Oxazolam: A Comprehensive Guide
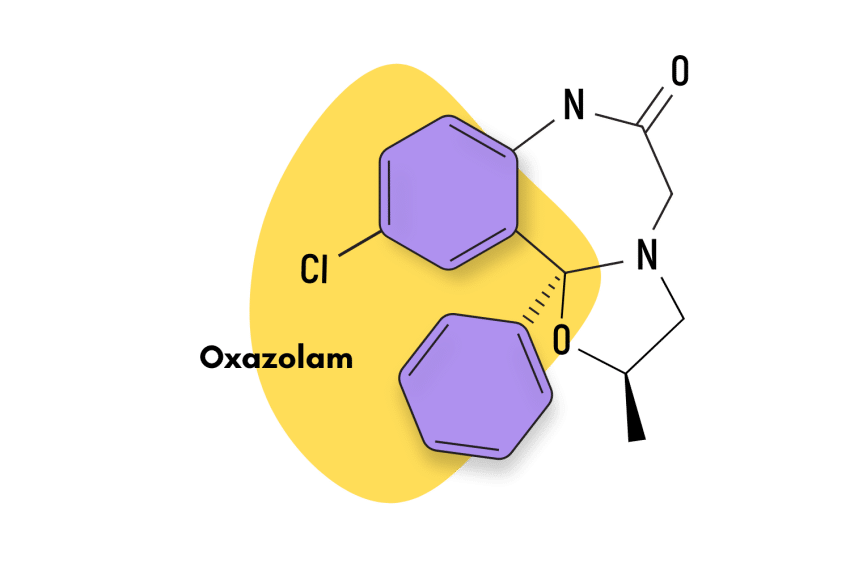
Oxazolam is a benzodiazepine derivative first discovered in the 1970s but never approved as a medication.
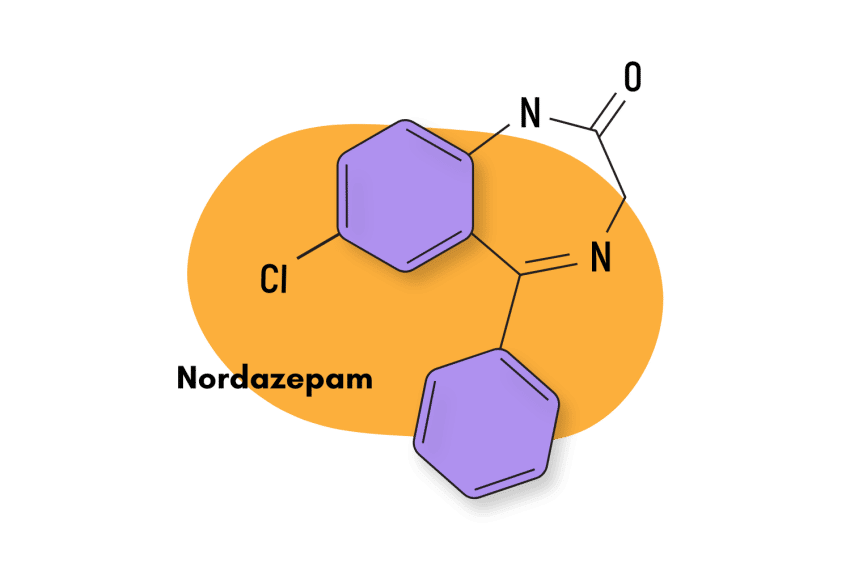
Oxazolam acts as a prodrug for another, FDA-approved benzodiazepine called nordiazepam. This means the effects of oxazolam have been indirectly proven to offer clinical relevance through its active metabolites.
Despite never being approved for use, oxazolam has found its way onto the grey market as a designer drug. A lot of oxazepam’s popularity comes from its status as a prodrug for other, more active benzodiazepines. In some countries, it’s legal to sell oxazolam because it isn’t officially banned.
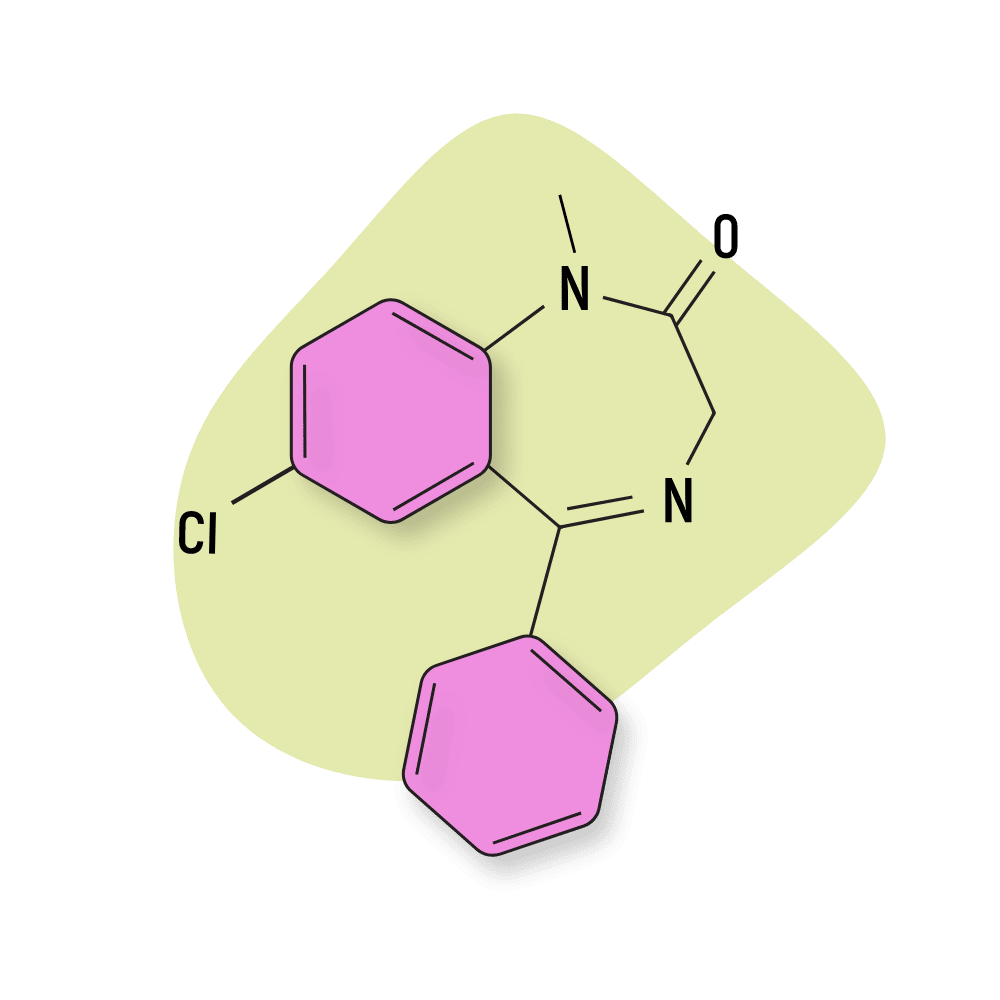
Oxazolam Specs
| IUPAC Name | (2R,11bS)-10-chloro-2-methyl-11b-phenyl-2,3,5,7-tetrahydro-[1,3]oxazolo[3,2-d][1,4]benzodiazepin-6-one |
| Other Names | Nordaz, Stilny, Madar, Vegesan, Calmday, Nordiazepam, Desoxydemoxepam, Desmethyldiazepam |
| Metabolism | The metabolic clearance of oxazolam is not CYP mediated. The kidneys perform the excretion from the body. |
| Duration of Effects | Oxazolam is a short-acting benzodiazepine (6-12 hours). However, its metabolite, nordiazepam, has one of the longest elimination half-lives out of all known benzodiazepines (36-200 hours). |
| Status | Research Chemical |
| Common Dosage | 10-25 mg |
| PubChem ID | 62779 |
| CAS# | 439-14-5 |
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Oxazolam Work?
Oxazolam is a fast-acting benzodiazepine. After ingestion, its elimination half-life generally falls within the range of 6 to 12 hours, which means that its function as a prodrug of nordiazepam happens quickly.
After oxazolam is metabolized into nordiazepam, the pharmacological effects of nordiazepam are known to occur through the standard GABA-A mediated pathway. This entails that nordiazepam falls in line with the majority of “classical” benzodiazepines in terms of its primary mechanism of action [1].
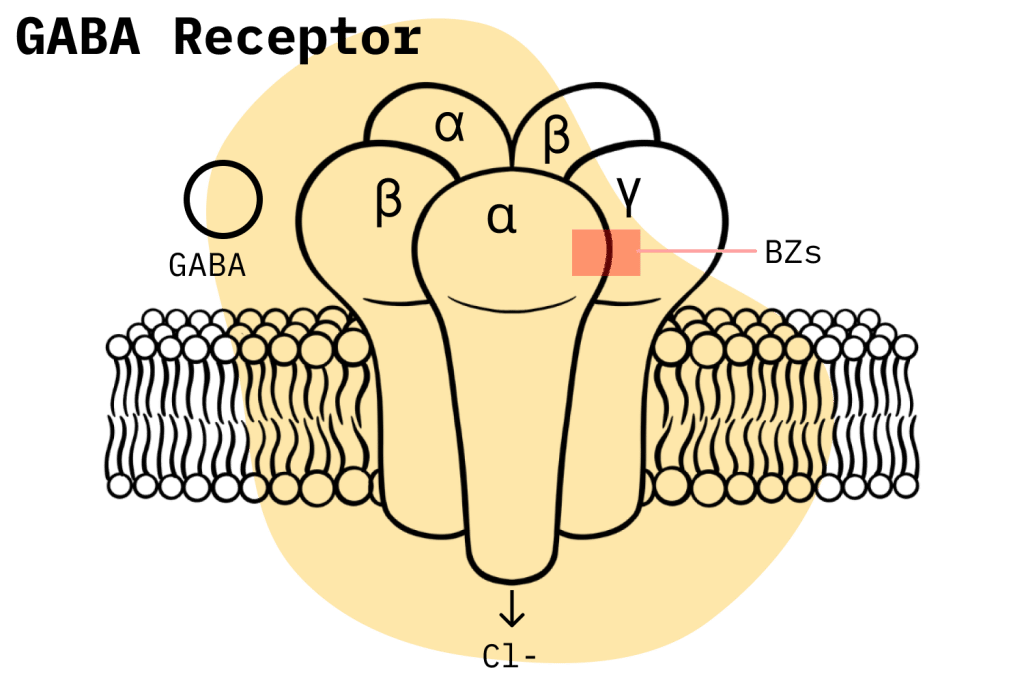
Nordiazepam is only a partial GABA-A agonist rather than a full agonist, and this has certain implications in terms of its pharmacology. A full agonist reaches the maximal response capability of a receptor system when compared to a partial agonist, which can only achieve partial efficacy even if it reaches full receptor occupancy.
In benzodiazepine pharmacology, full agonist benzodiazepines generally elicit stronger effects than partial agonist benzodiazepines and tend to cause more adverse effects because of this; as such, nordiazepam is considered to be of lesser potency, especially in its amnesic and muscle-relaxing effects [1].
Is Oxazolam Safe? Risks & Side Effects
Oxazolam, like most other benzodiazepines, is classified under the Controlled Substance Act (CSA) as a Schedule IV substance. This classification denotes a compound that has recognized medical uses but still carries the potential for misuse as well as the capacity to cause physical dependence and withdrawal symptoms, albeit to a lesser degree than substances classified as Schedule III.
According to their classifications under the CSA, benzodiazepines are supposedly less dangerous than other substances like cannabis, lysergic acid diethylamide (LSD), and psilocybin (magic mushrooms). However, if one takes a look at recent benzodiazepine misuse trends in the United States, the statistics paint quite a different picture.
For instance, the National Institute on Drug Abuse (NIDA) conducted a recent study that showed how 16% of opioid overdoses also contain some form of benzodiazepine presence [2]. Another 2020 study, this time by the CDC, can help us put these figures into context; it concluded that, in that year, benzodiazepines were involved in a total of 12,190 deaths in the United States.
When it comes to the specific contributions of oxazolam and nordiazepam and their own individual risk levels, it’s hard to come up with worthwhile conclusions. Oxazolam is not approved as a medication in the United States, so its risk factors are not really relevant. And with regards to nordiazepam, the amount of prescriptions is so low that it cannot be considered to meaningfully contribute to benzodiazepine-related fatalities.
Side Effects of Oxazolam
There is very little peer-reviewed information to be found on the adverse effects of nordiazepam.
Oxazolam has been found to have the following side effects:
- Altered libido
- Amnesia
- Ataxia
- Blood and lymphatic system disorders
- Blood dyscrasias
- Blurred vision
- Disorientation
- Drowsiness
- Dysarthria
- Gastrointestinal disturbances
- Hallucinations
- Headache
- Hypotension
- Irritability
- Leucopenia
- Lethargy
- Muscle weakness
- Nausea
- Restlessness
- Salivation changes
- Skin rashes
- Slurred Speech
- Suicidal ideation
- Syncope
- Tremors
Benzodiazepine Withdrawal & Dependence
In the medical world, it is common knowledge that, although rare, only benzodiazepines and alcohol withdrawals have the potential to become deadly. This is because tolerance to benzodiazepines and alcohol involves a combination of reduced GABA receptor activity and increased glutamate activity. When combined with sudden discontinuation, these factors can result in an inability of the neurological system to regulate hyperactive states. In essence, excessive glutamate levels, when left unchecked by GABA, can lead to excitotoxicity, neuronal damage, and even death.
This level of risk entails that doctors have to be careful when prescribing benzodiazepines. The general rule of thumb is to prescribe them for the minimum amount of time possible, and even then, they can still cause physical dependence.
Several studies indicate that even when used for a short period of time, benzodiazepines have a considerable potential to induce dependence and symptoms of withdrawal. One study, for instance, concluded that approximately one-third of individuals who use benzodiazepines for longer than four weeks experienced dependence and withdrawal symptoms after ceasing their treatment [3].
Harm Reduction: Oxazolam
When dealing with prescription drugs like benzodiazepines, there are several harm reduction principles that users should be aware of in order to minimize risk. Some of these recommendations might sound obvious, but at the end of the day, those are the ones that are the most effective.
First and foremost, there are also several methods that users should consider before they even try to attain a benzodiazepine prescription. As we have seen, benzodiazepines have a considerable risk profile, and it would be foolish not to consider viable non-pharmacological options to solve whatever ailment is troubling them. Behavior-oriented therapy, counseling, and plant-based medications work for a great number of people.
However, if a user is set on using benzodiazepines, then they should strive to avoid any and all misuse, which means they should not use benzodiazepines if they do not have a prescription, and they should only use said benzodiazepines in strict accordance with their prescriptions. Also, be aware that misuse is not synonymous with engaging in recreational use. For example: even if it is not done for recreational purposes, taking your benzodiazepine at the wrong time or unilaterally increasing the dosage is still considered misuse.
Lastly, users should also keep in mind the following rules which apply to all prescription drugs: the more a drug is consumed and the longer it is consumed, the more chance there is that dependence will develop; also, if a user has a history of abusing drugs or alcohol, their chance to misuse a prescription raises considerably.
Harmful Interactions
Benzodiazepines are central nervous system (CNS) depressants, which means that a couple of drug interactions will always cause serious risks to a user. These drug interactions would be the concomitant use of opioids, alcohol, and other benzodiazepines. However, in reality, the use of any other CNS depressant drug, like the kratom plant, for example, would also be a major cause for concern.
This is due to the fact that combining compounds that exert a depressive effect on the CNS is a major cause of respiratory depression: the leading cause of death among drug overdoses. Recent trends in drug fatalities in the United States should be more than enough of an example to show how dangerous this effect can be. In response to the situation, the FDA has issued several warnings about the dangers of concomitant CNS depressant use.
Users should also be aware of the potential of other drugs to affect the CYP-mediated metabolism of their given benzodiazepine.
The CYP enzyme system is responsible for metabolizing a large percentage of pharmacological compounds, and this means that drugs that either induce or inhibit the performance of these enzymes can end up affecting the metabolism of a benzodiazepine drug within the user’s system. This can lead to the drug building up in the body over time, which can raise risk levels, or it can lead to an accelerated metabolic process, which decreases the benzodiazepine’s effectiveness.
Contraindications
Most benzodiazepines will have a series of associated contraindications. These usually relate to special statutes like pregnancy and hepatic impairment, but many times they can also be found in connection to esoteric conditions and drug combinations, so always make sure to check with your doctor because you might be exposing yourself to risk in this way.
The contraindications listed for oxazolam are:
- Acute pulmonary insufficiency
- Chronic psychosis
- Hepatic insufficiency
- Hypersensitivity to benzodiazepines
- Lactation
- Myasthenia gravis
- Pregnancy
- Sleep apnea syndrome
Proper Dosage
If a user wants to reduce risk levels, then the proper dosage is a factor they should always be in control of. When it comes to oxazolam, the common dosage is 10-25 mg.
Similar Benzodiazepines
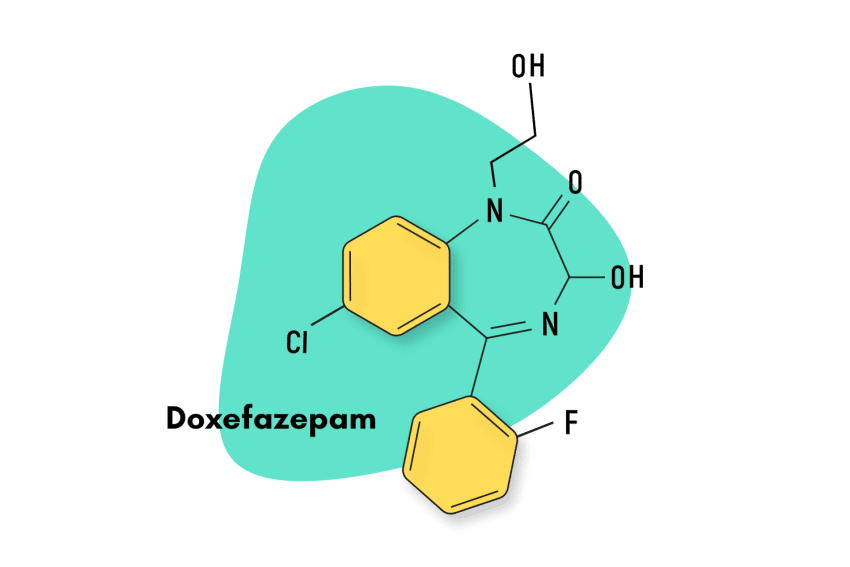
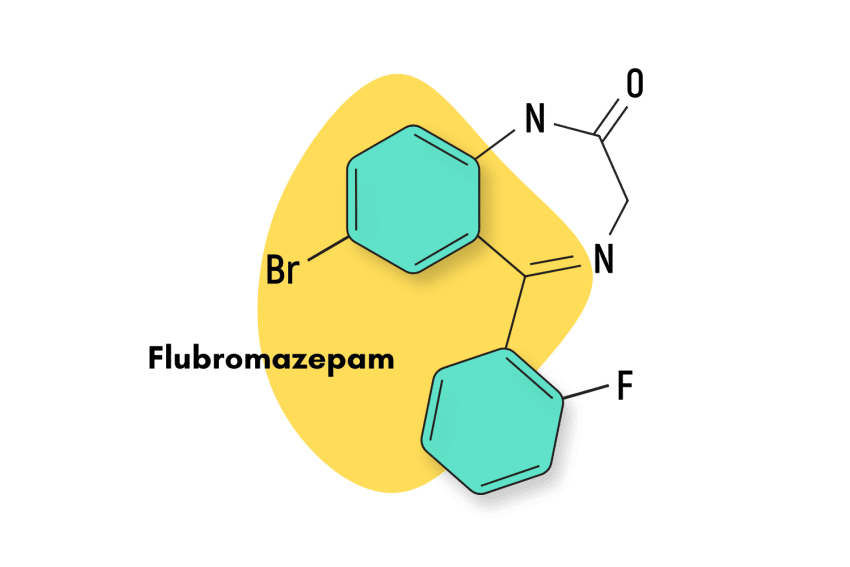
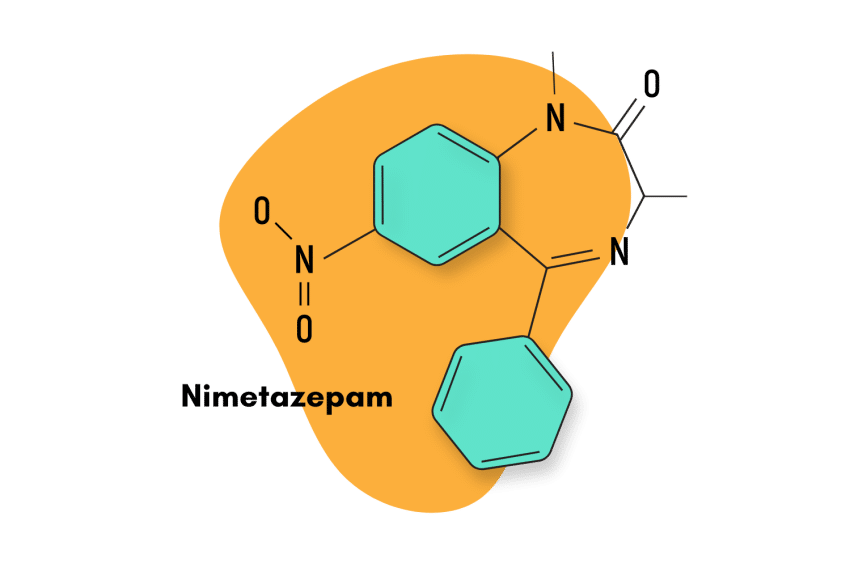
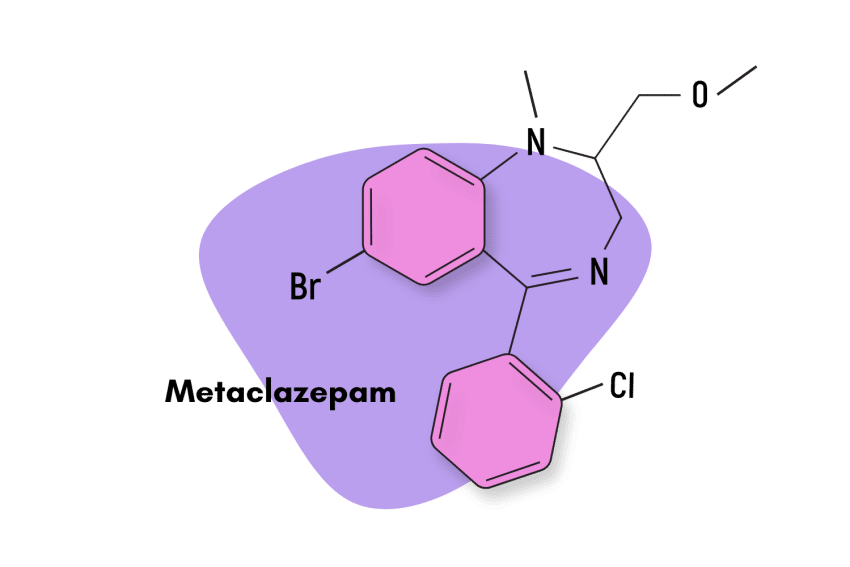
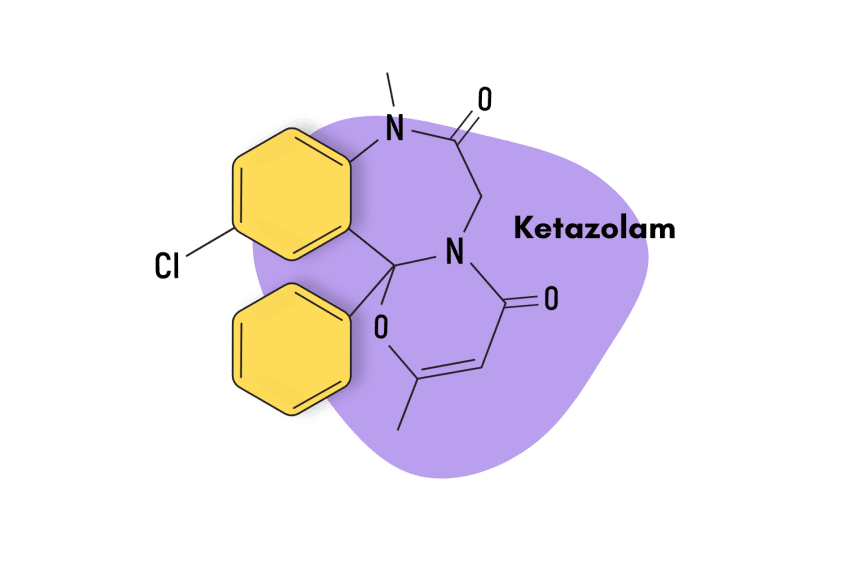
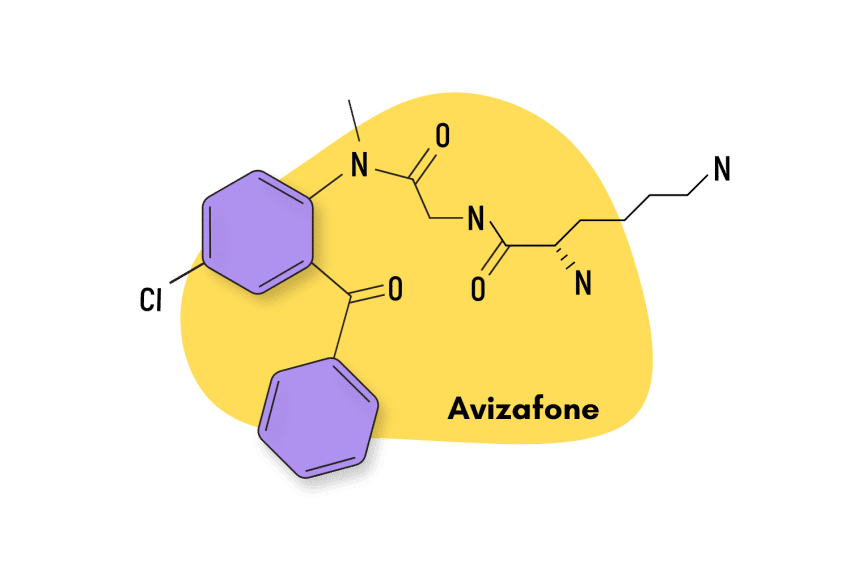
As a 1,4 benzodiazepine, oxazolam has similarities with a wide breadth of classical benzodiazepines.
Nordiazepam
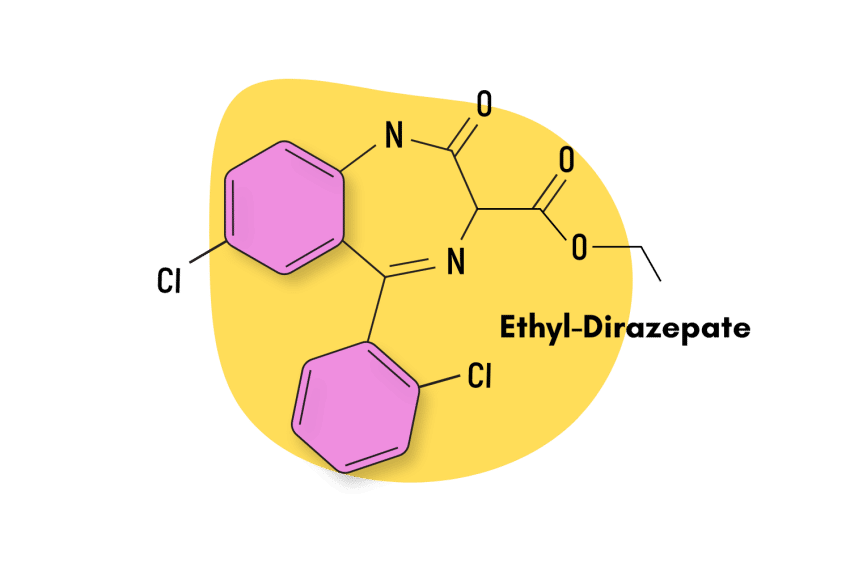
Oxazolam is a prodrug of nordiazepam, which means it has a pharmacological profile that is nearly identical to that of the former. However, there are meaningful differences when it comes to their pharmacokinetics, as oxazolam is short-acting, and nordiazepam is one of the longest-lasting benzodiazepines.
Diazepam
Nordiazepam, the drug which oxazolam metabolizes into, is itself a metabolic product of diazepam, one of the most popular benzodiazepines on the market. As such, they have similar characteristics in terms of pharmacology.
Alternatives to Benzodiazepines
For those looking to get off pharmacological benzodiazepines, there are several plant-based alternatives that can offer comparable effects.
For instance, valerian root is known to house a variety of compounds that also potentiate the natural effects of GABA receptors: just like benzodiazepines [4]. The compounds found in valerian root also produce an allosteric effect, but they are known to interact with GABA receptors in other ways too.

Another alternative is L-theanine, a natural ingredient found in green and black tea. Studies have shown that L-theanine induces feelings of calm and relaxation by increasing the concentrations of GABA, as well as other key neurotransmitters [5]. The effects aren’t as potent as with pharmacological benzodiazepines, but the risk profile is a lot less severe.
References
- Gobbi, M., Barone, D., Mennini, T., & Garattini, S. (2011). Diazepam and desmethyldiazepam differ in their affinities and efficacies at ‘central’ and ‘peripheral’ benzodiazepine receptors. Journal of Pharmacy and Pharmacology, 39(5), 388–391. https://doi.org/10.1111/j.2042-7158.1987.tb03404.x
- Benzodiazepines and Opioids. (2022, November 7). National Institute on Drug Abuse. https://nida.nih.gov/research-topics/opioids/benzodiazepines-opioids
- Riss, J., Cloyd, J., Gates, J., & Collins, S. (2008). Benzodiazepines in epilepsy: Pharmacology and pharmacokinetics. Acta Neurologica Scandinavica, 118(2), 69–86. https://doi.org/10.1111/j.1600-0404.2008.01004.x
- Patočka, J., & Jakl, J. (2010). Biomedically relevant chemical constituents of Valeriana officinalis. Journal of Applied Biomedicine, 8(1), 11–18. https://doi.org/10.2478/v10136-009-0002-z
- Nathan, P. J., Lu, K., Gray, M., & Oliver, C. (2006). The Neuropharmacology of L-Theanine (N-Ethyl-L-Glutamine): A Possible Neuroprotective and Cognitive Enhancing Agent. Journal of Herbal Pharmacotherapy, 6(2), 21–30. https://doi.org/10.1080/J157v06n02_02