Flumazenil (Anexate): The Benzodiazepine Antidote
Flumazenil — commercially available as Anexate, Lanexat, Mazicon, and Romazicon — is a benzodiazepine receptor antidote used for treating overdoses on other members of the benzodiazepine family.
Flumazenil has the opposite effects to most benzos. For example, rather than reducing anxiety-like other benzodiazepines, flumazenil induces it.
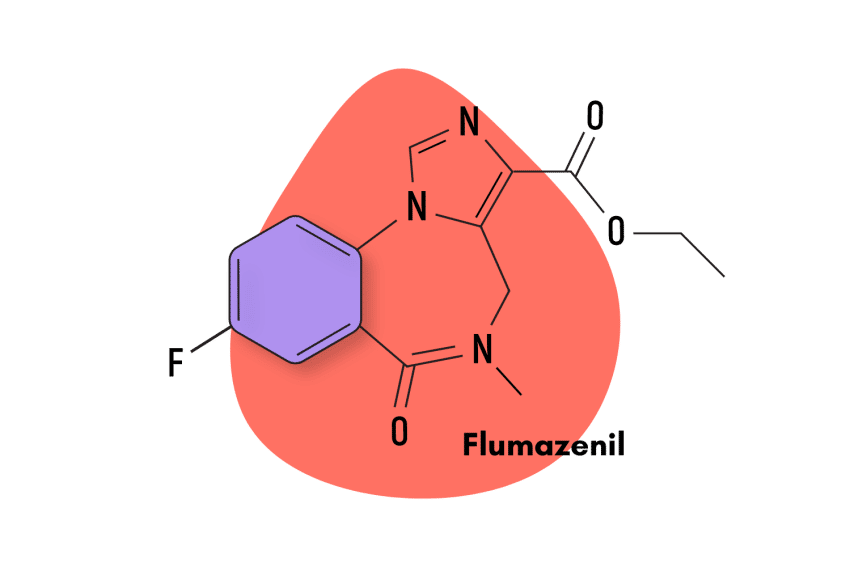
Structurally, flumazenil is classified as a 1,4-imidazobenzodiazepine closely related to another benzodiazepine derivative called bretazenil. Unlike flumazenil, bretazenil maintains the classic benzodiazepine effects.
Approved by the FDA in 1991, flumazenil is only commercially available as an injectable drug.
Flumazenil Specs
| Status | Approved (Antidote) 💊 |
| Common Dosage | Unspecified |
| PubChem ID | 3373 |
| CAS# | 78755-81-4 |
IUPAC Name: Ethyl 8-fluoro-5-methyl-6-oxo-4H-imidazo[1,5-a][1,4]benzodiazepine-3-carboxylate
Other Names: Anexate, Lanexat, Mazicon, & Romazicon
Metabolism: Flumazenil’s metabolism is 99% hepatic. Very little flumazenil (<1%) is found in the urine.
Duration of Effects: Short-Acting. The initial distribution half-life of flumazenil is 4 to 11 minutes, and the terminal half-life is 40 to 80 minutes. Prolongation of the half-life to 1.3 hours in patients with moderate hepatic impairment and 2.4 hours in severely impaired patients.
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Flumazenil Work?
Traditional benzodiazepine medications increase the activity of the target receptors (GABA-A). GABA increases the flow of chloride ions into the neurons, which reduces its ability to fire electrical signals. This action slows brain activity and is what gives benzodiazepines their sedating qualities.
Flumazenil binds to the same benzodiazepine receptors as other members of this class. Still, instead of increasing the chloride flow, flumazenil blocks this compound’s intake, thus increasing the action potential of the cell [2,3]. Logically, this action delivers the opposite effects to most other benzodiazepine drugs. Flumazenil can induce anxiety, insomnia, and muscle tension — rather than alleviate it.
This blocking action makes flumazenil helpful in reversing the effects of benzodiazepines. Flumazenil competes for the binding sites with other benzodiazepines, blocking their effects. This is useful for treating overdoses or waking patients who have been sedated by other benzodiazepines.
Flumazenil Pharmacokinetics
Flumazenil’s effects are fast-acting, a major reason it is clinically effective at reducing the effects of benzodiazepine overdose, such as respiratory depression. Effective benzodiazepine antagonism begins approximately one to two minutes after intravenous injection and reaches peak concentrations in six to 10 minutes, lasting up to one hour.
However, flumazenil has a shorter duration of action than most benzodiazepines, with its elimination half-life being 0.7 to 1.3 hours. This can be a potential problem when attempting to revert the effects of a benzodiazepine overdose. The duration and efficacy of the antagonistic effect depend on the given plasma concentrations of benzodiazepines in the affected patient and the amount of flumazenil that is administered. If the sedative and respiratory effects of the benzodiazepine last longer than the antagonistic effects of flumazenil, the patient could still be at risk [3].
Is Flumazenil Safe? Risks & Side Effects
Due to the particular nature of flumazenil, its usage has some important considerations when it comes to benzodiazepine misuse. But before we examine the specifics of flumazenil, let’s look at the general situation concerning benzodiazepine misuse in the United States.
Benzodiazepine Misuse Statistics
It is no secret that drug-related fatalities have been trending upward in recent years, and benzodiazepines have a part to play in that. Even though the opioid epidemic has garnered most of the media attention regarding this subject, the reality is that a smaller but still very significant benzodiazepine crisis has also developed.
And the statistics certainly bear this out. A recent 2020 survey by the CDC informs us that, in that year, benzodiazepines were involved in a total of 12,290 deaths in the United States. Another study by the National Institute on Drug Abuse (NIDA) helps us understand how the benzodiazepine situation relates to the opioid situation. According to the study: 16% of opioid overdose deaths in the United States also involve benzodiazepine use.
With data from the National Institute on Drug Abuse, we can look at the broader trend over the past twenty years.
It’s clear how benzodiazepine deaths have steadily risen since 1999. There was a brief drop plateau around 2010, but death rates started to climb again after the opioid crisis began in 2014.
Flumazenil & Benzodiazepine Misuse
When it comes to benzodiazepine misuse in the context of flumazenil, the situation is completely different. Because flumazenil does not exhibit the anxiolytic, hypnotic, and sedative effects of a traditional benzodiazepines, it carries much less risk of misuse. In fact, it is only commercially available as an injectable, which decreases this potential even further.
Flumazenil is one of the most important tools available to doctors and the general population in the fight against benzodiazepine-related fatalities. In this sense, it is very similar to naloxone, an opioid receptor antagonist used to reverse the effects of an opioid overdose.
If you are someone who regularly engages in the recreational use of benzodiazepines, it may be wise to acquire some flumazenil from a doctor ask them to show you how to use it. We do not recommend that anyone ever engage in benzodiazepine misuse but if it’s something you or someone you know is going to do, then having some flumazenil at hand is an important insurance policy for your health.
However, due to drug-related stigma, it can be hard for people who abuse benzodiazepines to seek help or even to ask a doctor what the proper way to administer flumazenil is. For this reason, clinics or groups that focus on harm reduction approaches for various types of drug use are an excellent resource to learn about the myriad harm reduction options available to drug users.
There is also an excellent argument for making flumazenil and other drugs like its more widely available. Currently, flumazenil remains a prescription drug in the United States, limiting its potential access and, thus, its ability to save lives. Unlike benzodiazepine agonists, flumazenil is not a controlled substance under the Controlled Substances Act.
Side Effects of Flumazenil
Multiple studies have demonstrated that high doses of flumazenil( up to 600 mg), both oral and intravenous (up to 100 mg), are safe and well tolerated [3]. There are side effects, though, mostly the ones that are typically related to benzodiazepines, like nausea, vomiting, dizziness, and headaches. However, many volunteer studies have documented a complete absence of serious adverse reactions. Compared to traditional benzodiazepine agonists, it is safe to say that flumazenil displays a much more benign side effects profile.
But this doesn’t mean that flumazenil is exempt from the possibility of serious adverse reactions. Other studies have documented the occurrence of seizures and cardiac irregularities after the administration of flumazenil [3]. However, the data suggests that these risks are much more prevalent in patients who have been on benzodiazepines for long-term sedation or in overdose cases where patients show signs of serious cyclic antidepressant overdose. If an overdose situation is serious enough to warrant the use of flumazenil, practitioners should be ready to manage a possible subsequent seizure.
Deaths have occurred following the use of flumazenil in a wide variety of clinical settings. However, it is hard to parse out what exact role flumazenil had in these instances, as they almost always occur in patients with severe underlying conditions or who have ingested large amounts of non-benzodiazepine drugs (usually cyclic antidepressants) as part of an overdose.
According to the FDA, the side effects associated with flumazenil include:
- Abnormal vision
- Agitation
- Anxiety
- Arrhythmia
- Bradycardia
- Confusion
- Cutaneous vasodilation
- Depression
- Euphoria
- Fatigue
- Flushing
- Headache
- Hiccups
- Hypertension
- Injection site pain
- Injection site reaction
- Insomnia
- Nausea
- Palpitations
- Paresthesia
- Speech disorders
- Sweating
- Tachycardia
- Tremors
- Vomiting
It’s important to note that almost all these adverse effects occur in only one to three percent of cases.
Benzodiazepine Withdrawal & Dependence
Due to the unique nature of flumazenil, virtually no one abuses the drug, and thus flumazenil dependence and withdrawals are not a real problem. In fact, there is substantial evidence that points to flumazenil’s ability to treat the symptoms of benzodiazepine withdrawal.
Harm Reduction: Flumazenil
Many general considerations can help people stay safe when taking benzodiazepines with or without a prescription. Obviously, the main recommendation would be to avoid all benzodiazepine misuse and only take benzodiazepines strictly following your prescription. However, in this article, we’re not interested in warding people off of drug abuse, although that’s important; we want to help people stay safe.
In this regard, one of the best recommendations is to consider what non-pharmacological options are available to you. If you’re looking for anxiolytic relief, plenty of herbal options like kratom and the kava plant are safe and effective. If what you’re looking for is to get high, then maybe consider far less dangerous options, like marijuana, 2CX substances, or MDMA.
Flumazenil Drug Interactions
Flumazenil is not a common recreational drug, so there isn’t much concern about what potential drug interactions can become harmful. What is important to note, though, that flumazenil cannot treat drug overdoses that involve drugs other than benzodiazepines. In fact, when it comes to certain drug types, like cyclic antidepressants, flumazenil is contraindicated and could even increase risk levels [4].
Contraindications of Flumazenil
According to the FDA, flumazenil is contraindicated in:
- Patients with a known hypersensitivity to flumazenil or benzodiazepines
- Patients given a benzodiazepine to control a potentially life-threatening condition (e.g., control of intracranial pressure or status epilepticus).
- Patients who are showing signs of severe cyclic antidepressant overdose
Flumazenil FAQs
Is flumazenil available in another formulation besides an injectable?
No. An oral formulation was attempted, but it was canceled during its clinical development due to low bioavailability.
What is flumazenil’s protein binding capability?
Protein binding is approximately 50%, mostly (66%) to albumin. Protein binding is reduced in patients with hepatic cirrhosis.
References
- Lader, M. H., & Morton, S. V. (1992). A pilot study of the effects of flumazenil on symptoms persisting after benzodiazepine withdrawal. Journal of Psychopharmacology, 6(3), 357-363.
- Brogden, R. N., & Goa, K. L. (1988). Flumazenil. Drugs, 35(4), 448-467.
- Sugarman, J. M., & Paul, R. I. (1994). Flumazenil: a review. Pediatric emergency care, 10(1), 37-43.
- Lheureux, P., Vranckx, M., Leduc, D., & Askenasi, R. (1992). Flumazenil in mixed benzodiazepine/tricyclic antidepressant overdose: a placebo-controlled study in the dog. The American journal of emergency medicine, 10(3), 184-188.
- Cairney, S., Clough, A. R., Maruff, P., Collie, A., Currie, B. J., & Currie, J. (2003). Saccade and cognitive function in chronic kava users. Neuropsychopharmacology, 28(2), 389-396.
- Swogger, M. T., & Walsh, Z. (2018). Kratom use and mental health: A systematic review. Drug and Alcohol Dependence, 183, 134-140.