Ibogaine: A Powerful Anti-Addictive Psychedelic
Iboga is one of the best emerging treatments for addiction — but tread cautiously. This psychedelic isn’t for everybody.

It’s difficult to have a conversation around the use of psychedelics in addiction treatment without bringing up iboga — a traditional plant medicine from Central Africa.
This plant forces you to confront your deepest, darkest traumas and suppressed thoughts, bringing them to the surface where they can be integrated and healed.
But this doesn’t come without its fair share of risk.
Here, we’ll explore iboga, and its active ingredient, ibogaine, in more detail. You’ll learn how it’s used, how it works, and what you need to know before seeking treatment.
What is Ibogaine?
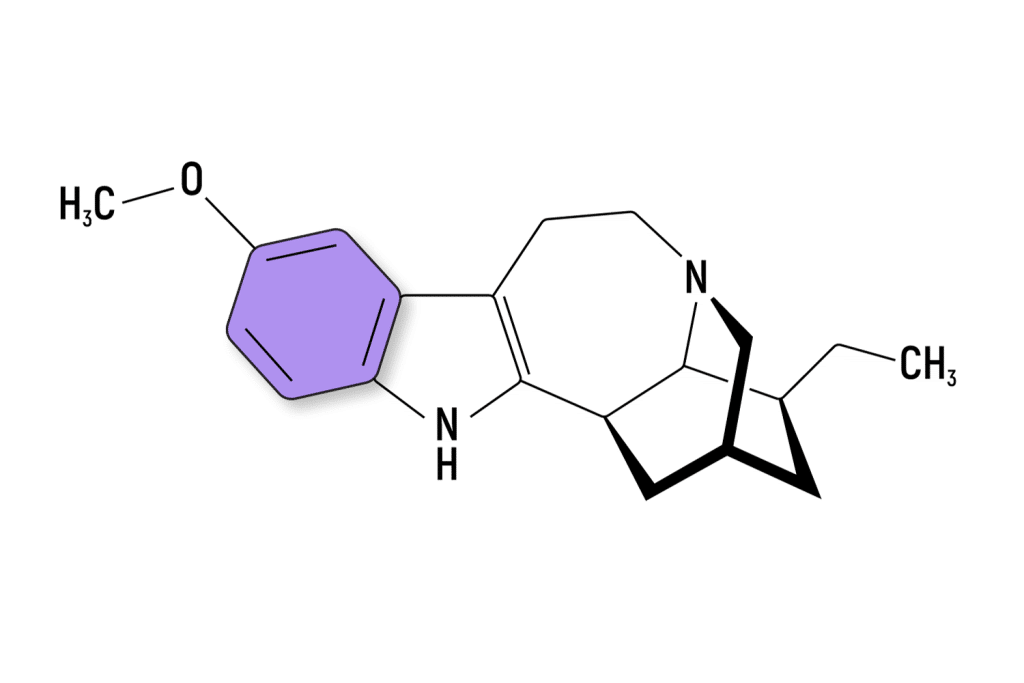
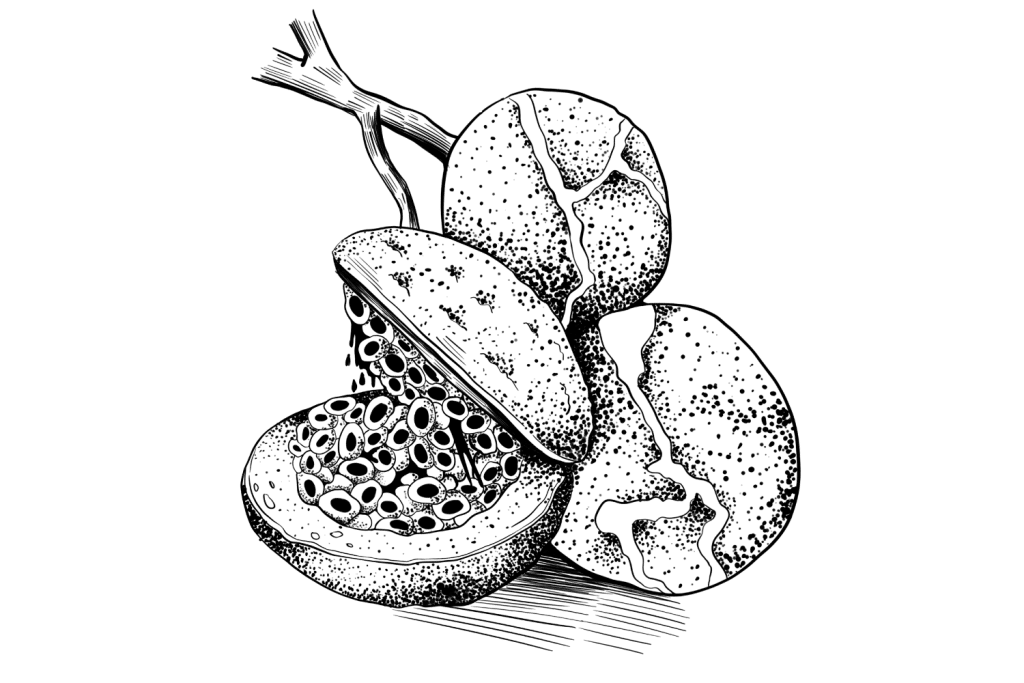
Ibogaine is a psychedelic alkaloid found in several species of plants in the Apocynaceae family. The most common species used is Tabernanthe iboga — a tropical shrub from the Congo.
Other species can also be used to obtain this alkaloid, including Voacanga africana and Tabernaemontana undulata. It can also be synthesized from its precursor compound, voacangine.
Ibogaine has a long history of use as an appetite suppressant and spiritual medicine. It was first discovered by the Pygmy tribes of Central Africa, who used the plant for spiritual and divination purposes.
It wasn’t until recently that ibogaine first made its debut as an anti-addiction medicine. This is now the most common application for the plant today.
Unfortunately, ibogaine brings some health risks that make it a less desirable psychedelic for addiction treatment than other substances like ayahuasca, 5-MeO-DMT, and ketamine — all of which have a much better safety profile.
Ibogaine: Specs & Technical Details
| Active Ingredients | Ibogaine |
| Level of Risk | Moderate-High |
| Most Common Side-Effects | Arrhythmias, nausea/vomiting |
| Duration of Effects | 8–24 hours |
| Legality | Illegal in most countries (Some exceptions) |
What Does Ibogaine Feel Like?
Ibogaine is a powerful psychedelic, dissociative, and oneirogenic (dream-inducing).
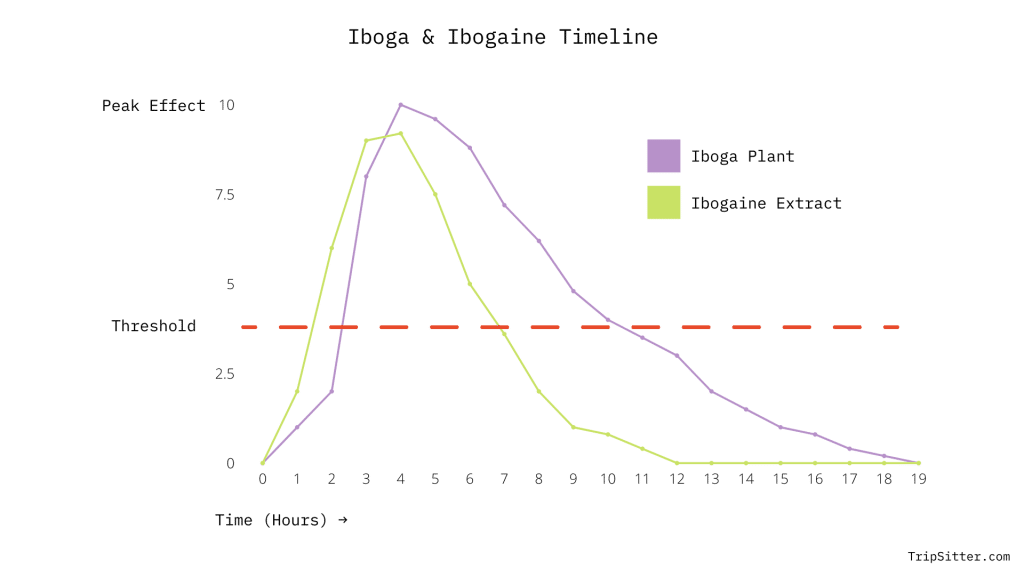
There are two different ways of using ibogaine — the raw root bark of the iboga plant and concentrated ibogaine. The iboga root contains 11 other alkaloids — many of which are thought to be biologically active on their own.
The effects of iboga root last longer and are much more likely to induce a spiritual experience than concentrated ibogaine.
With that said, both the iboga plant and ibogaine experience can be broken down into two phases — the visionary stage and the introspection phase.
1. The Visionary Stage
After taking ibogaine, you’ll need to wait between one and two hours before the effects start to kick in.
The experience begins gradually but intensifies over time. Users will start to experience visual distortions and geometric patterns that become more intense every minute.
Within about 30 minutes after the first onset of hallucinations, most users find themselves in a dreamlike state — this is the oneirogenic aspect of the experience. While you’re in the dream, the landscape could be your current environment or something entirely different.
This dream state is thought to dislodge unconscious thoughts and emotions in the form of a dream. The difference is that during this “waking dream,” you’re fully aware of what’s going on and able to retain the memory of it when the experience is over.
This effect is what makes ibogaine so powerful for facing trauma and internal struggles head-on. It forces you to face your shadow and explore the impacts traumatic events have had, or continue to have on your life.
This stage can be very uncomfortable. You may endure an ego-death experience, forcing you to explore parts of your psyche you normally try to suppress.
2. The Introspection Phase
Once the visionary stage starts to wear off, the introspective portion of the journey begins. This can happen anywhere from 4 to 8 hours after first taking ibogaine, or 10–24 hours if using the raw iboga plant.
During this stage, the mind processes the experience you just went through. Users are often filled with emotion, both good and bad, as they continue to process dislodged traumas and ego disillusionment.
This phase can last a long time. Some users report a maintained, semi-lucid, introspective state for up to 20 hours after taking ibogaine or 72 hours with the iboga plant.
During this stage, it’s important to be patient with yourself and others and ensure you have a safe and quiet space to sit with your thoughts alone. Some people find it helps to journal during this phase; others prefer to sit alone with their thoughts.
Even when this stage is over, users report having a higher capacity for introspection and self-exploration. Interestingly, users also report they need less sleep for up to two weeks after the session.
How Long Does Ibogaine Last?
The acute effects of concentrated ibogaine can last up to 8 hours, with an additional 10 hours of mild lucidity and deep introspection.
Iboga root bark lasts much longer — it’s not uncommon for the visionary stage to last a full 24 hours and the introspective stage an additional 48 hours.
Users should allow at least three days for an ibogaine session. One day beforehand to prepare (at least), one full day (24 hours) for the experience, and an additional day to recover and relax.
What’s the Dose of Ibogaine?
The dose of the root bark of the iboga plant can vary a lot. First of all, everyone’s physiology is unique, and several variables can alter the impact iboga alkaloids have on the body.
Secondly, the iboga root itself can vary. The alkaloid content may differ in one plant from another depending on the growing conditions, the region the plant was grown, and how it was harvested, stored, and prepared.
In general, the dose of iboga root is between 5 to 100 grams. This is a good example of why it’s so important to only use iboga under the care and supervision of an experienced practitioner who is intimately familiar with the dose of a particular sample of iboga.
The dose of ibogaine HCL is a little bit different. This concentrated alkaloid is much more consistent because there’s far less variability of the alkaloid itself — however, the variability of the individual still stands. The effective dosage range used in most clinical studies ranges from about 10 to 55 mg per kg of bodyweight.
Microdosing Ibogaine
Microdosing is the practice of taking sub-perceptual doses of a psychoactive substance. This dose is usually many times below the threshold dose — which is the minimum dose required to produce noticeable psychoactive effects.
There are people who microdose ibogaine and claim to have experienced a wide variety of benefits as a result. However, most iboga practitioners, both modern and traditional, don’t recommend microdosing this substance. Only those with a lot of experience using the plant and undergo regular medical visits to assess potential underlying risk (especially around cardiac function) should even consider microdosing iboga.
With that said, for the sake of thoroughness, the most common method people use iboga in microdoses is to prepare a tincture of the dried root bark of the Tabernanthe iboga shrub. The target dose is around 1g equivalent of a tincture. The amount of tincture you need to reach this dose depends on how concentrated the tincture is.

Is Ibogaine Legal?
As with any psychedelic substance, the legal status changes dramatically from one country to the next. While there are clear health benefits associated with ibogaine, there’s also some risk. Some countries completely ban the substance, others maintain it as a legal and useful medicine, and others keep ibogaine therapy open for research but restricted from the general public or clinical practice.
Ibogaine is illegal in the United States, with the exception of Oakland, California, and the state of Oregon.
In Canada, ibogaine is listed as a Natural Healthcare Product, which allows its use in approved medical centers as a form of treatment. There are several ibogaine therapy clinics in Canada. Recently, there’s been a push to reverse these laws and make ibogaine illegal over concerns of the potentially lethal side effects.
In Australia, ibogaine is classified as a Schedule IV substance — which means it can be distributed with a license. However, there has yet to be any licenses handed out for anything aside from research purposes.
Ibogaine is legal in Brazil, Mexico, South Africa, Gabon, New Zealand, the Netherlands, and Costa Rica.
Related: List of Legal Psychoactive Substances Around The World

Is Ibogaine Dangerous?
Ibogaine therapy isn’t without its risks. This psychedelic has a powerful therapeutic value but should be approached with caution and respect.
There have been cases of people dying from using ibogaine. The most common cause of death, by far, is heart failure.
This doesn’t happen just randomly — the majority of people experiencing lethal consequences from ibogaine have underlying heart disease or were using medications we now know are contraindicated with ibogaine.
Ibogaine should never be used without consulting with a medical professional first who can review your level of risk.
The simple solution to this is medical supervision. The Global Ibogaine Alliance recently set out some guidelines for providing treatment with ibogaine.
The criteria highlight several medical screening tests to explore potential complications from using ibogaine before treatment:
- Electrocardiogram test
- Thallium stress testing
- Complete metabolic panel (Chem 12 or Chem 18)
- Creatinine testing
- Full Blood Count (FBC)
- Thyroid function test
- Complete physical assessment
The Side Effects of Ibogaine
- Nausea & vomiting
- Ataxia (loss of muscle coordination)
- Sensitivity to light & sound
- Cardiac arrhythmias
Ibogaine Drug Interactions
One of the most dangerous aspects of ibogaine is its potential for negative interactions with other medications.
There are three different types of interactions a drug can have with ibogaine:
1. Metabolic Interactions
This happens when other substances or medications slow the liver’s ability to metabolize ibogaine, leading to increased duration and intensity of effects, which can be dangerous.
Ibogaine is metabolized primarily by the CYP2D6 enzymes, which is a common pathway for many substances, including tricyclic antidepressants, SSRIs, SNRIs, opioids, various antipsychotics, SERMs, class I antiarrhythmic medications, amphetamines, DXM, calcium channel blockers, and more.
Other substances that may inhibit the activity of this enzyme include CBD (cannabidiol), bupropion, quinine, and certain SSRIs.
2. Agonistic Interaction
These substances have an overlap in one or more of the effects ibogaine produces, which increases the risk for side effects from either substance.
Ibogaine causes changes in heart rhythm and blood pressure. This means there’s a strong potential for side effects with other substances that do the same thing — namely blood pressure medications and antiarrhythmic medications. The side effects of these substances can be lethal. Ibogaine is contraindicated for people taking medications for heart disease, stroke, or hypertension.
Vasoregulatory substances (AKA erectile dysfunction medications), such as Viagra, Cialis, Lovegra, or other PDE4 inhibitors, should also be avoided as well due to their overlapping effects on regulating blood flow.
Other potential agonistic interactions include medications that interact with serotonin or dopamine. Taking these compounds, like SSRIs, SNRIs, MAOIs, or tricyclic antidepressants with ibogaine could lead to severe side effects like seizures, serotonin syndrome, or death.
3. Antagonistic Interaction
These substances inhibit or contradict the effects of ibogaine, making both substances less effective.
An example of this could include 5-HT3 receptor agonists.
18-MC: Non-Psychoactive Ibogaine
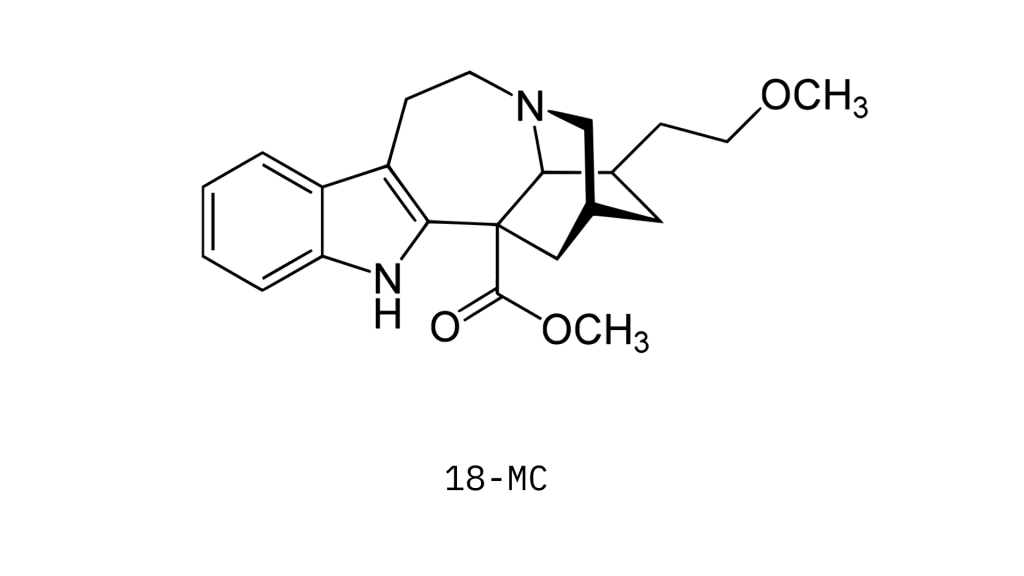
18-MC stands for 18-methoxycoronaridine; it’s a synthetic, non-psychedelic derivative of ibogaine. It was first created in 1996 by Stanley Glick (Albany Medical College) and Martin Kuehne (University of Vermont).
This substance is currently being investigated as a potential treatment for addiction — funded by a psychedelic startup called MindMed.
So far, preliminary research suggests that 18-MC could prove useful for reducing cravings in people dependent on opiates, stimulants, and nicotine. It’s thought to work by reducing the neuroadaptations in the dopamine receptors that contribute to drug cravings and compulsive behavior [1].
This substance activates the nicotinic receptors (α4β4), just like ibogaine, but it has no affinity for the α4β2 subtype, nor NMDA-channels or serotonin transporters.
There’s still a lot of research that needs to be done before this medication is likely to be approved for treatment, and the lack of psychoactive effects begs the question of whether or not the mystical experience is required for the full extend of therapeutic benefit from iboga and its alkaloids.
There are reports from people experienced in administering ibogaine that the raw root bark of the iboga plant has a much better positive outcome than the isolated ibogaine used in most clinical settings.
Much of the benefit that comes from these substances owes itself to the ability to reframe the self, facilitate ego-disillusionment, and induce a transient state of ontological shock in the individual. These experiences are what reframe our existence and show us aspects about ourselves that influence our thoughts and actions that we didn’t even know were there.
There have already been several new derivatives of 18-MC that are currently working their way through the pipeline. Some of these derivatives are already showing indications that they’re stronger than 18-MC itself. A few examples include ME-18-MC and 18-MAC.
How Does Ibogaine Compare to Other Psychedelics?
Ibogaine is one of the most well-known psychedelics. It’s best known for its use in the treatment of addiction. But it isn’t alone here — many of the greatest psychedelic substances we have available offer similar effects as ibogaine — but with a few key differences.
Ibogaine vs. Ayahuasca
| Ayahuasca | Iboga | |
| Origin | The Amazon Basin | The Congo |
| Mechanism of Action | 5-HT2A Agonism | 5-HT2A Agonism |
| Level of Risk | Low | Moderate-High |
| Celerity | Low | Very-Low |
| Potency | High | High |
Perhaps the closest substance to ibogaine is ayahuasca. Both substances have a long history in the use of spiritual healing and ceremony. Both produce powerful, long-lasting visions and facilitate introspective and mystical experiences.
Ayahuasca comes from the Amazon — Iboga comes from the Congo.
Ayahuasca is used for many of the same applications as iboga — despite having completely separate origins. This is an ode to the importance of reconnecting the body and the psyche — rather than relying specifically on altering dopamine levels or other neurotransmitters in the brain. Addiction is not a disease of the brain; it’s a symptom of disconnection between our true self and the mind. These visionary plants both work to re-establish this connection.
The difference between these substances in terms of the effects is that iboga is more of a dreamlike trip, while ayahuasca could be described as being interdimensional. Ibogaine also has much more of a focus on looking inward (but not always). It’s highly introspective. Ayahuasca can be too, but there’s more freedom in the ayahuasca experience to look outward at the universe at large.
The main therapeutic difference between the two, aside from the ceremony involved with their use, is the effects on withdrawal symptoms. Ayahuasca does very little to manage active withdrawal symptoms from using addictive drugs. Conversely, iboga has powerful anti-withdrawal effects. For this reason, many people will turn to iboga while still addicted to drugs and then turn to ayahuasca for further healing of traumas to help them remain sober long-term.
There’s also a big difference in the level of risk for these traditional psychedelics. Iboga is much more dangerous than ayahuasca. There have been deaths from both substances (though very rare) — but comparatively, iboga carries much more inherent risk than ayahuasca.
Ibogaine vs. 5-MeO-DMT
| 5-MeO-DMT | Iboga | |
| Origin | Bufo alvarius toad & synthetic | The Congo |
| Mechanism of Action | 5-HT2A Agonism | 5-HT2A Agonism |
| Level of Risk | Low | Moderate-High |
| Celerity | High | Very-Low |
| Potency | Very High | High |
5-MeO-DMT is the active ingredient in the Bufo toad (Bufo alvarius) — otherwise known as the Sonoran Desert toad or the Colorado River Toad. It’s also available in a synthetic form, which is generally the preferred source due to the environmental impact of harvesting this compound from the secretions of toads.
Iboga and 5-MeO-DMT share many common applications — both are used in the treatment of depression, addiction, and existential anxiety. They’re both powerful psychedelics that facilitate life-changing spiritual experiences and help dislodge repressed physical and psychological traumas from deep within the psyche — when used with the right intention and in the right set and setting.
The primary difference between these two substances is their celerity. This is a word that describes the amount of time it takes for the substance to start producing effects and how long these effects last.
5-MeO-DMT has a very high celerity. Within a matter of seconds, the effects go from 0–100 — as though you’re instantly teleported into another realm. Just as fast as it started, the experience comes to an end. The entire duration can last anywhere from 15 to 45 minutes.
Iboga has a very low reputation. It takes 1–2 hours for you to feel any effects, and they can last anywhere from 8 to 24 hours. The second phase can last even longer — up to 48 hours.
Like ayahuasca, and iboga 5-MeO-DMT has been proven to be extremely useful for the treatment of addiction. This effect doesn’t necessarily stem from an interaction with dopamine, the way researchers exploring non-psychedelic ibogaine derivatives suggest — rather, it comes from the spiritual experience itself and the surfacing of past traumas that are driving the symptom of addiction.
Ibogaine vs. Ketamine
| Ketamine | Iboga | |
| Origin | Synthetic | The Congo |
| Mechanism of Action | Kappa-opioid agonism | 5-HT2A Agonism |
| Level of Risk | Moderate | Moderate-High |
| Celerity | Moderate | Very-Low |
| Potency | Moderate | High |
Ketamine is more of a dissociative than a true psychedelic. This has a lot of similarities to iboga, which is considered both psychedelic and dissociative.
The difference between psychedelics and dissociatives may seem like semantics, but there is a clear subjective difference in the experience.
Ketamine and iboga are both very lucid substances — which is an important aspect of dissociatives. While there are plenty of differences, the subjective experience of these compounds has a lot of overlap.
It’s common for both of these substances to create visions that could be described as “dreamlike”. Many users report viewing their life as some sort of a slideshow.
One minute you’re watching yourself endure a traumatizing experience from your past — the next moment, you’re teleported to a completely different setting. Maybe you’re sitting in a park or on the beach feeling full of love and appreciation.
Despite having entirely different mechanisms of action, some of the experiences from these substances overlap — but they’re entirely distinct in other ways.
The celerity of ketamine and iboga or ibogaine is very different. Ketamine takes about 30 minutes to reach peak effects and usually lasts about 2 or 3 hours in total. Ibogaine lasts much longer — often exceeding 10 hours.
Both ibogaine and ketamine are used in the treatment of addiction. Ketamine is much more commonly used to treat depression than ibogaine in clinical settings. It’s preferred for its shorter duration and more idyllic safety profile. It’s also the only approved psychedelic for the treatment of depression in the United States at the moment. There are dozens of ketamine-clinics across the United States.
How Does Ibogaine Work?
Ibogaine is classified as an indole alkaloid — which is the same chemical classification of psilocybin, LSD, 4-AcO-DMT, and others.
These alkaloids work through several different mechanisms, including:
- Sigma-2-receptor activation [4]
- kappa-opioid receptor activation [5]
- NMDA receptor agonism [5]
- 5-HT2A receptor activation [6]
It’s believed that most of the psychedelic effects of ibogaine come from its impact on the serotonin receptors, namely, the 5-HT2A receptor.
This activity causes several things to happen:
- Stimulates BDNF — which increases synaptic plasticity
- Stimulates glutamate — which increases brain activity
- Suppresses the default mode network (DMN) — which leads to a higher state of entropy in the brain
All of these activities lead to what we perceive as the psychedelic experience.
Other receptors that influence the experience induced by ibogaine are the NMDA agonism and kappa-opioid receptor activation. These effects are likely the cause of ibogaines dissociative flavor. Other substances that work through the kappa-opioid receptors include ketamine, PCP, DXM, and salvia — all of which offer similar dissociative, out-of-body experiences.

Ibogaine & The Treatment of Addiction
Most of the research on iboga and its alkaloids is centered around its use for addiction therapy.
One study performed in New Zealand by MAPS (Multidisciplinary Association for Psychedelic Studies) administered ibogaine (25–55 mg/kg) and a benzodiazepine to 14 people with clinical opioid addiction [2].
The study conducted follow-ups at 3, 6, and 12 months following the trial, as well as urine drug screens to check for signs of opioid use. At the 12-month follow-up, 75% of the trial participants showed no signs of opioid drug use. One person died during treatment in this study.
Another similar study from MAPS was conducted in Mexico in 2017 [3]. This study also explored the effects of ibogaine therapy in the treatment of addiction. The study reported a >75% reduction in Drug Use scores compared to the pretreatment baseline.
Iboga Reverses the Neuroadaptive Changes That Cause Drug-Seeking Behavior
There are several theories about how ibogaine works for treating addiction. The pharmacological explanation comes from the ability of ibogaine and related iboga alkaloids to reverse the changes made within the dopaminergic system in the brain that leads someone to crave the drug.
This suggests that ibogaine may reverse the desensitization of the dopaminergic neurons in the brain that have become unresponsive to normal stimuli in the absence of drugs — such as stimulants or opioids.
In simple terms: when you’re addicted to drugs, your brain chemistry adapts to account for the drug being in the system. If you stop using them, your brain chemistry falls out of balance because of these changes, causing withdrawal. Ibogaine (appears) to reverse these adaptive brain changes, thus eliminating withdrawal.
This model of ibogaine-assisted therapy for addiction doesn’t rely on the need for a mystical experience. There’s a lot of research on this effect coming from the folks at Mind Med who are developing 18-MC around this concept.
Iboga & The Psychedelic Experience Dislodge Trauma Underpinning Addiction
Another theory follows the same mechanisms as unrelated psychedelics like ayahuasca, 5-MeO-DMT, psilocybin, LSD, and mescaline.
The idea is that psychedelics reconnect the mind with the body. This model relies on the idea that addiction is not a “chemical imbalance” — rather, it’s a symptom of a systemic detachment of the mind and the body.
A drug addict seeks the use of substances to escape from pain or discomfort. This pain and discomfort may be physical or it may be emotional. They’re attempting to self-soothe their pain by physically numbing the body or diverting attention further away from the physical self through the use of drugs.
The best treatment, therefore, isn’t something that changes the chemical “balance” of the brain but instead helps us identify the source of our trauma and bring it into the higher spheres of consciousness where we can more actively heal them.
Final Thoughts: The Future of Iboga & Ibogaine
The future for ibogaine therapy looks promising — but there are some hurdles that may limit its adoption into mainstream addiction therapy.
Iboga is highly effective for managing addiction — even in cases that have been unsuccessful with other forms of addiction therapy or in patients who are currently addicted to drugs. Conversely, ayahuasca or other psychedelics are usually only recommended once the user has weaned themselves off the substance.
When used in the right context, with trauma-informed psychotherapy, the results of iboga treatment truly speak for themselves.
The need for this plant, or others like it, can’t be understated. The opioid epidemic in the United States and around the world has gotten completely out of control — the current models for addressing this issue have proven themselves ineffective.
The need for new, effective treatments like ibogaine is higher now more than ever. There are movements pushing for the legal use of ibogaine-assisted therapy are moving along but appear to be at least 12 months away from being a reality in the US.
There are also signs that ibogaine regulations could regress in places like Canada, where it’s currently legal for approved clinics.
References
- Szumlinski, K. K., Maisonneuve, I. M., & Glick, S. D. (2001). Iboga interactions with psychomotor stimulants: panacea in the paradox?. Toxicon, 39(1), 75-86.
- Noller, G. E., Frampton, C. M., & Yazar-Klosinski, B. (2018). Ibogaine treatment outcomes for opioid dependence from a twelve-month follow-up observational study. The American journal of drug and alcohol abuse, 44(1), 37-46.
- Brown, T. K., & Alper, K. (2018). Treatment of opioid use disorder with ibogaine: detoxification and drug use outcomes. The American Journal of Drug and Alcohol Abuse, 44(1), 24-36.
- Mach, R. H., Smith, C. R., & Childers, S. R. (1995). Ibogaine possesses a selective affinity for σ2 receptors. Life sciences, 57(4), PL57-PL62.
- Glick, S. D., Maisonneuve, I. M., & Pearl, S. M. (1997). Evidence for roles of κ-opioid and NMDA receptors in the mechanism of action of ibogaine. Brain Research, 749(2), 340-343.
- Helsley, S., Fiorella, D., Rabin, R. A., & Winter, J. C. (1998). Behavioral and biochemical evidence for a nonessential 5-HT2A component of the ibogaine-induced discriminative stimulus. Pharmacology Biochemistry and Behavior, 59(2), 419-425.