Ketamine for Sedation: Risks, Applications, & How it Works
Ketamine’s sedative effects are sought after by recreational users and medical professionals.
Ketamine has long been used both in medicine and recreationally for its sedative effects. It was developed as an anesthetic, so ketamine is used for a variety of medical procedures.
Ketamine causes almost total amnesia while also being a potent painkiller. Combined with its strong safety profile, minor effects on breathing, and ability to increase blood pressure and heart rate, ketamine is an ideal anesthetic for short procedures that may be painful or uncomfortable.
Ketamine Sedation Mechanism of Action
Ketamine has a long list of interactions and potential mechanisms of action in the body. The sedative effects are rapid, occurring in seconds after injection.
The sedative effects are, at least in part, through interaction with NMDA (N-methyl-D-asparate) receptors in the brain [1]. When ketamine (and its metabolites) bind to NMDA receptors, a neurotransmitter called glutamate cannot bind to the receptors.
One (of many) results is a change in the balance between glutamate, an excitatory neurotransmitter, and GABA, a neurotransmitter known as “the breaks” of the brain, which exerts a calming and sedative effect [2].
The above explanation is pretty simplified, though. More sedative effects may come from ketamine blocking sodium [3] and potassium channels [4], which, when blocked, slow electrical activity and excitability in the brain and induce anesthesia at high doses. Ketamine also interacts with muscarinic [5] and nicotinic [6] receptors, in turn affecting memory, heart rate, and blood pressure.
Ketamine Conscious Sedation Dose
The dose for ketamine sedation varies across individuals and methods of administration. Typically, ketamine is administered according to body weight, in milligrams per kilogram. In the case of very obese people, the dose may be calculated based on “ideal weight.”
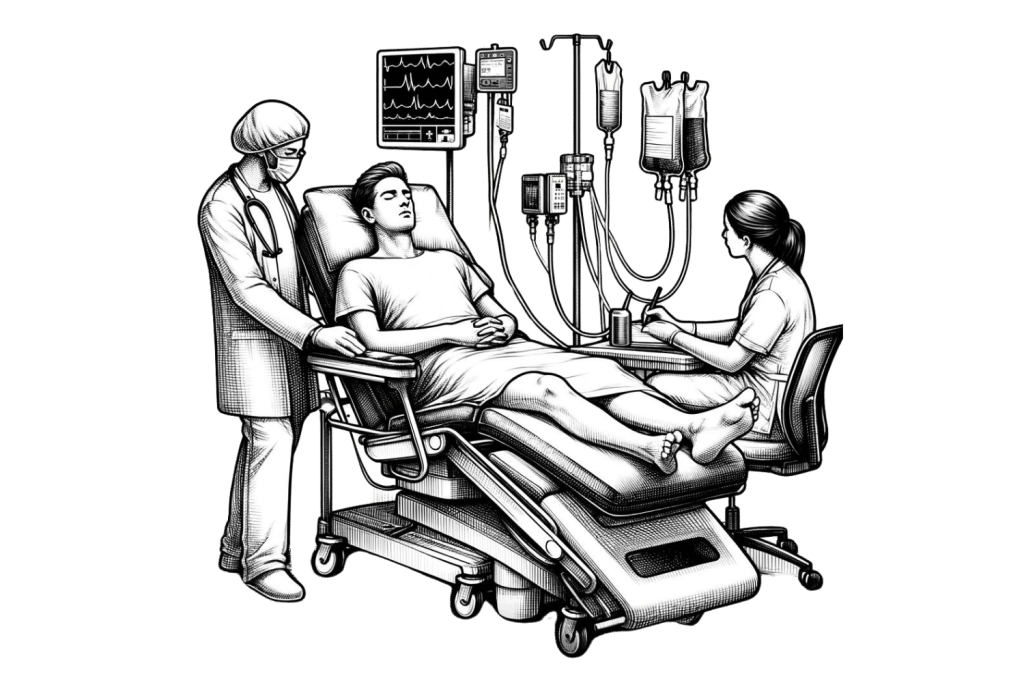
Intravenous or IV ketamine is the most bioavailable and effective method. Typically, a trained nurse or anesthesiologist will calculate the appropriate dose and administer the drug at the correct rate.
A “loading dose” or initial dose will often be given, followed by more doses or a drip to sustain effects.
One study puts loading anesthetic doses at [7]:
- Intravenous — 0.03 – 0.24 mg/kg
- Intramuscular — 3-4 mg/kg
There may be variations in the amounts above, depending on the level of sedation needed.
Infusions include a time element because, if given too quickly, ketamine can cause dangerous side effects, like apnea or cardiac issues.
Other methods of consumption include nasal spray and oral ketamine, which are used for sedation in children and sometimes adults.
Ketamine Sedation & Benzodiazepenes
Ketamine has long been known for its “emergence phenomenon,” also known as psychoactive effects. These shifts in mood and perception are attractive if you’re using it as a recreational drug, but in a medical setting, putting people in an altered state can cause problems.
Ketamine is frequently administered alongside benzodiazepines like diazepam and midazolam to help reduce adverse effects. Other anesthetics, like propofol, have been used alongside ketamine, along with painkillers like fentanyl.
A medical professional determines safe levels for these combinations and typically administers them with an IV.
Ketamine Sedation Contraindications
Medical professionals will determine if ketamine sedation is safe.
Anyone with the following should avoid ketamine:
- Pregnant or breastfeeding
- History of psychosis or schizophrenia
- Allergic to ketamine
- Anesthesia allergy
- Kidney or liver problems
- Uncontrolled hypertension
- Cardiovascular disease
- Substance abuse history
Ketamine Side Effects and Long-Term Effects
Ketamine sedation can come with side effects, including:
- Disassociation or floating
- Hallucinations
- Delirium
- Vivid dreams
- Nausea
- Headache
- Elevated heart rate and blood pressure
After sedation, effects like elevated heart rate and blood pressure tend to dissipate in a matter of hours.
Some effects may persist, such as:
- Memory defects
- Panic attacks
- Nausea Vomiting
- Sleepiness
- Cardiocasculvar stimulation
- Nightmares and vivid dreams
Persistent side effects after ketamine sedation may require medical attention. Immediately contact the appropriate professionals.
FAQs: Ketamine
There’s a lot more going on with ketamine than its sedative effects. While there’s too much to cover here, we’ll answer some of the most pressing questions we get asked about ketamine.
1. Is Ketamine Addictive?
When used within recommended parameters in a medical setting, ketamine poses little risk of addiction, particularly in comparison to drugs like opioids.
When used recreationally, ketamine poses a much greater risk. Abuse of ketamine, such as daily use, is associated with severe kidney, liver, and bladder problems.
Related: A Journey Through Ketamine Withdrawal
2. How Long Does Ketamine Sedation Last?
The duration of ketamine sedation depends on the dose, individual, and maintenance dosing.
Typically, a single IV push of ketamine will last 5-10 minutes. Continuous infusion will extend effects.
For intramuscular (IM) administration, the effects last a bit longer, around 12-25 minutes.
The above numbers are from MedScape, which also notes that an altered state may continue for 20 minutes after sedation effects have worn off.
3. Is Ketamine for Sedation Safe?
When administered by a professional at the recommended dose, ketamine sedation is safe.
In fact, ketamine is favored for its safety profile as it has lower kidney and liver toxicity than other anesthetics. Ketamine also does not depress respiration and heart rate to the extent other anesthetics do.
References
- Sleigh, J., Harvey, M., Voss, L., & Denny, B. (2014). Ketamine–More mechanisms of action than just NMDA blockade. Trends in anaesthesia and critical care, 4(2-3), 76-81.
- Pham, T. H., & Gardier, A. M. (2019). Fast-acting antidepressant activity of ketamine: highlights on brain serotonin, glutamate, and GABA neurotransmission in preclinical studies. Pharmacology & therapeutics, 199, 58-90.
- Frenkel, C., & Urban, B. W. (1992). Molecular actions of racemic ketamine on human CNS sodium channels. British journal of anaesthesia, 69(3), 292-297.
- Friederich, P., & Urban, B. W. (1999). Interaction of intravenous anesthetics with human neuronal potassium currents in relation to clinical concentrations. The Journal of the American Society of Anesthesiologists, 91(6), 1853-1853.
- Durieux, M. E. (1995). Inhibition by ketamine of muscarinic acetylcholine receptor function. Anesthesia & Analgesia, 81(1), 57-62.
- Furuya, R., Oka, K., Watanabe, I., Kamiya, Y., Itoh, H., & Andoh, T. (1999). The effects of ketamine and propofol on neuronal nicotinic acetylcholine receptors and P2x purinoceptors in PC12 cells. Anesthesia & Analgesia, 88(1), 174-180.
- Rosenbaum, S. B., Gupta, V., Patel, P., & Palacios, J. L. (2017). Ketamine.