinazepam — the compound 3-hydroxyphenazepam is converted into by the liver — behave at GABA-A receptor sites.
This active metabolite is responsible for the majority of 3-hydroxyphenazepam’s effect profile.
One study found that cinazepam increased synaptic vesicle acidification and hyperpolarization, whereas 3-hydroxyphenazepam demonstrated opposite effects [4].
It’s reasonable to assume that these differences lead to significant alterations in the pharmacological profile of both compounds. In this sense, we do know that, relative to phenazepam, another parent drug, 3-hydroxyphenazepam, has diminished myorelaxant properties, although it is comparable in most other aspects.
Is 3-hydroxyphenazepam Safe? Risks & Side Effects
Given how little formal information we have on this molecule, it’s hard to compare how 3-hydroxyphenazepam measures up to other benzodiazepines regarding risk levels. However, what we do know about the compound is more than enough to make some general statements.
The pharmacological profile of 3-hydroxyphenazepam means that it shares the common hazards associated with benzodiazepine use, mainly the risk of becoming physically dependent on the drug.
Were it not an obscure research chemical, it is likely that, along with most other benzodiazepines, 3-hydroxyphenazepam would receive a Schedule IV classification in the Controlled Substances Act.
Side Effects of 3-hydroxyphenazepam
All benzodiazepines share a common set of adverse effects. With the exception of specific side effects being more common in some benzodiazepines than others, all benzodiazepines exhibit the following side effects, although to differing degrees.
Common side effects of benzodiazepine drugs:
- Blurred vision
- Confusion
- Constipation
- Dizziness
- Drowsiness
- Dry mouth
- Light-headedness
- Memory problems
- Muscle weakness
- Nausea (feeling sick)
- Slurred speech
- Unsteadiness (especially in older people, who may fall and experience injuries)
Some less common side effects of benzodiazepines include:
- Changes in sexual libido
- Difficulty urinating
- Digestive disturbances
- Headaches
- Incontinence (loss of bladder control)
- Increased saliva production
- Low blood pressure
- Rashes
- Sight problems, such as double vision
- Tremors (shaking)
Some rare side effects of benzodiazepines include:
- Blood disorders
- Jaundice (yellow skin & eyes)
Benzodiazepine Withdrawal & Dependence
The considerable danger posed by benzodiazepine withdrawals is one of the most significant risk factors doctors have to deal with when prescribing benzodiazepines. Most people believe that if they avoid misuse, they will not expose themselves to this risk meaningfully, but this is an erroneous belief.
The possibility of developing a benzodiazepine withdrawal is real, even if treatment occurs for a limited period, say two to four weeks.
A recent study that examined this possibility found that over one-third of participants in a group of people who used benzodiazepines for more than four weeks developed withdrawal symptoms, a tell-tale sign of physical dependence [5].
Users must be aware of this risk because benzodiazepine dependence entails many things. It means users will have to go through a process of drug-tapering to get off benzodiazepines safely, which can often take a considerable amount of time. Quitting benzodiazepines cold turkey is not an option: withdrawals from benzodiazepines and alcohol can turn fatal, so users must do all they can to avoid these symptoms.
Harm Reduction: 3-hydroxyphenazepam
There are always specific rules of thumb that users can employ to minimize their risk factors. Follow the recommendations in this section to stay safe!
General recommendations
Guidelines For the Responsible Use of Benzodiazepines:
- 🥣 Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- ⏳ Take frequent breaks or plan for a short treatment span — Benzodiazepines can form dependence quickly, so it’s important to stop using the drug periodically.
- 🥄 Always stick to the proper dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- 💊 Be aware of contraindications — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- 🧪 Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- 💉 Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- 🌧 Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- ⚖️ Understand the laws where you live — In most parts of the world, benzodiazepines are only considered legal if given a prescription by a medical doctor.
- 📞 Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Look up “addiction hotline” for more information where you live. (USA: 1-800-662-4357; Canada: 1-866-585-0445; UK: 0300-999-1212).
3-hydroxyphenazepam Drug Interactions
When it comes to benzodiazepines, users should always avoid certain drug combinations. Any potent pharmacological compound should be avoided unless with the approval of a doctor, but special care should be taken to avoid other central nervous system-depressant compounds like opioids, barbiturates, or other benzodiazepines.
This combination can often result in respiratory depression: the leading cause of death among drug overdoses.
3-hydroxyphenazepam Contraindications
Most benzodiazepines share a common set of contraindications that users should be aware of so they don’t unknowingly expose themselves to risk.
- Bronchitis
- Chronic obstructive pulmonary disease (COPD)
- Common contraindications for benzodiazepines are:
- Conjunctive use of barbiturates, opiates, or those suffering from alcoholism
- Intellectual disabilities due to frequent paradoxical reactions
- Major depression
- Myasthenia gravis
- Over the age of 65 (high risk)
- Personality disorders
- Sleep apnea
Similar Benzodiazepines
Since the pharmacokinetics of 3-hydroxyphenazepam are not well understood, it is hard to determine which benzodiazepine compounds are comparable. However, 3-hydroxyphenazepam is related to other benzodiazepines in metabolic terms.
Phenazepam
3-hydroxyphenazepam is an active metabolite of the benzodiazepine phenazepam. User reports suggest that both compounds have roughly comparable effect profiles, but there hasn’t been any research to confirm.
Cinazepam
Cinazepam is a prodrug for 3-hydroxyphenazepam. This means that cinazepam is metabolized by the body into 3-hydroxyphenazepam. So the effects of these compounds are closely related. However, cinazepam is also considered an atypical benzodiazepine which means it doesn’t target the GABA receptors the same way other classical benzodiazepines do. This gives cinazepam unique differences for the first 1–3 hours after taking this drug. The conversion to 3-hydroxyphenazepam suggests both drugs have a similar effect profile as cinazepam is metabolized.
Alternatives to Benzodiazepines
There are a myriad of natural benzodiazepine-like plants and nutrients available today. Most of which are perfectly legal and widely available around the world.
It’s important to note that none of these substances are as strong as prescription benzodiazepines, but the mechanism of action is similar. These plants are considered a safer long-term alternative to prescription medications and may be useful for avoiding synthetic benzodiazepines entirely.
Kava (Piper methysticum)
The kava plant is a tropical plant species that has been found to exert natural anxiolytic and sedative effects, although less potent than benzodiazepines, are reasonably effective. Like benzodiazepines, active ingredients contained within the kava plant bind to GABA-A receptors and produce feelings of relaxation and calm [6]. And the best part is that kava can do this while offering users a much more benign side effects profile!
Kratom (Mitragyna speciosa)
The kratom plant is a go-to choice for users looking to avoid using prescription drugs. This plant is commonly used as an alternative to opiate painkillers, but it also offers similar anxiolytic and sedative effects to benzodiazepines when taken in the higher dosage range.
Kratom does have the potential to cause side effects and dependence, but this is only a significant risk in users who are compulsive about their consumption. In relative terms, kratom is still a much safer choice than prescription benzodiazepines.
3-hydroxyphenazepam FAQs
Is 3-hydroxyphenazepam available for purchase?
3-hydroxyphenazepam is not an approved medication and is only available through illegal outlets. Order at your own risk.
Where was 3-hydroxyphenazepam developed?
Phenazepam, a parent drug of 3-hydroxyphenazepam, was the first benzodiazepine designer drug to appear on the market. It was believed to have been developed in the Soviet Union in the 1970s. Given the fact that 3-hydroxyphenazepam is an active metabolite of this compound and its relative obscurity to western researchers, it’s likely this compound was also developed in Russia and the former soviet states.
References
- Schukin, S. I., Zinkovsky, V. G., & Zhuk, O. V. (2011). Elimination kinetics of the novel prodrug cinazepam possessing psychotropic activity in mice. Pharmacological Reports, 63(5), 1093-1100.
- Golovenko, N. Y., Larionov, V. B., Kravchenko, I. A., Ovcharenko, N. V., & Aleksandrova, A. I. (2002). Biokinetics of transdermal 3-hydroxyphenazepam. Bulletin of Experimental Biology and Medicine, 134(3), 254-256.
- Kopanitsa, M. V., Zbarska, S. M., Boychuk, Y. A., & Krishtal, O. A. (2000). Modulation of GABA-activated currents by phenazepam and its metabolites in isolated rat Purkinje neurons. Neurophysiology, 32(3), 192-192.
- Borisova, T., Pozdnyakova, N., Dudarenko, M., Krisanova, N., & Andronati, S. (2021). GABAA receptor agonist cinazepam and its active metabolite 3-hydroxyphenazepam act differently at the presynaptic site. European Neuropsychopharmacology, 45, 39-51.
- Riss, J., Cloyd, J., Gates, J., & Collins, S. (2008). Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta neurologica scandinavica, 118(2), 69-86.