Metaclazepam (Talis) Fact Sheet: Dosage, Safety, & List of Natural Alternatives
Metaclazepam, sold under the brand name Talis, is a benzodiazepine drug used as both an anxiolytic and muscle-relaxant.
The active form of metaclazepam is another compound known as N-desmethylmetaclazepam.
Talis, and generic forms of metaclazepam are designed to kick in quickly and last several hours. This drug requires several rounds of metabolization via the liver to deactivate it. Several metabolites formed during the drug’s breakdown remain active on the benzodiazepine (GABA-A) receptors.
Metaclazepam is considered an intermediate-acting 1,4-benzodiazepine. The total duration of effects lasts between 6 and 12 hours total.
Metaclazepam Specs
| Status | Approved 💊 |
| Common Dosage | 5–20 mg |
| PubChem ID | 71272 |
| CAS# | 84031-17-4 |
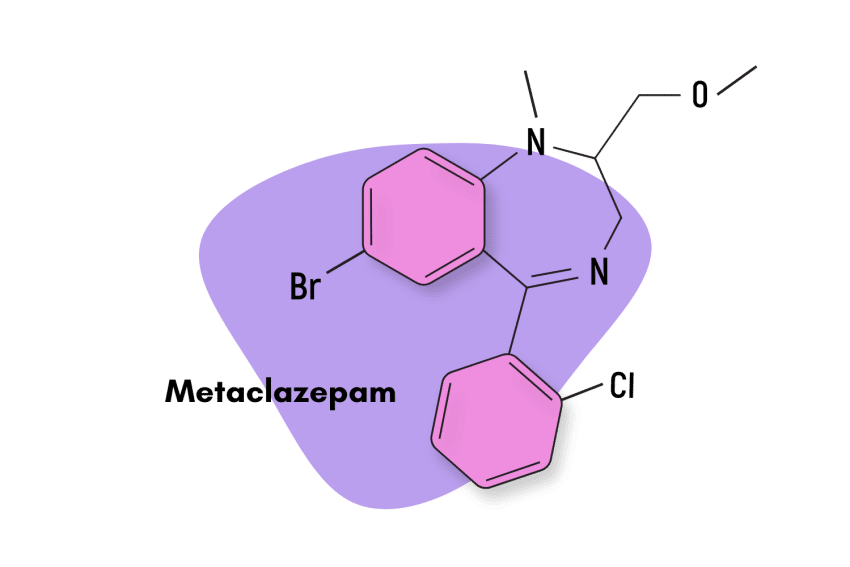
IUPAC Name: 7-Bromo-5-(o-chlorophenyl)-2,3-dihydro-2-(methoxymethyl)-1-methyl-1H-1,4-benzodiazepine
Other Names: Talis, Brometazepam, Metaclazepamum
Metabolism
Metaclazepem is metabolized in the liver by the process of demethylation into an active metabolite known as N-desmethylmetaclazepam [3].
Duration of Effects
The drug starts to show its action at around 30 to 60 minutes of drug intake. The peak concentration was obtained around 2 hours after the drug’s intake, and the drug’s half-life was found to be around 20 hours [4].
What is the Dose of Metaclazepam?
The recommended dose for metaclazepam is 15 mg per day. The dose can be taken as 5 mg in the morning and 10 mg in the evening, or 15 mg once a day. The dose can be increased to 30 mg per day. The side effect profile increases as the dose increases and can cause sedation and breathing problems [4].
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Metaclazepam Work?
Metaclazepam, like most other benzodiazepines, works by increasing the action potential of the nerve cells. This slows down the transmission of messages around the brain, resulting in fewer thoughts, reduced anxiety levels, and feelings of calmness and relaxation.
This same effect dulls electrical signals in the muscles, causing them to relax as well.
Benzodiazepines like metaclazepam achieve this by binding to a special receptor located on the neurons, aptly named the ‘benzodiazepine receptors.’
Once bound, benzodiazepines alter the shape of the receptor to become more sensitive to a neurotransmitter called GABA.
GABA is the body’s natural inhibitory messenger — it acts as the brake pedal for the brain, causing everything to slow down when we become too excited or anxious. It also helps to slow us down in the evenings when it’s time to wind down for bed.
Is Metaclazepam Safe? Risks & Side Effects
There are two major risks regarding the use of metaclazepam (as well as benzodiazepines in general).
The first major risk is overdose — which is uncommon when used responsibly. However, the risk of overdose increases dramatically when combined with other drugs or medications, especially those with sedative effects. Mixing benzos with alcohol, GHB, phenibut, barbiturates, opiates, or other benzodiazepines is extremely dangerous. The vast majority of overdose cases involving benzos involved more than one drug.
The second major risk to be aware of is the potential for addiction. Repeated benzodiazepine use results in tolerance formation in a relatively short period of time (2–5 weeks). As tolerance forms, users require higher doses of the drug to achieve the target effects. Additionally, as the effects of the drug wear off, users experience withdrawal symptoms, which often mimic the very effects the drug was designed to treat. This includes anxiety, insomnia, muscle tension, and seizures (in more severe cases).
Common Side Effects of Metaclazepam
The most common side effect of metaclazepam is sedation and fatigue. Other common side effects include disinhibition, amnesia, nausea, low blood pressure, and muscle weakness.
Serious side effects of metaclazepam are rare but may include the following:
- Severe hypotension and fainting
- Cardiac arrhythmia
- Temporary cessation of breathing while sleeping
- Respiratory depression and slow breathing
- Blurring of vision
- Confusion
- Psychotic symptoms like hallucinations and delusions
- Depression and suicidal thoughts
- Signs of liver injury, such as jaundice and loss of appetite
- Signs of anaphylaxis
Harm Reduction: Metaclazepam
Like other benzodiazepines, metaclazepam carries a high risk for abuse.
Here are some tips and tricks for staying safe while using benzodiazepine drugs:
- 🥣 Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- ⏳ Take frequent breaks or plan for a short treatment span — Benzodiazepines can form dependence quickly, so it’s important to stop using the drug periodically.
- 🥄 Always stick to the proper dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- 💊 Be aware of contraindications — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- 🧪 Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- 💉 Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- 🌧 Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- ⚖️ Understand the laws where you live — In most parts of the world, benzodiazepines are only considered legal if given a prescription by a medical doctor.
- 📞 Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Look up “addiction hotline” for more information where you live. (USA: 1-800-662-4357; Canada: 1-866-585-0445; UK: 0300-999-1212).
Similar Benzodiazepine Alternatives
The most common benzodiazepines used today include alprazolam (Xanax), bromazepam (Lectopam), diazepam (Valium), chlordiazepoxide (Librium), and clonazepam (Klonopin).
Designer benzos (not approved) include etizolam, flubromazepam, phenazepam, and pyrazolam.
Metaclazepam vs. Other Short To Intermediate-Acting Benzodiazepines [4,6]:
| Metaclazepam | Alprazolam | Bromazepam | Diazepam | Chlordiazepoxide | |
| Chemical composition | 1,4-Benzodiazepine | Triazolobenzodiazepine | 1,4-benzodiazepine | 1,4-benzodiazepine | 1,4-benzodiazepine |
| Route of administration | Oral | Oral | Oral | Oral, IV, IM | Oral, IV |
| Onset of action | 30 to 60 minutes | 30 to 60 minutes | 60 minutes | 15 to 60 minutes | 1 to 2 hours (oral) |
| Peak concentration | 1 to 2 hours | 1 to 2 hours | 1 to 4 hours | 1 to 1.5 hours | 2 hours |
| Duration of effects | Intermediate-acting (12-20 hours) | Short-acting (6 to 27 hours) | Intermediate-acting (8 to 9 hours) | Long-acting (20 to 80 hours) | Long-acting (36 to 200 hours) |
| Mechanism of action | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist |
| Medical Uses | Panic disorders, anxiety disorders | Panic disorders, anxiety disorders, insomnia | Anxiety disorder, alcohol withdrawal | Seizures, alcohol withdrawal, insomnia, muscle spasms, panic disorder, anxiety disorders | Panic disorders, alcohol withdrawal, anxiety disorders |
Natural Alternatives To Benzodiazepines
There are a handful of naturally-occurring plants and nutrients that can act like benzodiazepines — albeit much milder overall.
These substances may serve as a viable alternative to benzos in people who require long-term support or have had problems with addiction in the past.
It’s important to note that neither benzodiazepines nor herbal alternatives can treat the root cause of anxiety or insomnia and merely offer symptomatic support. Sufficient treatment involves identifying and addressing the underlying cause of the disorder rather than relying on crutches.
Kava
Kava (Piper methysticum) is a rhizome found on various islands in the Pacific Ocean, including Fiji, Vanuatu, and Hawaii. It’s used in much the same way as benzodiazepine drugs for managing anxiety and insomnia.
The effects of kava are similar to benzodiazepines but much milder (and safer). It’s a great option for people to try before using benzodiazepines or as a tool to help manage withdrawal symptoms while quitting (under medical supervision, of course).
A meta-analysis also showed that kava is effective for treating anxiety, with only mild side effects noted, such as headache and drowsiness [7].
Lavender
A study has shown that lavender essential oil is effective in the treatment of anxiety, depression, sleep disorders, and symptoms associated with alcohol withdrawal [9]. It works through similar mechanisms as benzodiazepines by modulating the GABA receptors.
Valerian Root
Valerian root contains a slurry of GABAergic active ingredients that mimic the effects of benzodiazepines [10]. This plant is very strong, but don’t expect it to match the intensity of pharmaceutical benzodiazepines. This herb serves as a gentler, non-addictive alternative to benzodiazepine medications.
GABA Supplements
GABA itself can be supplemented too. These supplements can support natural GABA levels in the brain, but it won’t induce the same powerful changes exerted by synthetic benzodiazepine drugs.
GABA supplements are useful for gently supporting chronic anxiety and insomnia but may not be strong enough for more serious cases.
This may be explained by the fact that oral supplements of GABA cannot cross the blood-brain barrier (BBB) [11]. It’s likely that GABA must first be broken down into its precursors and then reassembled in the brain.
Chamomile
Chamomile tea is a traditional tea made from chamomile flowers, which is gaining popularity for its soothing effects and other health benefits. It has been hypothesized that the tea works by binding to the benzodiazepine receptor and increasing the activity of GABA [12].
Metaclazepam FAQ
1. What are the benefits of metaclazepam over other benzodiazepines?
The main benefit of metaclazepam over other benzodiazepines is the absence of serious cardiovascular side effects. This may make metaclazepam a better alternative for cardiocompromised patients or elderly patients.
Metaclazepam was found to be equally effective as commonly used benzodiazepines such as diazepam (Valium) and bromazepam (Lectopam), but with a lower risk of side effects.
2. Which foods should I avoid while taking metaclazepam?
It’s wise to avoid foods that interact with liver metabolism, such as grapefruit while taking metaclazepam. Alcohol and caffeine should also be avoided.
3. Can I take metaclazepam if I am taking another benzodiazepine?
No, it is not advised to take metaclazepam if you are taking other benzodiazepines unless following the recommendation of a medical doctor.
References
- Buschmann, G., Kühl, U. G., & Rohte, O. (1985). General pharmacology of the anxiolytic compound metaclazepam in comparison to other benzodiazepines. Arzneimittel-forschung, 35(11), 1643-1655.
- Marano, P., Patti, F., & Nicoletti, F. (1988). A controlled study on the anxiolytic activity of a newly-developed benzodiazepine, metaclazepam. Current Medical Research and Opinion, 11(1), 41-44.
- Borchers, F., Achtert, G., Hausleiter, H. J., & Zeugner, H. (1984). Metabolism and pharmacokinetics of metaclazepam (Talis®), Part III: Determination of the chemical structure of metabolites in dogs, rabbits, and men. European journal of drug metabolism and pharmacokinetics, 9(4), 325-346.
- Gielsdorf, W., Molz, K. H., Hausleiter, H. J., Achtert, G., & Philipp, P. (1986). Pharmacokinetic profile of metaclazepam (Talis®), a new 1.4-benzodiazepine. European journal of drug metabolism and pharmacokinetics, 11(3), 205-210.
- Laakmann, G., Treusch, J., Schmauss, M., Schmitt, E., & Treusch, U. (1982). Comparison of growth hormone stimulation induced by desipramine, diazepam, and metaclazepam in man. Psychoneuroendocrinology, 7(2-3), 141-146.
- Griffin, C. E., Kaye, A. M., Bueno, F. R., & Kaye, A. D. (2013). Benzodiazepine pharmacology and central nervous system–mediated effects. Ochsner Journal, 13(2), 214-223.
- Pittler, M. H., & Ernst, E. (2003). Kava extract versus placebo for treating anxiety. Cochrane Database of Systematic Reviews, (1).
- Suyono, H., Jong, F. X., & Wijaya, S. (2020). Lavender, cedarwood, and vetiver balm work as anti-stress treatment by reducing plasma cortisol levels. Rec. Nat. Prod, 8, 10-12.
- Kasper, S. (2013). An orally administered Lavandula oil preparation (Silexan) for anxiety disorder and related conditions: an evidence-based review. International journal of psychiatry in clinical practice, 17(sup1), 15-22.
- Shinjyo, N., Waddell, G., & Green, J. (2020). Valerian root in treating sleep problems and associated disorders—A systematic review and meta-analysis. Journal of Evidence-Based Integrative Medicine, 25, 2515690X20967323.
- Boonstra, E., De Kleijn, R., Colzato, L. S., Alkemade, A., Forstmann, B. U., & Nieuwenhuis, S. (2015). Neurotransmitters as food supplements: the effects of GABA on brain and behavior. Frontiers in Psychology, 1520.
- Mao, J. J., Li, Q. S., Soeller, I., Rockwell, K., Xie, S. X., & Amsterdam, J. D. (2014). Long-term chamomile therapy of generalized anxiety disorder: A study protocol for a randomized, double-blind, placebo-controlled trial. Journal of clinical trials, 4(5).
- Akhondzadeh, S., Naghavi, H. R., Vazirani, M., Shayeganpour, A., Rashidi, H., & Khani, M. (2001). Passionflower in the treatment of generalized anxiety: A pilot double‐blind, randomized controlled trial with oxazepam. Journal of clinical pharmacy and therapeutics, 26(5), 363-367.