Clobazam: Safety, Risks, Dosage & Harm Reduction
Clobazam — commercially available as Frisium or Onfi — is a prescription benzodiazepine medication. It was developed initially as an anxiolytic but is more commonly prescribed as a muscle relaxant today.
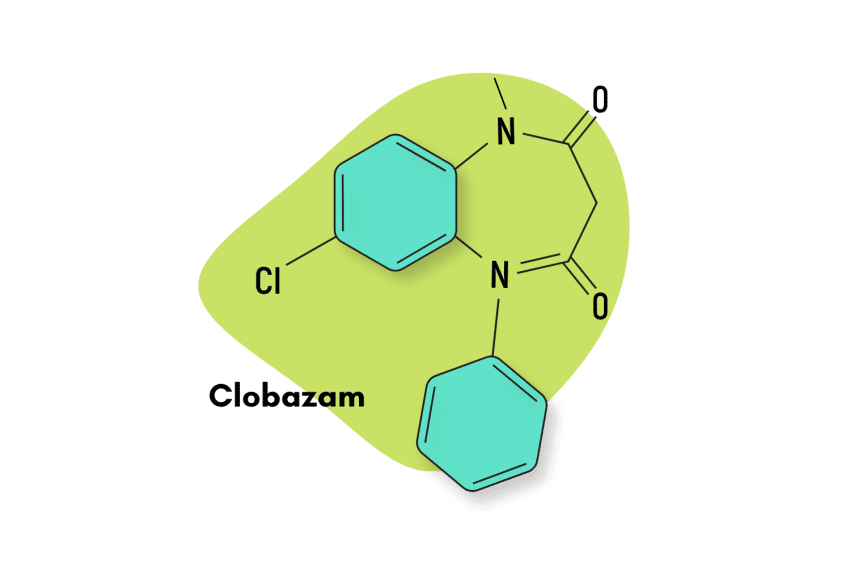
Clobazam has a different chemical structure than “traditional” 1,4 benzodiazepines, which have nitrogen atoms in the 1 and 4 positions. Instead, clobazam is classified as a 1,5 benzodiazepine similar to drugs like arefendazam and lofendazam.
Clobazam has a unique mechanism of action and is thought to carry a lower risk of side effects such as rebound insomnia or anxiety (unconfirmed).
Clobazam Specs
| Status | Approved ✅ |
| Common Dosage | 10–15 mg |
| PubChem ID | 2789 |
| CAS# | 22316-47-8 |
IUPAC Name: 7-chloro-1-methyl-5-phenyl-1,5-benzodiazepine-2,4-dione
Other Names: Onfi, Frisium, Urbanol
Metabolism: The major metabolic pathway of clobazam involves N-demethylation, primarily by CYP3A4 and to a lesser extent by CYP2C19 and CYP2B6.
Duration of Effects: Intermediate-Acting (6–12 hours). Clobazam is rapidly and extensively absorbed following oral administration. The time to peak concentrations of clobazam tablets under fasted conditions ranged from 0.5 to 4 hours after single- or multiple-dose administrations. The relative bioavailability of clobazam tablets compared to an oral solution is approximately 100%. The estimated mean elimination half-lives (t½) of clobazam and N-desmethylclobazam were 36-42 hours and 71-82 hours, respectively.
Dosage: Proper dosage is determined on a case-by-case basis.
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Clobazam Work?
Like most other benzodiazepines, clobazam is a positive allosteric modulator at the GABA-A receptors.
Wondering what that means? We’ll break it down for you.
Benzodiazepines exert their inhibitory effects on the brain and central nervous system (CNS) by interacting with GABA molecules at receptor sites along the CNS. Specifically, they bind to the GABA-A receptors at a site different from where GABA-A binds and potentiate the GABA-A neurotransmitter’s natural activity [1].
Benzodiazepine’s action upon GABA-A receptors increases the opening frequency of the chloride channel in the neuron, allowing chloride atoms to enter and hyperpolarize the neuron. Clobazam, specifically, also increases the production of the GABA transporter [2].
The hyperpolarization of the neuron’s membrane potential alters the electric charge inside it and makes it less likely the neuron will fire an action potential. Reduced action potential activity means reduced overall brain activity. This inhibitory effect gives benzodiazepines their anxiolytic, hypnotic, sedative, muscle relaxant, and anticonvulsant effects.
What Makes Clobazam Unique?
The most meaningful differences between benzodiazepines lie in the nitty-gritty of how they interact with GABA-A and other neurotransmitters to exert their inhibitory effects. Even slight differences in their mechanisms of action lead to significant variations in their effects and side effects.
GABA-A receptors are made up of five subunits, each one typically having αsubunits, two βsubunits, and one γsubunit [3]. Each subunit has multiple types.
These drugs are still not well understood, but we do know something about how clobazam differs when compared to traditional benzodiazepines. We know the α1 subunit mediates sedative effects while the α2 subunit controls anxiolytic effects; all αsubunits mediate anticonvulsant effects [4].
Additionally, clobazam binds in the junction between the α and γ2 subunits. It also has increased selectivity for α2 subunits over α1 subunits when compared to 1,4 benzodiazepines. It’s been suggested that this is why clobazam exhibits a decreased likelihood of causing sedation. Also, the selective binding may explain clobazam’s decreased potential to cause tolerance (theoretical) [5].
Is Clobazam Safe? Risks & Side Effects
To understand the danger one is risking when taking clobazam, it is key to understand the inherent risks in all benzodiazepine use and how they have taken their toll on the United States in recent years.
Benzodiazepine Misuse Statistics
The current situation regarding benzodiazepine use is quite alarming when one considers the dangers they represent. However, the problem has flown under the radar largely due to the severity and alarm caused by the opioid crisis. Still, there is a good argument to be made that a corresponding benzodiazepine crisis has also developed.
In a 2020 survey, the CDC showed how benzodiazepines were involved in 12,290 deaths in the US. Another National Institute on Drug Abuse (NIDA) study shows that 16% of opioid overdose deaths also involved benzodiazepines.
Looking at the broader trend, we can see how benzodiazepine-related deaths have increased steadily since 1999. They leveled off around 2010 but started climbing once again in 2014, mainly because of the explosion in concomitant opioid use. United States health authorities have recognized the seriousness of this trend and are taking strong action to reign in the explosion in opioid and benzodiazepine misuse. In 2016, the FDA warned healthcare professionals and consumers about the risks of mixing opioids with benzodiazepines and other CNS depressants.
Clobazam Misuse
Like all prescription drugs, clobazam use does imply certain risks. First of all, the United States classifies it as a Schedule IV drug under the Controlled Substances Act — despite its approved medical uses, it still carries the potential to develop physical dependence and withdrawal symptoms.
There is almost no data on how clobazam fits into the larger picture regarding benzodiazepine misuse. It is essential to understand the trends surrounding popular benzodiazepines with large numbers of prescriptions and a reputation for recreational abuse, such as clonazepam and alprazolam. However, compared to these popular benzodiazepines, clobazam misuse is almost a non-issue.
Side Effects of Clobazam
One of clobazam’s most remarkable features is the mildness of its side effects. In fact, during its development, one of the primary clinical goals was to create a drug with fewer benzodiazepine-like side effects but with effective anxiolytic properties. It has relatively mild side effects when compared to other antiepileptic drugs [5].
According to the FDA, clobazam is commonly associated with the following side effects:
- Ataxia
- Bronchitis
- Constipation
- Decreased/increased appetite
- Drooling
- Dysarthria
- Dysphagia
- Fatigue
- Insomnia
- Irritability
- Lethargy
- Pneumonia
- Psychomotor hyperactivity
- Pyrexia
- Somnolence or sedation
- Upper respiratory tract infection
- Urinary tract infection
- Vomiting
The FDA also includes the inherent risk of physical and psychological dependence involved in the use of clobazam. Additionally, research suggests clobazam’s side effects are dose-dependent, with milder doses leading to milder side effects [5].
We also know that, although very rare, the development of toxic epidermal necrosis (TEN) and Steven-Johnson syndrome (SJS) is possible. These adverse effects are very severe [6].
Clobazam Withdrawal & Dependence
Benzodiazepine withdrawal is similar to opioid and alcohol withdrawal — it can become serious enough to cause fatalities.
A benzodiazepine prescription likely implies a drug-tapering process once the treatment cycle has ended. Research shows that even with no misuse on the user’s part, benzodiazepine treatment is quite likely to cause physical dependence and withdrawal symptoms. One study concluded that nearly one-third of individuals who used benzodiazepines for longer than four weeks experienced dependence and withdrawal symptoms after completing the treatment [7].
Indeed, the likelihood of having to engage in drug tapering when using clobazam is not trivial whatsoever. In four Phase 1 studies where clobazam was discontinued abruptly, 68 of 207 patients suffered withdrawal adverse events. In contrast, in three Phase II or Phase III studies where clobazam was gradually tapered off over three weeks, none of the 87 participants experienced withdrawal adverse events [8].
As with most other prescription drugs, the higher the dosage and the longer clobazam is taken, the more a user exposes themselves to the possibility of developing an addiction. Additionally, users can develop a tolerance to clobazam’s antiepileptic effect [9]. For this reason, clobazam is not considered a long-term solution for treating epilepsy.
Harm Reduction: Clobazam
Stay safe by always sticking to these harm reduction principles.
Benzodiazepine Harm Reduction 101:
- Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- Take frequent breaks — Benzodiazepines can form dependence quickly, so it’s important to stop using them periodically.
- Know the dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- Know who should NOT use benzos for any reason — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
General Considerations
Benzodiazepine users should always keep in mind these basic harm reduction principles. They might sound quite obvious, but these generalized considerations are the most effective if one wants to stay safe.
The most common-sense recommendation would be the following: do not engage in recreational use of benzodiazepines. Only use benzodiazepines if you have a legitimate prescription and, if so, only take them strictly following your prescription’s instructions.
Anyone considering benzodiazepine use would do well to think long and hard about the possible negative effects. Can the possible adverse effects cause more harm than good? Before jumping into benzodiazepine use, consider all available options and alternatives.
There are plenty of non-pharmacological options that can achieve great success. For example, behavior-related solutions like therapy, exercise, and meditation yield tremendous benefits.
Herbs like kava, kratom, or cannabis may also be good alternatives.
Clobazam Drug Interactions
Some drugs should be studiously avoided if one is currently on benzodiazepines. Any and all CNS depressants could be fatally dangerous, but the two that stand out are opioids and alcohol. Recent trends in drug overdose deaths should be enough to convince anyone how dangerous these combinations can be.
The most dangerous drugs to mix with clobazam include alcohol, GHB, phenibut, phenobarbitol, or any of the opiate drugs.
However, in the world of prescription drugs, many other combinations often have to be avoided. The sheer number of drugs out there can make this very unwieldy, so it’s always smart to ask your doctor what you should avoid. When consulting with them, disclose all drugs and supplements you take regularly. At the very least, check what drugs are contraindicated to whatever benzodiazepine you plan on consuming.
Finally, users must be aware of the possibility of CYP drug interactions. Drugs that affect the CYP enzymes might also be responsible for metabolizing benzodiazepine. Inhibiting said CYP enzymes could make drug metabolization less efficient, raising the potential for adverse effects. On the other hand, inducing the CYP enzyme associated with a given benzodiazepine could make the drug less efficient since it’s cleared from the body faster.
Clobazam Contraindications
All drugs have certain contraindications. Users unaware of what is contraindicated for a given benzodiazepine could put themselves in serious danger without knowing. Most contraindications are related to age groups and special statuses like pregnancy or the operating of heavy machinery. However, esoteric drug interactions and the presence of certain conditions can also be contraindications. Always make sure to know what contraindications are present in the drugs you’re taking.
Clobazam Dosage
By sticking to the proper dosage for your indication and age group, users can do much to minimize their risk. If you’re unsure about the correct dosage, speak to your doctor.
Note: The recreational doses of clobazam are usually much higher than the medical doses. It’s wise to never exceed a dose of 50 mg.
The Mayo Clinic has identified the following dosages for clobazam (oral):
Adults and children 2 years of age and older weighing more than 66 lb (30 kg) — The dose is based on body weight and must be determined by your doctor. The starting dose is usually 10 mg per day, given as two divided doses. Your doctor may adjust your dose as needed. However, the dose is usually not more than 40 mg per day.
Adults and children 2 years of age and older weighing 66 lb (30 kg) or less — The dose is based on body weight and must be determined by your doctor. The starting dose is usually 5 mg as a single dose per day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 20 mg per day.
Older adults — The dose is based on body weight and must be determined by your doctor. The starting dose is usually 5 mg as a single dose per day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 40 mg per day.
Children younger than 2 years of age — Use and dose must be determined by your doctor.
Similar Benzodiazepines
There are literally hundreds of benzodiazepine compounds on the market today. Most of them share a similar core effect profile — offering powerful anxiolytic and sedative actions. However, each one has a slightly different character from the next.
Clonazepam (Klonopin)
Clonazepam (Klonopin) is considered the closest (and usually preferred) alternative to clobazam. It’s used medicinally for treating seizures and insomnia, and recreational for i’s “MDMA-like” effects on mood. Klonopin has a different mechanism of action than clobazam but is similar in that it also differs slightly from traditional benzodiazepines.
Arfendazam
Arfendazam is the benzodiazepine most similar to clobazam. They have a similar chemical structure as well as a comparable pharmacological profile. However, arfendazam is considered milder and less euphoric.
Natural Alternatives to Clobazam
There are plenty of plant-based options to try if a user does not want to expose themselves to the risks inherent in prescription benzodiazepine use.
Recently, the kava plant has garnered a reputation for being able to induce states of calm and even sedation. These pharmacological properties are confirmed by peer-reviewed studies [10]. What’s more, the adverse effects of kava are far more benign than any pharmacological option. However, it is not a viable replacement for clobazam as it does not have anticonvulsant effects.
Users could also consider the kratom plant. This option is slightly more controversial as it carries certain risks due to its interactions with the body’s opioid receptors. However, in reality, the only real risks stem from concomitant use with other CNS depressants and misuse; fatalities caused by only consuming kratom are almost non-existent.
The kratom plant has a wide range of pharmacological benefits. It can produce stimulating and euphoric effects in low doses and anxiolytic and sedating benefits in mid-to-high doses [11].
References
- Poisbeau, P., Gazzo, G., & Calvel, L. (2018). Anxiolytics targeting GABAA receptors: Insights on etifoxine. The World Journal of Biological Psychiatry, 19(sup1), S36-S45.
- Doi, T., Ueda, Y., Tokumaru, J., & Willmore, L. J. (2005). Molecular regulation of glutamate and GABA transporter proteins by clobazam during epileptogenesis in Fe+++-induced epileptic rats. Molecular brain research, 142(2), 91-96.
- Sankar, R. (2012). GABAA receptor physiology and its relationship to the mechanism of action of the 1, 5-benzodiazepine clobazam. CNS drugs, 26(3), 229-244.
- Jensen, H. S., Nichol, K., Lee, D., & Ebert, B. (2014). Clobazam and its active metabolite N-desmethylclobazam display significantly greater affinities for α2-versus α1-GABAA–receptor complexes. PLoS One, 9(2), e88456.
- Gauthier, A. C., & Mattson, R. H. (2015). Clobazam: a safe, efficacious, and newly rediscovered therapeutic for epilepsy. CNS neuroscience & therapeutics, 21(7), 543-548.
- Ertam, I., Sezgin, A. O., & Unal, I. (2009). A case with Stevens Johnson syndrome triggered by combination of clobazam, lamotrigine, and valproic acid treatment. International journal of dermatology, 48(1), 98-99.
- Riss, J., Cloyd, J., Gates, J., & Collins, S. (2008). Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta neurologica scandinavica, 118(2), 69-86.
- Tolbert, D., Harris, S. I., Bekersky, I., Lee, D., & Isojarvi, J. (2014). Withdrawal-related adverse events from clinical trials of clobazam in Lennox–Gastaut syndrome. Epilepsy & Behavior, 37, 11-15.
- Isojärvi, J. I., & Tokola, R. A. (1998). Benzodiazepines in the treatment of epilepsy in people with intellectual disability. Journal of intellectual disability research: JIDR, 42, 80-92.
- Cairney, S., Clough, A. R., Maruff, P., Collie, A., Currie, B. J., & Currie, J. (2003). Saccade and cognitive function in chronic kava users. Neuropsychopharmacology, 28(2), 389-396.
- Swogger, M. T., & Walsh, Z. (2018). Kratom use and mental health: A systematic review. Drug and Alcohol Dependence, 183, 134-140.