An Easy Guide to Ketamine Therapy & Insurance: Is It Worth the Cost?
One form of ketamine has received FDA approval for treatment-resistant depression, but does that mean insurance companies cover it?
While telehealth, clinics, and even prescription ketamine options have advanced dramatically in popularity, insurance has been slow to adapt to it. While a growing number of providers include ketamine therapy as an option in their plans, it’s exceedingly uncommon.
Below, we’ll cover some major questions about ketamine therapy, including:
- Does Insurance Cover Ketamine Therapy?
- Is Ketamine an FDA-Approved Drug For Treatment?
- Does Insurance Cover FDA-Approved Ketamine Options?
- When is Ketamine Therapy Worth The Cost?
While the legality of ketamine therapy can make it seem exceptionally appealing, it’s often costly and requires repeated doses to maintain efficacy.
As ads run rampant about ketamine’s potential to treat depression, let’s talk about insurance and ketamine therapy — and if it’s even worth it in the first place.
Will Insurance Pay for Ketamine Therapy?
In most cases, ketamine treatment is not covered by insurance, but this isn’t always the case.
Healthcare plans can differ wildly, and various factors go into determining if insurance will cover ketamine therapy.
Factors determining insurance coverage include:
- Insurance Provider — Some providers see value in offering ketamine therapy treatment as a solution they pay for (at least partially). The cost for ketamine therapy every couple of months is likely less expensive than daily medication.
- Form of Treatment — Ketamine therapy takes various forms, including prescriptions, off-label injections, and more. Some of these may fall outside of coverage, while others don’t.
- Your Network/Plan — Insurance providers offer several options for coverage, but they often restrict treatment to a select pool of providers (your “network”). Clinics outside of this approved network are not likely covered, whereas others might be.
Even with all these variables in play, insurance companies are rarely willing to pay for ketamine. Since the majority of treatment solutions utilize “off-label” — or unapproved uses — ketamine, insurance companies typically refuse to accept it.
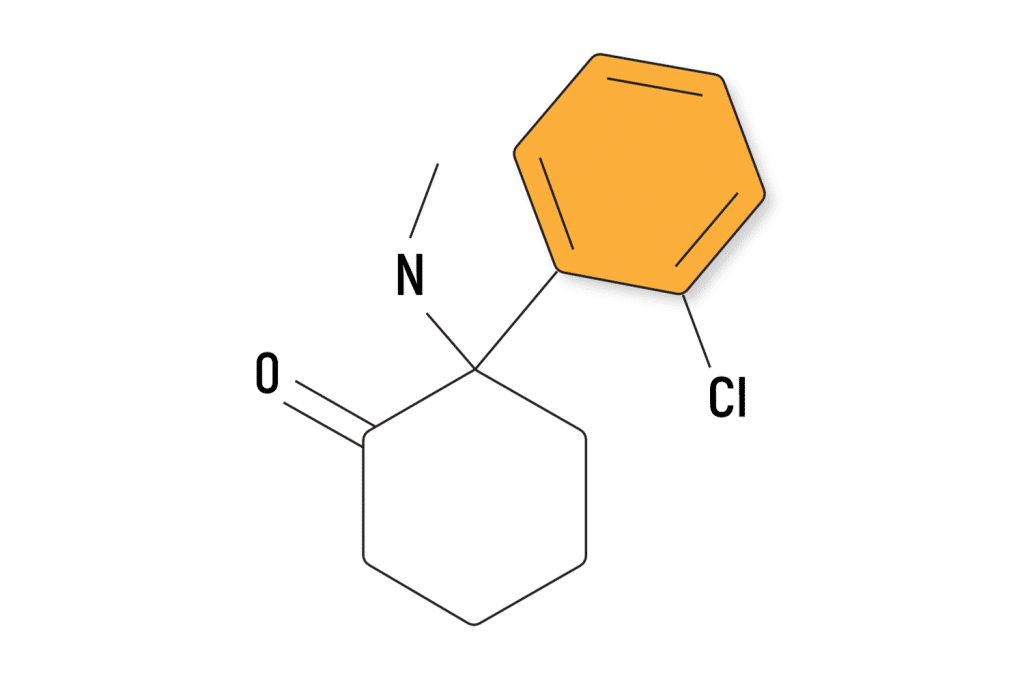
Is Ketamine Approved by the FDA?
Yes and no — technically, Spravato (a nasal spray from Johnson & Johnson) is the only form of ketamine the FDA approves of. This is an isolation of one of the two molecules (s-ketamine without its counterpart, r-ketamine) that make up standard racemic ketamine mixtures.
Spravato is an approved treatment for treatment-resistant depression (TRD), but other forms of ketamine are not included in this. However, since ketamine is a legal anesthetic, clinics can still easily obtain it and offer it for use outside of its intended purpose.
This creates a legal gray area where ketamine telehealth providers can mail lozenges of ketamine to nearly anyone willing to fill out a form and pay a small fee. On the other side of this battle are patients who may greatly benefit from ketamine therapy in a clinical setting but can’t afford it.
Will Insurance Pay for a Spravato Prescription?
As an approved treatment, Spravato is much more likely to be covered by your insurance provider, but it’s still not guaranteed. Your company may require you to hit a minimum amount of healthcare payments before it starts covering them; other times, it simply won’t cover them at all.
Spravato prescriptions typically involve 1–2 sessions with the nasal spray per week along with current depression medication, and the cost can get high quickly.

When Is Ketamine Therapy Worth the Money?
While ketamine’s rapid antidepressant action receives a lot of attention, its short-acting nature often goes unnoticed. Studies show a large percentage of people feel a dramatic alleviation of their depressive symptoms after even just a single dose; however, one study found an average time to relapse into depression of around 18 days [1].
This means most people have to return frequently to receive (often costly) treatments, and while studies often overlook this fact, repeated doses of ketamine can be quite dangerous. Ketamine carries an especially high potential for harm to urinary tracts — one study estimates over 20%, while another study claims 90% of users experience problems in this regard [2].
While more common in users who frequently consume large amounts of ketamine, the toxicity leading to this is worth considering before starting an ongoing ketamine treatment.
The second consideration is the level of care you’d like to receive. Some ketamine clinics offer therapeutic care and oversight during your sessions, but this is unlikely to happen for telehealth options (and the former costs much more).
These factors are important when deciding which therapy meets your needs. Ultimately, there are times when ketamine therapy can be the best choice, but it seems companies are inflating how often this is.
Some particularly good use cases for ketamine therapy may include:
Ketamine Therapy for Substance Use Disorder
Ketamine’s dissociative and pain-relieving qualities (theoretically) could be especially helpful for quenching drug cravings, while its psychedelic nature might assist mentally. Like all forms of ketamine therapy, this seems to be short-acting, with small, introductory studies showing low successful percentages after long-term follow-up without repeated dosing and therapeutic intervention [3].
“Addiction,” as we know it, is often a dramatic misinterpretation of what is happening when people are compulsively seeking drugs. Drs. Neşe Devenot et al. showed this when evaluating the successes of a smoking cessation study involving psilocybin, finding a shift in mindset was the determinant factor for success [4].
Still, ketamine’s rapid, short action makes it perfect for quickly finding relief and easily fitting it into their day. Of course, the research is inconclusive on how effective this is (particularly without therapy).
Ketamine Therapy for Suicidal Ideation
Suicidal ideation is often a recurrent symptom of depression that can appear suddenly, overwhelming people who experience it. Since this symptom usually occurs in cycles, ketamine’s lack of duration is less of a concern.
Additionally, as with the above, its rapid action and capability to easily fit into most days can be especially useful. However, this is one condition for which therapeutic care is especially important during your ketamine session.
Ketamine is not a guaranteed cure for anything, and dark thoughts aren’t going to necessarily vanish because of it. In some cases, the overwhelming effects of ketamine and negative visuals can worsen a condition.
Always take suicidal ideation seriously and follow the advice of a professional — none of whom would advise you to try to self-cure it by taking a potent psychedelic drug without any support.
Subscribe to Tripsitter: Newsletter & Podcast
Unlock Your Mind: Subscribe for Expert Insights on Psychedelics 🍄🌵
References
- Murrough, J. W., Perez, A. M., Pillemer, S., Stern, J., Parides, M. K., aan het Rot, M., Collins, K. A., Mathew, S. J., Charney, D. S., & Iosifescu, D. V. (2013). Rapid and Longer-Term Antidepressant Effects of Repeated Ketamine Infusions in Treatment-Resistant Major Depression. Biological Psychiatry, 74(4), 250–256. https://doi.org/10.1016/j.biopsych.2012.06.022
- Srirangam, S., & Mercer, J. (2012). Ketamine bladder syndrome: An important differential diagnosis when assessing a patient with persistent lower urinary tract symptoms. BMJ Case Reports, 2012, bcr2012006447. https://doi.org/10.1136/bcr-2012-006447
- Ivan Ezquerra-Romano, I., Lawn, W., Krupitsky, E., & Morgan, C. J. A. (2018). Ketamine for the treatment of addiction: Evidence and potential mechanisms. Neuropharmacology, 142, 72–82. https://doi.org/10.1016/j.neuropharm.2018.01.017
- Devenot, N., Seale-Feldman, A., Smith, E., Noorani, T., Garcia-Romeu, A., & Johnson, M. W. (2022). Psychedelic Identity Shift: A Critical Approach to Set And Setting. Kennedy Institute of Ethics Journal, 32(4), 359–399. https://doi.org/10.1353/ken.2022.0022