The Truth About Kratom & Your Kidneys
Some tout kratom as a miracle herb — others call it a deadly, organ-damaging drug. Today, we’ll find the truth to one question… Does kratom cause kidney damage?

Some people suggest and even report from personal experience, that kratom — a tropical tree from Southeast Asia with close relations to the coffee plant — causes kidney damage.
Others vehemently deny this possibility, accusing these people of lying or fearmongering.
How could such an incredibly important topic be the subject of such disagreement and debate?
We examine the claim that kratom causes kidney damage and look at the available evidence. We will also cite some anecdotal reports from survivors of people who believe their kidney injuries are the result of kratom.
How Does Kratom Affect the Kidneys?
Asking how any plant affects a single organ is a loaded question. The body is a holistic, integrated system. Influencing one organ’s function can create a cascade effect, altering the output of hormones or enzymes in an entirely different organ, which can influence all the organs reliant on those enzymes, and so on.
The holistic approach to science and medicine is based on the recognition that anything that creates change in a specific part of the body influences the entire system, one way or another. As such, there are many ways that kratom affects the kidneys, both directly and indirectly.
To get a full understanding of the potential risk of renal toxicity, you need to know how kratom impacts various bodily systems that, in turn, affect the kidneys.
Kratom: A Pharmacological Enigma
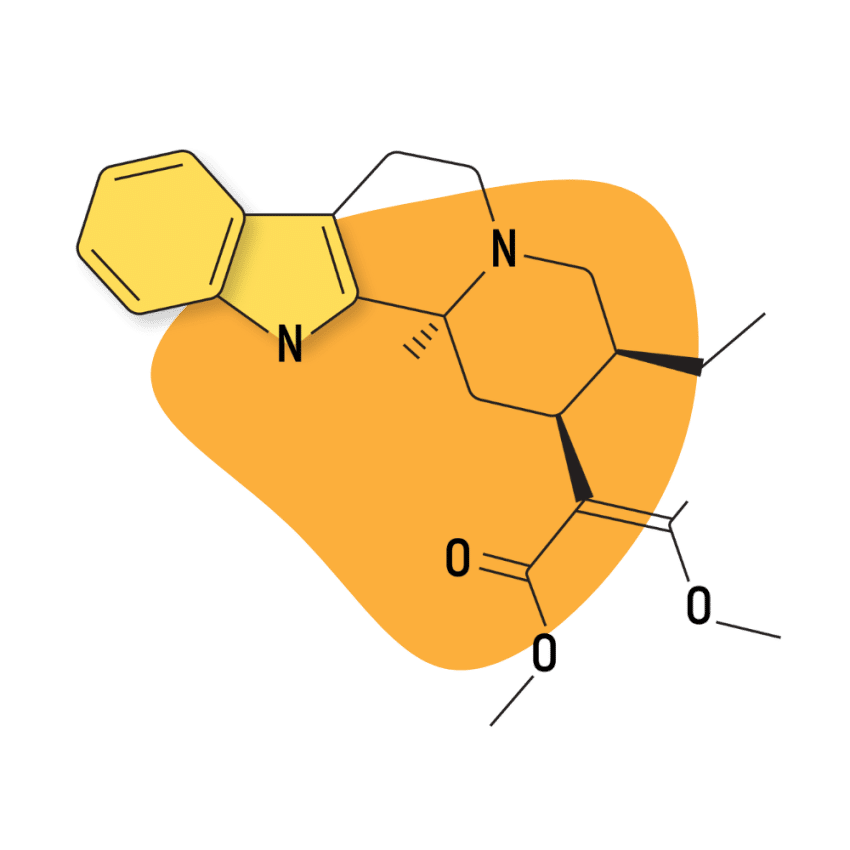
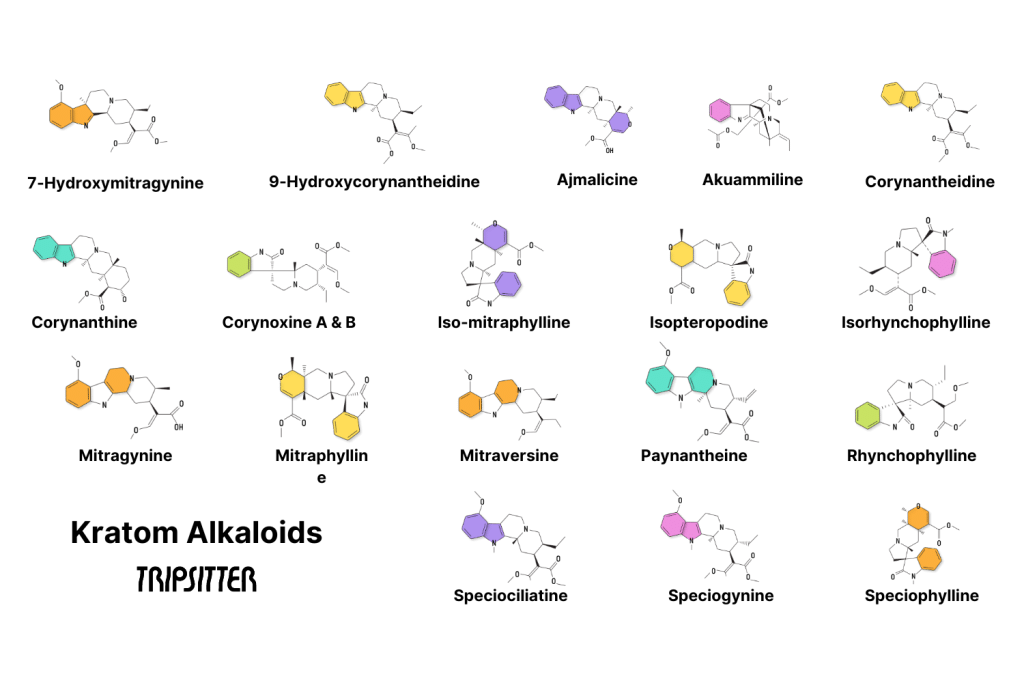
Researchers haven’t pinpointed the exact nature and severity of kratom’s effect on the renal system partly because kratom has so many biological effects due to its many different active alkaloids.
For example, mitragynine acts on more than half a dozen different bodily systems. It targets all three different opioid receptor subtypes and influences serotonin, dopamine, and adrenaline, as well as many of the hormones produced by the hypothalamic-pituitary-adrenal axis [1].
That’s a lot of different systems. And guess what? All of these systems interact with the kidneys.
To briefly touch on the scale of complexity we’re talking about here:
- The intrarenal dopamine system (yes, our kidneys have their own dopaminergic transmission system) is highly involved in regulating blood pressure and is possibly linked to hypertension (high blood pressure) [2].
- Serotonin is a powerful renal vasoconstrictor. In addition to regulating metabolism and glomerular function in the kidneys, serotonin controls the flow of blood in and out of the renal system. Since kratom affects both dopamine and serotonin, both of which are involved in controlling blood flow to the kidneys, this could spell a dangerous situation [3].
- Mu opioid receptors found in the kidneys regulate its function [4].
- The kappa opioid receptors help regulate the flow of fluid and electrolytes through the kidneys and out of the body (in rats, at least) [5].
- Delta opioid receptors are not intrinsically influential in renal function. However, they have been shown to produce significant changes in the kidney’s ability to excrete and process waste when they are activated through the use of external substances [7].
- The adrenaline glands sit right atop your kidneys. Anything that influences the production or distribution of adrenaline will affect your kidneys.
- The hypothalamic-pituitary axis is responsible for producing numerous hormones. Deficiencies or disorders of the axis tend to be associated with increased risk or worsening severity of kidney disease [8].
This is just scratching the surface of the pharmacological interactions of one of the dozens of alkaloids found in kratom. It’s no wonder that there’s very little conclusive evidence.
Is There Evidence That Kratom Damages the Kidneys?
Unfortunately, yes. There is enough evidence to suspect that using excessive amounts of kratom long-term may cause damage to the kidneys.
There’s more evidence to suggest that it can indirectly damage the kidneys by impairing the function of other organs. However, these cases are far from the norm, and many of the studies follow questionable methods or are blatantly sensationalized.
Not all of them are, though. Some of them are just plain, old, incriminating evidence that kratom does bad stuff to your little bean-shaped blood filters. We’ll start with those ones to get the unpleasantries out of the way first before moving forward to explain why some studies aren’t really a good example of kratom’s overall impact on your kidneys and health.
1. Renal Impact of Kratom-Induced Liver Damage
A couple of studies seem to suggest that kratom damages the liver, but some of these studies are guilty of using unjust, determinative wording when evidence is not sufficient. Banyan Treatment Center, which claims that kratom “absolutely” damages the liver, makes an embarrassing attempt to summarize such studies [9].
Let us first state that they blatantly butchered just about every aspect of the study that they’re referencing, and it’s really a shame that people rely on this site for information.
They state that “a 47-year old male with no history of drug use experienced symptoms of lethargy, abnormal liver tests, and pruritis after drinking kratom tea for 21 days. He was ultimately diagnosed with drug-induced liver disease as a result.”
Then, they reference the study. It states clearly that a 31-year-old man — not a 47-year-old one, so we’re already off to a bad start regarding accuracy — used kratom for 2 weeks in order to treat opioid withdrawal. Hey Banyan, weren’t you going to note that this fellow was already physically dependent on opioids? And two weeks is not quite 21 days [10].
The rest of what they’ve mentioned is true enough. His liver tests were abnormal; there were elevated levels of bilirubin and numerous other enzymes. However, the study makes mention of the patient’s “prior medical history” as if to suggest he was tested recently and consistently throughout his opioid addiction. The table states his previous liver test was 10 months prior.
Either way, he was diagnosed with drug-induced hepatotoxicity. But they don’t specify whether that was because of the kratom, the opioid addiction, or both. Banyan seems to pin it all on kratom and avoids acknowledging the heavy physical addiction to an unnamed opioid.
So, is it likely that kratom aggravated his liver enzymes? Absolutely! It’s almost a certainty. But is it possible that this fellow’s habit of unspecified opioids (which could mean anything from codeine to oxycodone to heroin laced with fentanyl) for up to 10 months could have also impacted his liver enzymes? Absolutely! It’s somewhat fishy that the study doesn’t mention this.
(For what it’s worth, in my personal experience, having worked with dozens of kratom users and recovering opioid addicts, people tend to come to kratom when they’re fairly desperate, which suggests a serious opioid habit.)
The study doesn’t actually state specifically that kratom caused the liver injury, although it does seem to be aggressively suggesting that it did. What they do mention, however, is that the damage was reversed easily with time and abstinence alone.
Sub-Chronic Administration of Mitragynine & Renal/Hematological Toxicity
Another study evaluated the sub-chronic administration of mitragynine in rats. The mitragynine was used in its isolated state, extracted from leaves and providing a clear pharmacological profile of this single alkaloid [11].
The study revealed that in sub-chronic low dosing periods, kratom is relatively safe, showing no signs of toxicity at the low dosage range (between 1-10 mg/kg). However, when the dose is increased to the upper range (~100 mg/kg) various signs of toxicity emerge.
Hematological, biochemical, and histopathological effects were all evident. However, there is no evidence that this damage was permanent, and the researchers recommended a longer 90-day follow-up to assess the possible reversal of damage.
Multiorgan Dysfunction Related to Kratom Ingestion
This is another study with a slammer of a title. It’s based mostly on the experience of a 37-year-old woman who had used “kratom-containing herbal supplements” for “prolonged” periods. Her symptoms were acute liver injury, acute kidney injury and pancolitis [12].
The study acknowledges that this is an atypical case and, “to the best of our knowledge, this is the first description of multiorgan dysfunction in the setting of prolonged kratom ingestion.” So, at least, we can see that this study is fairly stable in its claims.
After several tests, the woman was diagnosed with kidney injury that worsened with hospitalization, eventually requiring renal replacement therapy for anuria. It should be noted that she also took dextroamphetamine for ADHD.
2. General Opioid Use & Liver/Kidney Damage
Studies have shown, at least in animal models, that opioid use itself can be a factor in the degradation of liver and kidney health. One such study evaluated the impact of giving rats a dose of morphine increased every 10 days for a total of 30 days. They were given 4, 8, and then 10 mg/kg daily [13].
Note that this is a massive dose, and it’s somewhat surprising that it didn’t kill them. The equivalent dose for a 70 kg person would begin at 280 mg daily, intravenous, eventually leading up to 700 mg daily. The FDA considers people “morphine tolerant” at 60 mg/day total for a week. (Although no kratom habit could reach this level, the mechanisms are nonetheless important to consider).
Researchers took liver samples after the study and evaluated a host of liver enzymes and other compounds [14].
They observed severe centrilobular congestion and focal necrosis in the liver of the rats on opiates, necrosis being present only in the morphine group. Tubular cells were vacuolized. There was a significant increase in aminotransferase, aspartate aminotransferase, lactate dehydrogenase, and malondialdehyde. MDA was also high in the morphine group.
This suggests that opioids increase the rate of lipid peroxidation, as well as directly cause organ damage to the kidney and liver when used extensively over long periods. This is interesting as this isn’t something commonly stated by drug awareness groups or even by the FDA/DEA, perhaps because the doses in this study are so absurd.
Related: Is Kratom an Opiate?
Why Don’t Experts Agree on Kratom’s Health Issues?
Scientists (and, by proxy in a science-based society, pretty much everyone) point to clinical trials as the pinnacle of unbiased evidence because they are, in theory, objective. In theory, this type of testing can verify other theories without skewing the results via personal bias.
When multiple tests by different researchers provide the same results, we strengthen the link between cause and effect. A one-off study with a small sample size (a small number of participants) that concludes a plant (like kratom) might be harmful (to the kidneys) is not considered hard evidence.
Neither are case studies considered hard evidence unless there are a statistically significant number of them. Case studies are individual medical evaluations of patients admitted with conditions that might be linked to a certain substance. A good deal of the ‘evidence’ for kratom damaging the kidneys is due to case studies.
Not everyone knows this, though. In fact, it’s easy enough to recognize that the majority of the population has no clue how scientific evidence is deduced nor how to verify it themselves. On top of this, politics and science are becoming unhealthily intertwined. Wealthy corporations are funding studies that conveniently produce results in their favor.
Leading scientists and researchers express displeasure at modern political leaders manipulating, misrepresenting, or flat-out falsifying scientific data to pursue a certain agenda.
There are many different arms of the scientific establishment, but many would agree that the pharmaceutical sector is the most politically driven. That the medical industry eschews patient safety and medicinal efficacy for profit and personal gain is nothing new [15,16].
And kratom is a very hot topic in the medical world because of its potential to be both disruptive and life-saving. It could single-handedly
1. Financial Motivations Prevent Proper Research
The pharmaceutical industry is among the largest in the world. Most of the global population contributes to it. So, it’s no wonder that people are quick to suspect the pharmaceutical industry as being responsible for the misunderstanding of kratom.
As mentioned, many people use kratom to get off of harder drugs. This is basically identical in practice as a treatment that the medical industry calls medication-assisted treatment. Just as with kratom, patients are given doses of opiates to “relieve themselves of withdrawal symptoms.”
More-or-less, they’re receiving a government-approved fix of the drug they’re addicted to. This allows them to build their lives back up. In theory, you’re supposed to be weaned off of the drugs after the minimal amount of time that it takes to find stability, but in practice, many people end up more addicted to the maintenance drugs and end up taking them for their whole lives [17].
The general consensus is that Big Pharma is afraid that they will lose tons of money if patients start using kratom and then simply stop. And this is likely true to some degree. Since most plant and drug research is funded by Big Pharma, they’ll only do so if they have a financial incentive to. This means no Big Pharma-funded studies are going to focus on kratom’s benefits [18].
2. Lack of Understanding, Lack of Transparency
There are, however, lots of case studies and reviews describing its negative effects, as well as obfuscating results to make them seem worse than they are. It may not be obvious to the untrained eye, but the wording of studies hugely impacts their interpretation. This is especially true among the laymen of our society, most of whom don’t read scientific journals to pass the time.
It’s incredibly important to assess the quality of studies. But how can you do that? Therein lies the major issue with the clinical trials associated with kratom — among many other supplements, healthy herbs, and drugs. Furthermore, a lot of the evidence base is drawn from case studies (evaluations of specific, often anomalous, medical cases), not actual tests.
Most people don’t know how to run the tests or use the equipment involved in clinical trials, nor could they set up a proper double-blind study. They will blindly (ha) assume that any studies published in scientific journals are inherently legit because they were done by professional researchers.
And that’s the elephant in the room, the big fat paradox that allows us to have our bank accounts ransacked by corrupted pharmaceutical corporations continually. Most of us can’t read the studies due to the complexity of the research involved.
Those who can often face another hurdle. Many studies are locked behind paywalls costing $40+ per paper. The scientific journals provide free access only to students enrolled in university programs. Students who are being instructed by the same type of researchers are responsible for the studies. This is not inherently bad but certainly sets up a foundation for massive bias.
The rest of us have to base our knowledge of medicine on these “objective and reproducible” studies that we can’t do ourselves. So we trust all the scientists who can do them to translate convoluted scientific knowledge like we trust priests to translate the word of God. However, if we’ve seen anything throughout history, the middle man often has his own agenda [19,20].
Instead, we base our understanding on the abstract or summary, as written by the study’s authors. Unfortunately, it’s relatively easy for authors to push the “conclusion” of a study in a certain direction. This section largely serves to explain how and why studies like the following one are published and proceed to confuse the public.
3. Example of a Misleading Study on Kratom Causing Kidney Damage
Let’s look at the first study that showed up in a Google search for “kratom and organ damage.” It’s a rat study entitled “Reversal of Hepatomegaly Following Cessation of Kratom Consumption in C57BL/6 Male and Female Mice” [21].
Already, we have a strong implication that kratom is directly responsible for liver injury. In this case, it’s certainly true, but the circumstances are not what normal kratom users would ever be exposed to.
The rats were put onto liquid diets — the study group rats were put on a liquid diet of kratom tea, and the control group was given a diet of water. That alone already separates the study results from just about every kratom user in the world because none of them subsist on anything but kratom tea.
The abstract, which is all a non-paying reader can look at, also leaves out a ton of information that is necessary to draw proper conclusions.
The study doesn’t mention whether or not the study rats got to drink regular water, for example. How would you feel if you drank nothing but strong kratom tea for two weeks without eating food or drinking water?
Why Proper Context Is Crucial
Generally, it takes dozens of trials, all of which need to draw similar conclusions, before the evidence is strong enough for researchers to use definitive terms like “kratom causes this,” or “kratom damages that.” At best, they may say that there is a link between the object of the study and a particular result.
In this case, they say: “Consumption of kratom in as few as 10 days causes hepatomegaly that can be reversed if kratom is discontinued.” Quoted out of context, this sentence alone can be disastrous for the reputation of kratom.
The amount of extreme dehydration that would result from drinking only kratom tea for ten days would surprise nobody if it straight up killed the rats, so it’s no surprise at all that they took some damage from it.
What’s more, is that the damage was later reversed when they stopped using kratom.
So, while the study was framed in a negative way that suggests “using kratom for a mere ten days can damage organs!” It could also have been framed in a way that said, “even when forced to consume absolutely nothing besides liquid kratom extract for ten days, rats quickly healed from secondary side effects.”
Unfortunately, studies like these lead to the creation of clickbaity articles like “Kratom Causes Organ Damage!” which now have only to cite this study as “scientific proof.” Suddenly, kratom takes a hit, and people start calling it “that herbal drug that scientists proved is destroying people’s organs.”
As we’ve discussed already, it’s pretty clear that there is some relationship between long-term, regular opioid use (yes, including kratom) and degraded kidney function. But nowhere near the degree, you’d expect if someone were held in a box and given only kratom tea for 10 days, suggesting that this sort of treatment is reflective of average kratom use is unprofessional.
Minimizing Kratom Damage to the Kidneys
The complexity of kratom makes it a tough job for the body to process. Imagine the whole process like a packing plant at the post office. Kratom is a huge, complicated shipment arriving from one source that needs to be separated into hundreds of individual packages that are then sent to several dozen different addresses.
The time and effort it takes for your body to break it into its individual parts, sort them, and then ship the alkaloids accurately to their proper destination is immense. Your body only has so many workers available at a time. If it gets overwhelmed, then it may repurpose enzymes or hormones from one task and redelegate them to help process the kratom more quickly.
1. Stay Hydrated & Get Your Electrolytes
When it comes to something that affects your kidneys, you want to make sure that they have the proper tools that they need to function. In the case of kratom use, that mostly means lots of fluids and electrolytes.
Staying hydrated ensures that your kidneys have a constant flow of liquid in and out so that they can properly flush the blood. When taking a diuretic like kratom, the kidneys excrete more urine so it’s important to stay hydrated. They also will expend more electrolytes during this process, so replenishing these, especially potassium, is incredibly important.
It’s rather interesting that kratom is linked to kidney damage since most herbal diuretics tend to be healthy for the kidneys. Dandelion, for example, provides numerous biological actions that work in tandem to enhance the health and function of the kidneys. It is, however, contraindicated in people who have pre-existing or a high risk of developing kidney ailments.
It’s also interesting that kratom is a diuretic at all. Most opioids tend to cause urinary retention as a side effect, not excretion [1].
Regardless, perhaps kratom is rich in electrolytes like other herbal diuretics. The studies, once again, hardly paint a conclusive picture of kratom and its interaction with the kidneys. Given the huge number of kratom users and the relatively low instances of kidney illness, we can assume that it’s something to be cautious of but not a guaranteed result from kratom use.
Related: List of All Common Kratom Side Effects
2. Decrease Your Kratom Use
Above all, though, your best bet is to reduce your kratom use. Yes, even more than you already have! The bottom line is that we don’t know how dangerous kratom is, but as the picture becomes clearer, it’s looking unpleasantly like kratom is more along the lines of tramadol than it is to something like codeine.
Final Thoughts: Kratom & Kidney Disease
Kratom is a beast of a plant with a huge number of biological actions. It has tremendous benefits but also presents significant risks. Using the plant without properly understanding the risks could be a recipe for disaster.
Although it’s very uncommon, kratom has been associated with kidney failure. It is also becoming more widely known that drugs targeting the opioid system seem to contribute to kidney and liver damage over time. In both cases, concomitant use of other substances significantly increases the risks.
Just as with other drugs and supplements, the risk of side effects can be diminished by taking proper care of your body. Staying hydrated and supporting your kidneys and liver with electrolytes, herbal supplements and a healthy diet is paramount to avoid any damage.
References
- Karunakaran, T., Ngew, K. Z., Zailan, A. A. D., Mian Jong, V. Y., & Abu Bakar, M. H. (2022). The chemical and pharmacological properties of mitragynine and its diastereomers: An insight review. Frontiers in Pharmacology, 13, 805986.
- Harris, R. C., & Zhang, M. Z. (2012). Dopamine, the kidney, and hypertension. Current hypertension reports, 14(2), 138-143.
- Kaur, G., & Krishan, P. (2020). Understanding Serotonin 5-HT 2A Receptors-Regulated Cellular and Molecular Mechanisms of Chronic Kidney Diseases. Renal Replacement Therapy, 6, 1-11.
- Kapusta, D. R., Jones, S. Y., & DiBONA, G. F. (1991). Renal mu-opioid receptor mechanisms in the regulation of renal function in rats. Journal of Pharmacology and Experimental Therapeutics, 258(1), 111-117.
- Ashton, N., Balment, R. J., & Blackburn, T. P. (1990). Kappa-opioid-receptor agonists modulate the renal excretion of water and electrolytes in anesthetized rats. British journal of pharmacology, 99(1), 181.
- Sezen, S. F., Kenigs, V. A., & Kapusta, D. R. (1998). Renal Excretory Responses Produced by the Delta Opioid Agonist, BW373U86, in Conscious Rats. Journal of Pharmacology and Experimental Therapeutics, 287(1), 238-245.
- Meuwese, C. L., & Carrero, J. J. (2013). Chronic kidney disease and hypothalamic–pituitary axis dysfunction: the chicken or the egg? Archives of medical research, 44(8), 591-600.
- Palmer, B. F., & Clegg, D. J. (2017). Gonadal dysfunction in chronic kidney disease. Reviews in Endocrine and Metabolic Disorders, 18, 117-130.
- Osborne, C. S., Overstreet, A. N., Rockey, D. C., & Schreiner, A. D. (2019). Drug-induced liver injury caused by kratom use as an alternative pain treatment amid an ongoing opioid epidemic. Journal of Investigative Medicine High Impact Case Reports, 7, 2324709619826167.
- Sabetghadam, A., Ramanathan, S., Sasidharan, S., & Mansor, S. M. (2013). Subchronic exposure to mitragynine, the principal alkaloid of Mitragyna speciosa, in rats. Journal of Ethnopharmacology, 146(3), 815-823.
- Khan, M. Z., Abou Saleh, M., Alkhayyat, M., Roberts, D. E., & Lindenmeyer, C. C. (2021). Multiorgan dysfunction related to kratom ingestion. ACG case reports journal, 8(8).
- Atici, S., Cinel, I., Cinel, L., Doruk, N., Eskandari, G., & Oral, U. (2005). Liver and kidney toxicity in chronic use of opioids: an experimental long-term treatment model. Journal of Biosciences, 30(2), 245-252.
- Hazani, H. M., Naina Mohamed, I., Muzaimi, M., Mohamed, W., Yahaya, M. F., Teoh, S. L., … & Kumar, J. (2022). Goofballing of Opioid and Methamphetamine: The Science Behind the Deadly Cocktail. Frontiers in Pharmacology, 1173.
- Aschner, M., Paoliello, M. M., Domingo, J. L., Spandidos, D. A., Mally, A., Wallace, H. M., … & Tsatsakis, A. (2020). When the boundaries between science and politics are blurred. Toxicology Reports, 7, 1607.
- Abraham, J. (2003). The science and politics of medicines control. Drug Safety, 26(3), 135-143.
- Frank, D., Mateu-Gelabert, P., Perlman, D. C., Walters, S. M., Curran, L., & Guarino, H. (2021). “It’s like ‘liquid handcuffs”: The effects of take-home dosing policies on Methadone Maintenance Treatment (MMT) patients’ lives. Harm Reduction Journal, 18(1), 1-10.
- Kodjak, A. (2016). Investors See Big Opportunities in Opioid Addiction Treatment. NPR.
- Lebied, M. (2018). Misleading Statistics Examples–Discover The Potential For Misuse of Statistics & Data In The Digital Age.
- Hoffmeier, J. K. (2015). Akhenaten and the Origins of Monotheism. Oxford University Press.
- Guenther, E., Musick, M., & Davis, T. (2019). Reversal of Hepatomegaly Following Cessation of Kratom Consumption in C57BL/6 Male and Female Mice. The FASEB Journal, 33(S1), 765-8.
- Guenther, E., Musick, M., & Davis, T. (2019). Reversal of Hepatomegaly Following Cessation of Kratom Consumption in C57BL/6 Male and Female Mice. The FASEB Journal, 33(S1), 765-8.