Can Kratom Cause Seizures?
Here’s a look at the research and statistics on kratom use and seizures.
Kratom (Mitragyna speciosa) is generally described by enthusiasts as a harmless medicinal alternative to conventional opioids.
Unfortunately, very few people are certain of what kratom is capable of in terms of both positive and negative. Its benefits and actions are not fully understood, nor is the extent of the damage it might do.
There are more than enough reports of kratom causing seizures to warrant concern. This article explores the available evidence of kratom causing seizures so you can consider the risks before using or continuing to use kratom.
Can Kratom Cause Seizures?
The short and sweet answer to this unfortunate question is a resounding yes. It seems that in certain circumstances, kratom can, indeed, cause seizures.
There are many reports of people who have had seizures while taking kratom. Most of these reports are anecdotal and come from online kratom communities like Reddit. A few scientific studies report on kratom-related seizures, but they can’t conclusively prove that the seizures were the direct result of kratom.
For example, one study evaluated youth who had seizures following kratom ingestion, but the variables were too huge for the study to be of value. The subjects used kratom anywhere from “more than 8 times a month” to every day, had been using it for periods of months up to eight years, and experienced seizures anywhere from 10 minutes to 72 hours post-ingestion.1
Nonetheless, that alone is enough evidence to warrant caution. Combined with anecdotes from Reddit, there is reason to think that kratom lowers the seizure threshold and can cause seizures, especially in people predisposed to epilepsy.
Many of the seizures were caused by people who had large habits. In some cases, they resulted from people who were mixing kratom with other substances (though not, like most kratom communities would have you believe, “hard drugs” or research chemicals. Simple, everyday nootropics such as Modafinil, gabapentin, or 5-HTP.)
At least one study coincides with several posters who reported concomitantly using Dexedrine or lisdexamfetamine, an ADHD medication, with their kratom.
The reports of seizures are quite disturbing and all very serious. The types of seizures can range from grand mal to tonic-clonic (alternating rhythmic jerking of muscles with spontaneous sudden contractions and stiffness).
Seizure reports are also likely underreported, as people who have seizures when they’re alone don’t usually realize that they’ve had a seizure. The firsthand experience tends to be something akin to feeling momentarily dizzy or confused and then waking up in a different position or on the floor without any memory of falling asleep.
Many of the threads posted by people who have had seizures draw in reports from other kratom users who are unsure but speculate that they may have also experienced a kratom-related seizure.
They describe strange experiences that they felt were potentially building up to a seizure. Blurred vision, unsettling cognitive processing changes, blackouts, waking up on the other side of the room after settling down in bed to watch TV after a dose of kratom.
All of these symptoms are enough to make someone seriously reconsider using kratom. So why aren’t these serious issues taken more seriously by the kratom community?

Challenges Interpreting Data Regarding Kratom & Seizures
The population of the United States, one of the world’s most prolific kratom-using demographics, is divided regarding kratom. This has seriously hindered research and development regarding it and is largely the reason that questions like, “Can kratom cause seizures?” don’t have cut-and-dry answers yet.
Many members of the kratom-using demographic feel that they are subjected to a smear campaign against the plant. There’s a lot of confusion. And where there isn’t disinformation, there is often a lack of information. The plant isn’t FDA-approved, which hinders interested parties from seeking funding that might verify some of the claims made about it.
On the one hand, you have bureaucratic folk supporting the FDA’s claims that kratom is a deadly, dangerous drug that should be banned globally and scheduled alongside heroin and fentanyl. On the other extreme end, you have people who believe that kratom is a panacea and refuse to consider the possibility of it causing any ill effects whatsoever [3].
A third, more rational group exists somewhere in the middle of these two poles, and this is where the truth lies.
The Blurred Line Between Fact & Fiction
Some of the more serious claims made about kratom (such as the suggestion that it’s a deadly narcotic) come from erroneously interpreted studies and autopsy data. The FDA sensationalized the perceived dangers of kratom by using clickbait titles that seem to be an amateur attempt to scare people away from using it.
This is a bit of a strange approach for a federal, government-appointed agency. They deliberately focus on keywords implying that kratom alone causes death. Instead of acknowledging the millions of people using kratom for pain and addiction, they state that “millions of people are pushing unproven claims about kratom helping with pain or addiction” [4].
This sort of fear-mongering is unacceptable and discredits the FDA as a whole. Convinced that the FDA and DEA are nothing but propaganda-pushing, profit-hungry monsters intent on banning kratom to cash in on methadone and prescription painkillers, the kratom community at large now discredits the majority of evidence gathered by any federal organization.
As such, the community now tends to ignore some truly alarming data from poison control centers regarding kratom.
Over 1,800 calls were placed due to kratom between 2011-2017. Over 1,000 of them were in 2016 and 2017 alone; 65% of the calls were from people using kratom alone, and of these, just over half resulted in serious medical complications like seizures, comas, liver problems, or cardiac arrest [5].
The FDA and DEA’s decision to sensationalize these facts rather than provide unbiased reporting pushed a lot of buttons in the kratom community. There are an estimated two million people using kratom in the USA alone. A couple of thousand phone calls to poison control regarding a herb that’s not widely discussed is hardly unusual for something this widespread [6].
Thus began a movement to discredit the studies and autopsies of people who have died with kratom in their blood.
Not all of these efforts were completely invalid. Many victims were on various other prescription drugs that most likely had interactions with kratom. There are more than 260 interactions between kratom and other substances.
A review of kratom deaths in the UK observed that only 23% of all cases resulted from mitragynine alone and that 87% of the recorded fatalities occurred among individuals who had a history of poly-substance abuse. Causes of death were generally cited as “toxic effects of kratom + other substances; underlying health issues” [7].
The problem with this is that it actually does a disservice to those who are suffering from real, dangerous side effects of kratom—like the large number of people who have had seizures.
For years, these people have been rejected from kratom communities and told that their seizures were caused by something else. It was assumed that there was a “never cry wolf” scenario going on, so anybody who spoke up about any serious ailments caused by kratom was immediately discredited.
Reports of People Having Seizures From Kratom
There are, quite frankly, a lot of reports of people having seizures from kratom. Most of these reports state that they only became aware that they had a seizure because somebody found them afterward and were fairly certain that they had had them before without realizing it.
That means that there’s probably a significant number of people who haven’t reported their kratom seizures. Regardless, here are a few of the most significant and troubling reports of people having kratom-related seizures, both anecdotally and from medical reports.
Example #1
User u/throaway298811’s post described their full-blown grand mal seizure that resulted in hospitalization after taking between 10-25 g of Bali kratom from Colorado Cures for four days. On the day of the seizure, they had taken about 15-20 g and took another two capsules before laying down in bed.
After laying in bed, they felt extremely dizzy and sweaty and began having muscle spasms, loss of vision, and brain zaps (a somewhat common symptom associated with serotonin levels). The next thing they knew, they awoke to their mom slapping them in the face on the other side of the room, on the floor.
They had been screaming and aggressively vomiting for some time, and his mom had come in to try and bring him back to consciousness. She immediately took him to the hospital. He bit off a chunk of his tongue during the experience and felt extremely traumatized. People in r/kratom discredited him and downvoted him for telling his story.
He also mentioned experiencing kidney issues due to kratom.
Example #2
u/Dysphoric_Otter reported that they knew their kratom use was out of hand. They’d been using steadily for 4 years after the plant helped them stop drinking, and then it was just a regular part of their life. They struggle to quit because it’s taken such a foundational role in their life that it’s hard to imagine living without it.
One day, they opened a new bag and took their regular dose. They got the wobbles, felt shaky, and then woke up to see their girlfriend sitting beside them, crying and saying that he had just had a seizure. He was confused and had no idea what she was talking about. His habit was about 40 g per day, with no family history of seizures.
u/Duncan4224 was quick to add his similar experience in the comments. He also experienced waking up next to his girlfriend, crying, telling him that he had seized out. Like many people, Duncan experienced numerous online support groups telling him that kratom wasn’t the cause of his seizure until he found solace in the subreddit r/quittingkratom.
u/reddtit chimed in later in the thread. He had also had two seizures, both times when he took a large dose of kratom mixed with gabapentin. Interestingly, gabapentin is an antiepileptic drug.
However, he says he constantly follows any posts related to kratom and seizures and notes that kratom lowers the seizure threshold and may cause other drugs to do the same.
Every kratom extremist who denied the association always revealed that they hadn’t bothered reading the post by saying, “gabapentin is antiepileptic, bud.” Nonetheless, patient Reddit would provide a link to a peer-reviewed study showing that antiepileptic drugs can actually lower the seizure threshold when taken by non-epileptic people.
Of course, nobody had anything to say in response to these links.
Example #3
This story is from a 65-year-old man with the user name u/Privacy_Advocate_ who had been using kratom for years. At the time of writing, he had just had his seventh seizure. Over the years, he’d used as much as 85 g a day. He started having seizures two months prior to his post — long episodes that lasted half an hour — and came to Reddit to see if there were any similar stories.
Later in the thread, he engaged in a dialogue that gives a very good example of the issues present in the kratom community and how they can distort the perceptions of even the people who are seeking help.
The person replying to him linked him to a thread in which four people with similar-sized kratom habits all reported having seizures. Privacy_advocate_ simply said that “those stories don’t seem to hold much weight,” despite that they all mirrored his own story. He seemed instead to be looking for stories that denied the possibility of kratom-induced seizures.
The commenter replied to his denial of the anecdotes by showing him toxicological data from a medical journal that indicated that kratom caused a seizure. His reply? “It seems like they just assumed the kratom caused the seizure because they couldn’t find anything else.”
Before giving up, the commenter urged him to look at the pages of Reddit results from dozens of people having seizures with daily, large kratom habits. That is to say, dozens of anecdotes that verify and confirm the original poster’s story. And yet, he responds with, “I came here to find anecdotal evidence and haven’t been satisfied.”
This staunch refusal to consider the possibility that kratom might actually be causing the problems he came to ask for help about is very telling.
Reports of Kratom & Epilepsy
Many users have drawn a link between kratom and epilepsy. The overall conclusion seems to be that kratom lowers the seizure threshold. In pre-epileptic people, this can bring on the condition quicker and more severely. What’s even more concerning is that excessive kratom use seems to cause symptoms in some people that are indicative of epilepsy.
The dizziness, confusion, and vertigo often associated with “the wobbles,” may be similar to some pre-seizure symptoms.
u/lonelydruggy said that they had a tonic-clonic seizure for the first time an hour after taking a large dose of kratom. This seems to be a recurring theme: most seizures occur when people take larger than normal doses.
While withdrawing at the hospital, they were diagnosed with generalized epilepsy due to a number of strange symptoms that they reported. These included shaky hands, sudden uncontrollable muscle twitches, getting feelings of deja vu, and “feeling really strange.”
Once he stopped taking the kratom, all the symptoms disappeared.
One user who has deleted their account suffers from epilepsy and remains pro-kratom. He simply pushes for greater awareness and harm reduction practices, pointing out that everyone reacts differently to drugs.
He actually contributed to a lot of the publication of kratom’s negative side effects through direct work with the FDA and DEA because he had seen how much harm the plant had caused people. He continues to use it and doesn’t think it should be banned but says that people need to be aware of the risks.

Why Would Kratom Cause Seizures? Biological & Neurological Actions
There are many different ways that seizures can occur.
When it comes to drug and alcohol-induced seizures, most professionals or educated users are quick to point the finger at GABA. GABA is a neurotransmitter that helps to dampen the effect of glutamate. Glutamate, in turn, is an excitatory neurotransmitter. In short, it helps your neurons fire electrical messages at each other. That’s how they talk.
One of the major causative factors for a seizure is overexcitation of the nervous system. If GABA weren’t around, glutamate would run amok, causing all of our nerve cells to rapid-fire electricity at one another, resulting in — you guessed it — a seizure.
Some drugs and alcohol cause the body to release excess GABA, mainly alcohol and benzodiazepines. When you stop using these drugs, your body needs to remember how to produce GABA on its own because it’s basically become lazy in the GABA department thanks to having an external supply. During this period, the seizure threshold is massively diminished [8].
Because kratom can be effective for anxiety, many speculate that it is a strong GABAergic as well. While some opioids do affect the GABA system due to the expression of mu-opioid receptors on some GABAergic interneurons, it’s not enough to throw the whole system out of whack [9].
So, the point of this first section is mostly to get that idea out of the way: kratom-related seizures (most likely) have nothing to do with it being a GABA-releasing agent. In the case of GABA releasers, seizures tend to be more common during the withdrawal period, not after the user has taken the drug. Kratom seizures tend to occur after users take a large dose.
This brings us to a more interesting point: kratom and certain opioids are actually believed to antagonize the GABA system. In other words, they make the body less responsive to it. Since GABA is the neurotransmitter responsible for keeping glutamate in check and preventing seizures, this could explain why kratom lowers the seizure threshold [10].
Assuming a dose-responsive effect, the more kratom you take, the more GABA receptors would become antagonized. This would discourage the dampening effect that GABA has on our excitatory nervous transmission and would explain some of the weird, pre-epileptic symptoms that high-dose kratom users have, as well as the lowered seizure threshold.
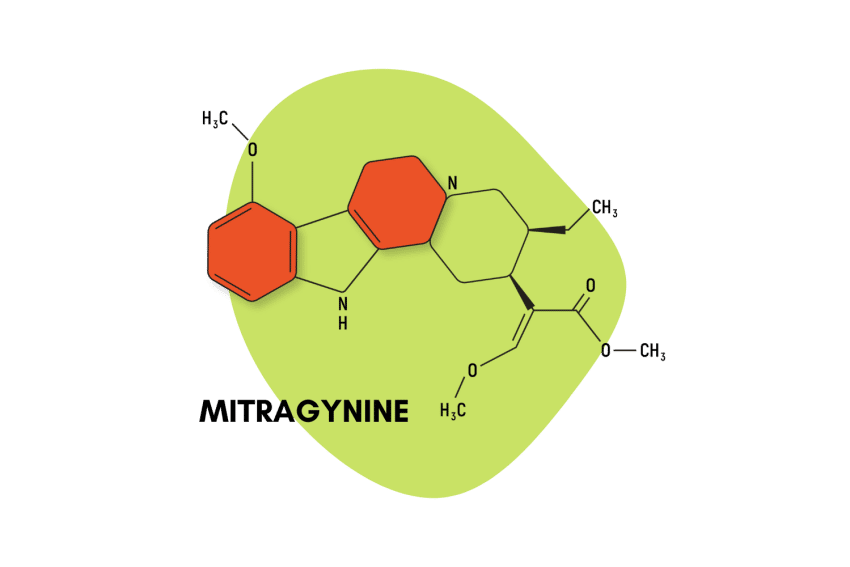
Kratom & Its Alkaloids
On top of this, kratom and its alkaloids do have a very diverse number of effects, however. They interact with all three of the opioid receptors (mu, kappa, and delta), the adrenergic system, various serotonin receptors, dopamine, and acetylcholine. This isn’t to mention its effect on the hormonal systems [11].
So, in addition to antagonizing GABA and making your body less capable of resisting the overexcitation of glutamate, it also stimulates a wide sect of neurotransmitters.
One poster on Bluelight brings up the fact that agonists of the delta-opioid receptor (DOR) tend to lower the seizure threshold. He is familiar with alpha-chloro morphide, a strong DOR agonist known to lower the seizure threshold.
He goes on to describe the drug as being strangely stimulating and unlike other opioids — a description often applied to both kratom and tramadol, the two opioid-like substances most often linked to seizures. While they do provide some of the opiate-like warmth and sedation, they’re unhinged by a strange undercurrent of nervous stimulation.
He observes that some of the alkaloids in kratom are most likely epileptogenic convulsants. One of the main culprits, he says, is mitragynine pseudoindoxyl, a metabolite that is formed when mitragynine is exposed to oxygen for long periods of time [12].
He also notes that the alkaloid ryncophylline has similar properties and that kratom has a number of yohimbine-like alkaloids. Yohimbine is one of the most powerful nervine stimulants in the world, many times stronger than coffee. It could easily lower the seizure threshold [13].
Kratom & Serotonin — Similarities to Tramadol
Serotonin is another one of the neurotransmitters involved in bodily functions. Its actions are extremely diverse, ranging from perception to digestion, from cognition and mood to muscle movement. There are more than 20 different receptor types in the serotonin system, and activating different ones can cause seriously different effects.
There is one opioid drug that was widely prescribed for years that had a strong influence on serotonin: tramadol. Tramadol has effects that are strikingly similar to kratom, which is also known to influence serotonin.
Both substances are more stimulating than typical opioids. They tend to produce a unique sensation—the previously described “strange undercurrent of nervous stimulation” — as well as causing cognitive deficits like brain fog and memory loss.
Dr. Fudin of Practical Pain Management describes tramadol as a “nightmare in terms of side effects, tolerability, and pharmacokinetics,” and says that kratom is like a sloppier form of it, which is about as bad of an insult as you could hurl at a psychoactive plant.
But he’s right. The pharmacology of kratom is ridiculously complex.
At low doses, its stimulant effects override any sedation, at least at the onset. It behaves like an MAOI, the notoriously difficult and high-risk antidepressants that were widely prescribed half a century ago until researchers could develop something with fewer side effects, at which point they were rapidly withdrawn [14].
Like kratom, they interfere with the reuptake of norepinephrine, dopamine, and serotonin. All of these neurotransmitters are part of a family called monoamines. MAOIs (monoamine oxidase inhibitors) basically prevent them from taking time off after doing their job, which is pushing the button to activate whatever receptor (dopamine, serotonin, etc.) they fit into.
So instead, they’re basically stuck in their office cubicle with nothing to do but push the button over and over, massively increasing the effects of these neurotransmitters. This is why MAOIs interact with just about every other kind of medication.
As if that weren’t complicated enough, kratom also works as a centrally acting alpha agonist. This could deceive users, blunting the symptoms of the reuptake inhibitors.
In low amounts, this could theoretically prevent opioid withdrawal, but most people prefer to stave off withdrawal with higher doses, where kratom begins to exhibit activity at the mu, delta, and kappa opioid receptors.
Kratom, Dehydration, & Hypokalemia
Kratom is a diuretic. Diuretics extra make you pee. If you pee a lot, then you’re going to be sending a whole lot of nutrients down the drain.
Assuming that you have a relatively healthy diet, then this shouldn’t be an issue. Your kidneys filter out all of the nutrients that your body doesn’t need. But if you’re peeing constantly, they’re going to end up depleting your body of key nutrients, mainly electrolytes. One of the most important electrolytes to replenish when using diuretics is potassium.
Most natural diuretics, like dandelion leaf, are chock full of potassium and can easily offset any risk of hyperkalemia (potassium deficiency). Others, like parsley and asparagus, are aquaretics and increase fluid excretion without affecting electrolytes. However, these are palatable and easily digested; it seems that nature intends for them to be eaten [15,16].
Kratom leaf needs to be ground into a powder prior to being swallowed and, even still, often causes digestive upset. Unless you’re a koala, it doesn’t seem that nature intended it to be a great salad green. It might contain some potassium in small amounts; even if it does, additional electrolyte supplementation may be a good idea.
Hypokalemia itself can cause seizures if it becomes serious enough, but it’s quite rare. Still, taking diuretics on a daily basis for months could cause hypokalemia if you’re not supplementing with potassium. Taking diuretics for years? At massive doses over the 50-gram range? That sounds like a serious potential health hazard [17].
So, Is Kratom Safe to Take?
We’ve just provided you with all sorts of information that probably seems pretty scary. But before you run and toss all your kratom in the trash, look at the big picture. Kratom is no different than any other drug — that’s right, I did the unthinkable and called it a drug.
But with pharmacological actions as complex and potent as kratom has, it seems risky to refer to it as a simple herb. Nobody refers to opium poppies as simple herbs (except for people trying to justify daily habits involving the consumption of dozens of opium poppies).
But even opium poppies can be used safely. With enough preparation and wherewithal, they can even be used in such a manner that they don’t produce any serious addiction, although this requires serious preparation and a well-planned regimen of potentiators and antagonists and is generally not something the average user is going to bother with.
But what every user should bother with is following proper health and safety practices when using kratom. Make sure that you stay hydrated. Follow regular precautions like you would when taking any diuretic, which means replenishing your electrolytes.
Don’t combine kratom with other drugs. If you’re considering doing so, just visualize the enormous complexity of neurochemical chaos that’s already going to be wreaking havoc throughout your body once exposed to kratom. Then, imagine introducing another substance into the mix.
If that doesn’t deter you, then you should perhaps reconsider your usage entirely.
Lastly, remember that it can lower the seizure threshold, and don’t hesitate to share that information with people. If you see people getting shamed for having concerns about kratom, refer the concerned users to unbiased sites like this one or r/quittingkratom.
Final Thoughts on Kratom Causing Seizures
It’s not a pleasant thing to admit, but it’s certainly an important one: kratom has been linked to seizures in dozens of situations. These usually involve high-dose, habitual users and often with the combination of other drugs or pre-epileptic patients. This fits in easily with the current understanding of opioids lowering the seizure threshold.
But most opioids are single chemicals; kratom is an entire pharmacy unto itself. Its interactions are much more complex and similar to tramadol — the only opioid directly and consistently linked to seizures.
As such, it’s best to be extremely cautious when using kratom. Take the precautions mentioned above and remember to keep your dosage low. Avoid daily dosing if possible, and don’t take or do anything else that could further lower your seizure threshold.
Lastly, make sure that you’re spreading accurate information about kratom as far and wide as possible. The more that people know about this plant, the fewer people will have to suffer serious side effects as a result of ignorance and misinformation.
References
- Halim, S. A., Low, J. H., Chee, Y. C., & Alias, M. R. (2021). Seizures among young adults consuming kratom beverages in Malaysia: A case series. Epilepsy & Behavior, 121, 108057.
- Tatum, W. O., Hasan, T. F., Coonan, E. E., & Smelick, C. P. (2018). Recurrent seizures from chronic kratom use, an atypical herbal opioid. Epilepsy & behavior case reports, 10, 18-20.
- Swetlitz, I. (2018). HHS recommended that the DEA make kratom a Schedule I drug, like LSD or heroin. STAT, 9.
- Food and Drug Administration. FDA issues warnings to companies selling illegal, unapproved kratom drug products marketed for opioid cessation, pain treatment and other medical uses. Food and Drug Administration, Bethesda, MD.
- Corkery, J. M., Streete, P., Claridge, H., Goodair, C., Papanti, D., Orsolini, L., … & Hendricks, A. (2019). Characteristics of deaths associated with kratom use. Journal of Psychopharmacology, 33(9), 1102-1123.
- Palamar, J. J. (2021). Past-year kratom use in the US: estimates from a nationally representative sample. American journal of preventive medicine, 61(2), 240-245.
- Corkery, J. M., Streete, P., Claridge, H., Goodair, C., Papanti, D., Orsolini, L., … & Hendricks, A. (2019). Characteristics of deaths associated with kratom use. Journal of Psychopharmacology, 33(9), 1102-1123.
- Petroff, O. A., Rothman, D. L., Behar, K. L., & Mattson, R. H. (1996). Low brain GABA level is associated with poor seizure control. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society, 40(6), 908-911.
- Shi, M. M., Fan, K. M., Qiao, Y. N., Xu, J. H., Qiu, L. J., Li, X., … & Liu, Z. Q. (2020). Hippocampal µ-opioid receptors on GABAergic neurons mediate stress-induced impairment of memory retrieval. Molecular psychiatry, 25(5), 977-992.
- Werz, M. A., & MacDonald, R. L. (1982). Opiate alkaloids antagonize postsynaptic glycine and GABA responses: correlation with convulsant action. Brain Research, 236(1), 107-119.
- Hanapi, N. A., Chear, N. J. Y., Azizi, J., & Yusof, S. R. (2021). Kratom Alkaloids: Interactions with Enzymes, Receptors, and Cellular Barriers. Frontiers in Pharmacology, 12.
- Spencer, C. A. (2019). A computational approach to predicting and understanding new psychoactive substances (NPS) for developing a database for state and federal crime laboratories.
- Finch, N., & Taylor, W. I. (1962). Oxidative transformations of indole alkaloids. I. The preparation of oxindoles from yohimbine; the structures and partial syntheses of mitraphylline, rhynchophylline and corynoxeine. Journal of the American Chemical Society, 84(20), 3871-3877.
- Shulman, K. I., Herrmann, N., & Walker, S. E. (2013). Current place of monoamine oxidase inhibitors in the treatment of depression. CNS drugs, 27(10), 789-797.
- Hook, I., McGee, A., & Henman, M. (1993). Evaluation of dandelion for diuretic activity and variation in potassium content. International Journal of Pharmacognosy, 31(1), 29-34.
- Hook, I., McGee, A., & Henman, M. (1993). Evaluation of dandelion for diuretic activity and variation in potassium content. International Journal of Pharmacognosy, 31(1), 29-34.
- Khajavirad, N., Shakiba, S., Abbaszadeh, M., & Reyhan, S. K. (2021). Rare presentation of Gitelman syndrome: a case report and literature review. Case Reports in Clinical Practice, 6(1), 20-24.