Highs & Lows: How Marijuana Affects the Brain
Is marijuana a friend or foe of the brain? The answer is complicated, like a Facebook relationship status.
It’s difficult to find a meatier subject in the cannabis space than “how marijuana affects the brain.”
These effects are complicated, and we’ve only just scratched the surface of our understanding of their relationship.
Marijuana can have a positive impact on the brain; you can tell by looking at studies evaluating its neuroprotective and antioxidative properties [1]. Some researchers argue that cannabis may prevent the onset of neurodegenerative diseases like Alzheimer’s [2].
Neuroscientist Gary Wenk, the author of the book “Your Brain on Food,” claims that consuming one joint on average once you enter your 30s can significantly reduce the risk of excessive neurodegeneration [3].
But on the other hand, we have evidence that in some people, marijuana may cause a slight cognitive decline, especially when abused.
This article will help you understand how marijuana affects the brain, including individual differences, confounding factors, and patterns of use.
The Endocannabinoid System & its Role in the Brain
The endocannabinoid system (ECS) is a complex network of neurotransmitters, receptors, and enzymes that occur throughout the body — including the brain.
The main function of the ECS is to regulate essential physiological processes in order to maintain homeostasis (balance) in the body [4].
The ECS has two types of receptors:
1. CB1 Receptors
These receptors occur in high concentrations in the brain and central nervous system. Some are also found in the peripheral nervous and immune systems. They mostly regulate cognitive processes and are responsible for pain perception, mood, emotional stability, and motor function [5].
2. CB2 Receptors
These receptors are mostly found in the immune system, blood, and organs. The CB2 receptor is involved in regulating inflammation, pain responses, metabolism, and cell death [6].
When these receptors are activated by endocannabinoids — anandamide and 2-AG — they modulate the release of certain neurotransmitters, such as GABA, serotonin, and dopamine, which influence mood, reward, decision-making, focus, and cognition.
The ECS is involved in most aspects of brain function, including learning, memory, appetite, and sensory perception, and is the key catalyst of marijuana’s effects on the brain.
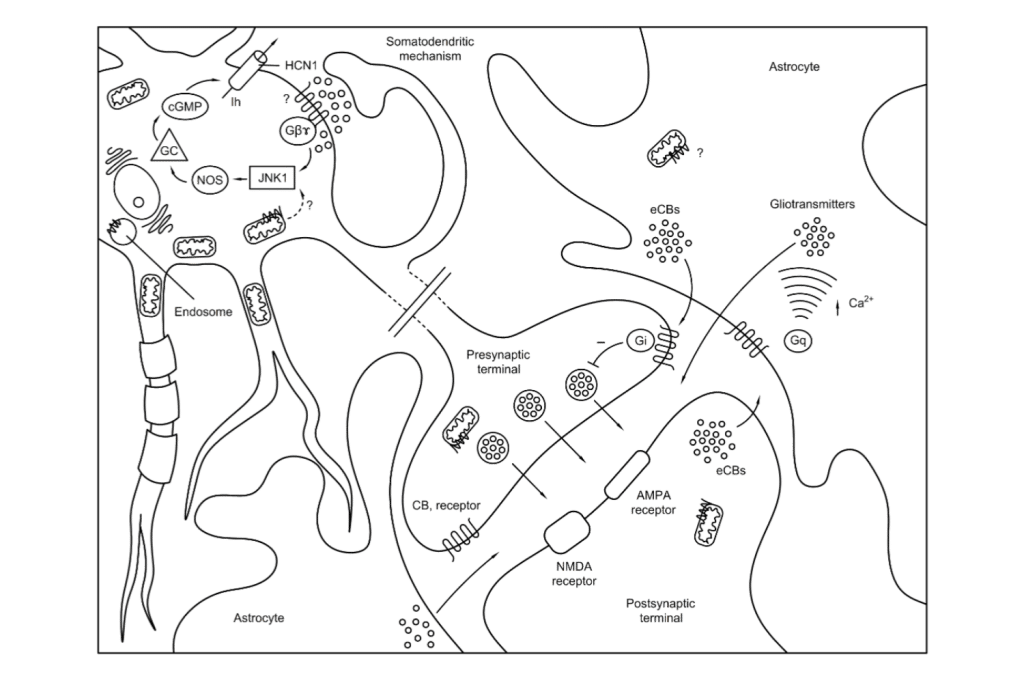
The Effects of THC (Tetrahydrocannabinol) on the Brain
THC (tetrahydrocannabinol) is the primary psychoactive cannabinoid in marijuana. It has a strikingly similar molecular structure to anandamide — the endocannabinoid that activates CB1 receptors in the brain.
In other words, your brain produces its own THC, but in “sustainable” amounts.
When you use marijuana, THC enters your bloodstream and mimics the actions of anandamide.
The brain gets fooled that more anandamide is circulating in your bloodstream.
Marijuana’s signature effects include:
- Euphoria
- Calmness
- Increased appetite
- Sharpened senses
- Reduced pain
- Altered perception of time
The exact effects of marijuana on your brain — and potential adverse reactions — are dosage-dependent.
It’s also worth noting that THC has a biphasic nature, meaning that low and high doses produce opposite effects.
Short-Term Effects of Marijuana on the Brain
When you get high on weed, your brain experiences bliss. Your thinking patterns change — and so does the perception of your thoughts, time, and surroundings.
Intoxication with THC also leads to short-term impairments in low-tolerance users, such as [7]:
- Selective short-term memory
- Confusion
- Issues with coordination
- Dry mouth
- Red eyes
- Sudden appetite influx
If you’re sensitive to THC and take too high a dose, you may experience its biphasic nature.
When triggered, THC may backfire and cause anxiety, paranoia, increased heart rate, and a drop in blood sugar, also known as greening out.
Long-Term Effects of Marijuana on the Brain
Up until recently, scientists have followed the notion that the long-term use of marijuana negatively affects the brain.
The greatest concerns point to the following:
- Short-term memory impairment
- Slight cognitive decline
- Increased risk of anxiety and depression
- Addiction
- Loss of motivation

Studies Give Conflicting Results on How Marijuana Affects the Brain
A large body of previous research was biased due to marijuana’s status as a Schedule I drug. The scheduling assumed that cannabis has no medical value and a high potential for abuse.
But when you use reverse engineering, the fact so many depressed people use cannabis doesn’t mean weed causes depression.
Looking at the antioxidative, anti-inflammatory, and antidepressant properties, you can use reversed causality and suggest that people with depression use marijuana to treat symptoms and improve their quality of life.
Another example of that confusion is the motivational syndrome.
At least four high-quality studies published between 2021-2023 have debunked the amotivational syndrome theory regarding cannabis [8, 9].
The authors claimed previous studies didn’t control for confounding factors and used too small samples to draw their conclusions.
When it comes to marijuana and memory, the largest meta-analysis to date concludes that these effects are yet to be fully understood and require a better understanding of individual differences between cannabis users [10].
According to the WHO, cognitive declines caused by marijuana abuse should diminish within 72 hours of starting abstinence [11].
Does Marijuana Have Medical Benefits?
Yes, there’s compelling evidence that marijuana is a versatile plant medicine.
The endocannabinoid system is involved in the pathophysiology of various disorders and diseases. According to E.B. Russo, our society is deficient in endocannabinoids, and some individuals even have clinical endocannabinoid deficiencies (CECD) [12].
It’s no wonder that cannabinoids and terpenes from marijuana can help level these deficiencies and put your body on the right track to regain homeostasis.

Evidence Supporting Marijuana Use for Various Medical Conditions
Marijuana was widely used by Western medicine practitioners between 1850-1937. Doctors would prescribe cannabis-based medicines for a wide range of ailments. It was ultimately included in the United States pharmacopeia.
Current evidence supports the use of marijuana for the following health benefits:
1. Pain Relief
People have been using marijuana for centuries to alleviate pain. Modern research confirms it has remarkable analgesic properties. Today, doctors can recommend marijuana as an alternative to conventional painkillers, including opioids and non-steroidal anti-inflammatory drugs (NSAIDs) [13].
2. Anti-Inflammatory Effects
Both THC and CBD have been dubbed as novel anti-inflammatory drugs, making them useful for conditions such as arthritis, Crohn’s disease, multiple sclerosis, neuroinflammation, and autoimmune diseases [14].
3. Nausea & Vomiting
Cannabis has a long history as an antiemetic. It can reduce nausea and vomiting, especially in cancer patients undergoing chemotherapy or radiotherapy. THC is the primary compound responsible for these effects, but CBD may strengthen them in the entourage effect [15, 16].
4. Anxiety & Depression
Although marijuana can exacerbate anxiety in some individuals, current research suggests that it has an antidepressant and calming effect. Since marijuana shares many traits with psychedelics, the setting, and your current mental state are paramount for your experience [17].
5. Neurological Diseases
Marijuana has neuroprotective properties, making it beneficial for treating neurological conditions such as epilepsy, Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis [18].
6. Diabetes & Obesity
A recent review of the scientific literature concluded that marijuana could be a novel solution for diabetes and obesity by increasing basal metabolic rate, insulin sensitivity, and the amount of brown fat cells in your body [19].

Potential Risks & Side Effects of Using Marijuana for Medical Purposes
While marijuana has impressive medical potential, it also has side effects. Some of the risks associated with using marijuana for medical purposes include:
1. Impaired Cognition
Especially if you’re a new user and have a low tolerance to THC. These impairments include memory, attention, and motor function. Your tolerance will increase with time, so you won’t be high as a kite each time you use marijuana. However, it’s best to avoid driving a car or operating heavy machinery under the influence of THC.
2. Addiction and Dependence
You can get addicted to marijuana in the same way you can get hooked on other substances affecting your brain’s reward system (e.g., coffee). Around 9% of regular cannabis users can get addicted to weed. The addiction is solely behavioral, although you may experience signs of physical dependence when trying to quit. The number of people aged 12 and older seeking cannabis addiction treatment doesn’t exceed 1.1%, according to The Drug Policy Alliance.
3. Respiratory issues
Smoking marijuana can cause respiratory problems over time due to the presence of tar and carcinogens. Recent longitudinal studies controlling for confounders have found that smoking marijuana doesn’t reduce airflow in the lungs and doesn’t cause emphysema. However, it can cause lung infection and bronchitis, so it’s better to buy a vaporizer and minimize the harm.
4. Psychiatric Effects
According to some theories, marijuana use can speed up the onset of schizophrenia in genetically predisposed individuals. The jury is still out on whether it’s just correlation or causality.
5. Interactions with Other Medications
Marijuana can affect the liver’s ability to metabolize active ingredients in pharmaceutical medications. Depending on the type of interaction, marijuana can increase or decrease the concentration of the drug in your bloodstream, causing either a subtherapeutic effect or increasing the risk of toxicity.

What Factors Influence How Marijuana Affects the Brain?
Several factors decide how marijuana affects the brain, including:
1. Dosage & Frequency of Use
Lower doses are more relaxing and promote neurogenesis without getting you high [20]. High doses will produce more intense and longer-lasting effects. The frequency of marijuana use affects your tolerance, meaning you won’t experience most of the side effects of intoxication. However, it increases your risk of dependence and behavioral addiction.
2. Cannabis Consumption Methods
The way you consume marijuana changes its effects on the brain. Smoking or vaping weed can result in almost instantaneous effects, while edibles can take up to 90 minutes to kick in.
3. THC:CBD Ratio
THC and CBD are the yin and yang of cannabis. CBD can counteract the psychoactive effects of THC, offsetting some of its unpleasant side effects, such as anxiety and paranoia. Most marijuana strains are low in CBD, but you can find several selectively-bred flowers out there that boast higher levels of this cannabinoid. Alternatively, try mixing your weed with some CBD hemp flower to modulate the ratios.
4. Individual Differences
Some people are more receptive and sensitive to the psychedelic nature of THC. Others have a naturally high tolerance and need higher doses to achieve the same effects. Individual factors, such as age, sex, genetics, and overall health, can change the way marijuana affects the brain.
5. Setting
Where you use marijuana and who you share it with have a profound impact on its effects. Smoking weed in a stressful environment or when you have hidden fears that you’ve broomed under the carpet may increase the risk of anxiety and paranoia.
Is Marijuana Addictive?
Although marijuana isn’t as addictive as alcohol, nicotine, or opioids, some people can still get addicted to it.
According to the National Institute on Drug Abuse (NIDA), around 9% of regular cannabis users will develop a cannabis use disorder.
The concept of addiction to marijuana revolves around behavioral addictions.
Related: Can Psychedelics be Used to Treat Addiction?
Understanding the Concept of Addiction
Marijuana affects your brain in various ways, but it doesn’t make you physically addicted.
Physical addiction occurs when withdrawal symptoms are so severe that they cause literal pain.
The spectrum of physical addiction symptoms ranges from bouts of aggression to depression, anxiety, panic attacks, severe pain in the muscles and bones, convulsions (sometimes epilepsy), and even suicidal ideation.
With marijuana, it’s a matter of behavioral addiction.
When you use marijuana frequently, you give your nervous system signals that this particular activity is important to you.
And since marijuana affects the brain’s reward circuit, every time you use it, your brain receives pleasure for doing nothing engaging.
If you simply smoke a bowl and vegetate on the couch, then you’re not doing anything constructive afterward, either.
That’s how you fry your dopamine receptors with cheap pleasure.
It’s similar to doom scrolling or checking your notifications on the phone every few minutes.
Who is More Likely to Get Addicted to Marijuana?
As mentioned earlier, some people are more prone to behavioral addiction. If you use cannabis responsibly and take tolerance breaks from time to time, your risk of getting addicted is low. But it increases proportionately to your emotional dependence on the plant.
You’re more likely to get addicted to marijuana if you:
- Start at an early age
- Frequently use large doses
- Have a personal or family history of substance abuse
- Don’t have a job, hobby, or a well-developed social life
According to Carl Hart, a neuroscientist, and professor of psychology at Columbia University, people who abuse marijuana regulate certain behaviors that normally make people happy and fulfilled.
When you look at people who are addicted to marijuana and compare them with those who aren’t, you’ll notice that the latter have a good job, a hobby, a loving partner, and good relations with their family.
Something which the former often lack — hence that compensation mechanism with marijuana.
Withdrawal Symptoms from Marijuana Use Disorder
Withdrawal symptoms affect individuals who use marijuana frequently and in large doses. Doing so leads to the overstimulation of the cannabinoid receptors in the brain.
The endocannabinoid system must return to its normal function and shape; withdrawals are indicators of that comeback.
Common withdrawal symptoms of marijuana use include:
- Irritability — you may have a short fuse for the first few days of withdrawal.
- Anxiety — marijuana has anxiolytic properties, so withdrawing may cause heightened feelings of anxiety.
- Insomnia — you may experience difficulty falling asleep on top of some crazy dreams because nothing affects your REM sleep stage anymore.
- Appetite fluctuation — marijuana gives you munchies. By the same token, withdrawing from it may lead to decreased appetite.
- Low mood — some individuals may go through depressive episodes, feeling sad, unmotivated, and hopeless.
- Physical symptoms — hot flashes and sweaty hands are typical symptoms within the first few days of withdrawing.
Not everyone who uses marijuana will experience withdrawal symptoms. Their duration and severity also differ between individuals and depend on factors like the potency of marijuana, the patterns of use, and individual differences in brain chemistry.
They hit their peak in the first week of abstinence and generally dissipate afterward. You shouldn’t experience any withdrawals after 2-3 weeks from starting abstinence.
What is Marijuana?
Marijuana is an informal name for plants from the Cannabis sativa L. genus. It contains chemicals called cannabinoids, including delta-9-tetrahydrocannabinol (THC), cannabidiol (CBD), and over 100 other similar compounds.
The effects of marijuana on the brain depend on the overall phytochemical profile of the strain.
Cannabinoids, terpenes (aromatic molecules), and flavonoids (they give plants their unique colors) work together to create a unique synergy known as the entourage effect.

Types of Marijuana Plants
There are three types of marijuana plants:
- Cannabis sativa — tall, slender plants growing in warm, tropical climates. Their effects are more energizing and better suited for daytime use.
- Cannabis indica — shorter and bushier plants native to the Asian continent. They produce relaxing and sedative effects, making them a decent option for evenings.
- Cannabis ruderalis — smaller than both indica and sativa, coming from Central and Eastern Europe. This type of marijuana plant is used for breeding hybrid strains; people rarely use it for recreational or medical purposes.
Today, there’s a myriad of hybrid strains between Sativa, Indica, and/or Ruderalis, which can produce different aromas, flavors, and effects.
Different Ways to Use Marijuana
Marijuana is a versatile plant; you can use it for smoking, vaping, or making DIY edibles and topicals.
1. Smoking
Smoking is the oldest and most common form of marijuana consumption. Due to the use of high temperatures, more cannabinoids enter your body in a short time span. This ensures more intense effects, but it also delivers harmful substances from combustion, not to mention that some cannabinoids and terpenes are lost in the process.
2. Vaporization
It’s a smokeless method of inhaling cannabinoids and terpenes in the form of warm vapor. The active ingredients are released gradually, and the device allows for precise temperature control. It’s the go-to consumption method for medical marijuana patients and health-conscious recreational users.
3. Edibles
Arguably the funniest way to enjoy the buzz. Edibles are stronger because THC converts into a more potent metabolite in the liver (11-hydroxy-THC). However, they have a delayed onset, meaning you’ll need to wait 30-90 minutes before they kick in.
4. Tinctures
Tinctures are taken under the tongue; they get absorbed through the capillary glands under the tongue. Since the tincture avoids the liver, the effects take hold faster — usually around 15-20 minutes.
5. Topicals
This form of marijuana doesn’t affect the brain because the THC doesn’t reach the bloodstream. Instead, it binds to cannabinoid receptors in the epidermis layer of the skin, providing localized relief from pain and other types of physical discomfort.
References
- Hampson, A. J., Grimaldi, M., Lolic, M., Wink, D., Rosenthal, R., & Axelrod, J. (2000). Neuroprotective antioxidants from marijuana. Annals of the New York Academy of Sciences, 899, 274–282.
- Kim, S. H., Yang, J. W., Kim, K. H., Kim, J. U., & Yook, T. H. (2019). A Review on Studies of Marijuana for Alzheimer’s Disease – Focusing on CBD, THC. Journal of Pharmacopuncture, 22(4), 225–230.
- Wenk, G. (2016). Using Marijuana to Prevent Alzheimer’s Disease. Psychology Today.
- Kaur, R., Ambwani, S. R., & Singh, S. (2016). Endocannabinoid System: A Multi-Facet Therapeutic Target. Current clinical pharmacology, 11(2), 110–117.
- Kendall, D. A., & Yudowski, G. A. (2017). Cannabinoid Receptors in the Central Nervous System: Their Signaling and Roles in Disease. Frontiers in cellular neuroscience, 10, 294.
- Turcotte, C., Blanchet, M. R., Laviolette, M., & Flamand, N. (2016). The CB2 receptor and its role as a regulator of inflammation. Cellular and molecular life sciences: CMLS, 73(23), 4449–4470.
- Kroon, E., Kuhns, L., & Cousijn, J. (2021). The short-term and long-term effects of cannabis on cognition: recent advances in the field. Current opinion in psychology, 38, 49–55.
- Gage, S. H., Jones, H. J., Burgess, S., Bowden, J., Davey Smith, G., Zammit, S., & Munafò, M. R. (2017). Assessing causality in associations between cannabis use and schizophrenia risk: a two-sample Mendelian randomization study. Psychological medicine, 47(5), 971–980.
- Pasman, J. A., Verweij, K. J. H., Gerring, Z., Stringer, S., Sanchez-Roige, S., Treur, J. L., Abdellaoui, A., Nivard, M. G., Baselmans, B. M. L., Ong, J. S., Ip, H. F., van der Zee, M. D., Bartels, M., Day, F. R., Fontanillas, P., Elson, S. L., 23andMe Research Team, de Wit, H., Davis, L. K., MacKillop, J., … Vink, J. M. (2018). GWAS of lifetime cannabis use reveals new risk loci, genetic overlap with psychiatric traits, and a causal influence of schizophrenia. Nature Neuroscience, 21(9), 1161–1170.
- Burggren, A. C., Shirazi, A., Ginder, N., & London, E. D. (2019). Cannabis effects on brain structure, function, and cognition: considerations for medical uses of cannabis and its derivatives. The American Journal of Drug and alcohol abuse, 45(6), 563–579.
- Medina, K. L., Hanson, K. L., Schweinsburg, A. D., Cohen-Zion, M., Nagel, B. J., & Tapert, S. F. (2007). Neuropsychological functioning in adolescent marijuana users: subtle deficits detectable after a month of abstinence. Journal of the International Neuropsychological Society: JINS, 13(5), 807–820.
- Russo E. B. (2016). Clinical Endocannabinoid Deficiency Reconsidered: Current Research Supports the Theory in Migraine, Fibromyalgia, Irritable Bowel, and Other Treatment-Resistant Syndromes. Cannabis and cannabinoid research, 1(1), 154–165.
- Bains S, Mukhdomi T. Medicinal Cannabis For Treatment Of Chronic Pain. [Updated 2022 Dec 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
- Nagarkatti, P., Pandey, R., Rieder, S. A., Hegde, V. L., & Nagarkatti, M. (2009). Cannabinoids as novel anti-inflammatory drugs. Future medicinal chemistry, 1(7), 1333-1349.
- Parker, L. A., Rock, E. M., & Limebeer, C. L. (2011). Regulation of nausea and vomiting by cannabinoids. British Journal of Pharmacology, 163(7), 1411–1422.
- Russo E. B. (2011). Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. British Journal of Pharmacology, 163(7), 1344–1364.
- Li X, Deviant JP, Stith SS, Brockelman F, Keeling K, Hall B, Vigil JM. The Effectiveness of CannabisFlower for Immediate Relief from Symptoms of Depression. Yale J Biol Med. 2020 Jun 29;93(2):251-264. PMID: 32607086; PMCID: PMC7309674.
- Milano W (2018) Neuroprotection by Cannabinoids in Neurodegenerative Diseases,
- Cavalheiro, E. K. F. F., Costa, A. B., Salla, D. H., Silva, M. R. D., Mendes, T. F., Silva, L. E. D., Turatti, C. D. R., Bitencourt, R. M., & Rezin, G. T. (2022). Cannabis sativa as a Treatment for Obesity: From Anti-Inflammatory Indirect Support to a Promising Metabolic Re-Establishment Target. Cannabis and cannabinoid research, 7(2), 135–151.
- Prenderville, J. A., Kelly, Á. M., & Downer, E. J. (2015). The role of cannabinoids in adult neurogenesis. British journal of pharmacology, 172(16), 3950-3963.