Kratom & Liver Damage: Is There Really That Much of a Risk?
We’re all about safety and will never ignore possible risks. But we’re also about truth and backing claims with science.
Can kratom cause liver damage? Possibly. Is it as big a deal as some people make it out to be? We wish there was a clear answer — or at least more information — but all we can do is provide the available facts. The conclusions are up to you.
This article looks at the most up-to-date research (mostly case reports, not studies), but you — and your doctor — will have to decide if kratom is safe for you.
Why the Research Falls Short
You can find a lot on how kratom causes liver damage, but the problem is that there’s nothing conclusive, and the evidence is sorely lacking.
Does that mean we should dismiss it? No, but it’s important to consider all angles.
1. It’s Mostly Case Reports
Most of the claims come from a handful of case reports (or case studies) instead of clinical studies.
These can be “used to explain, describe, or explore events or phenomena in the everyday contexts in which they occur” [1]. However, too many variables are at play, and they’re focused on isolated instances instead of large groups — randomized, blinded studies are considered the “gold standard.” [2]
The case reports lack a standardized causality assessment method. There is no set protocol for the tests done or for assessing the patient’s medical history and other possibilities that could contribute. Overall, there’s a lot of missing information, and the door is wide open to interpretation.
2. Animal Studies Used Unrealistically Large Doses
Currently, there are very few human studies — most kratom research is on animals.
Many (if not all) of these studies use vast amounts of mitragynine, much more than a person would take.
This makes it hard to accurately and realistically assess the risks. In forty-eight experiments, doses were higher than what even a heavy user would use — 100 mg/kg of mitragynine or 1000 mg/kg of kratom extract.
For the curious, these levels caused elevated liver enzymes and hepatic cellular damage but did not cause death. [3]
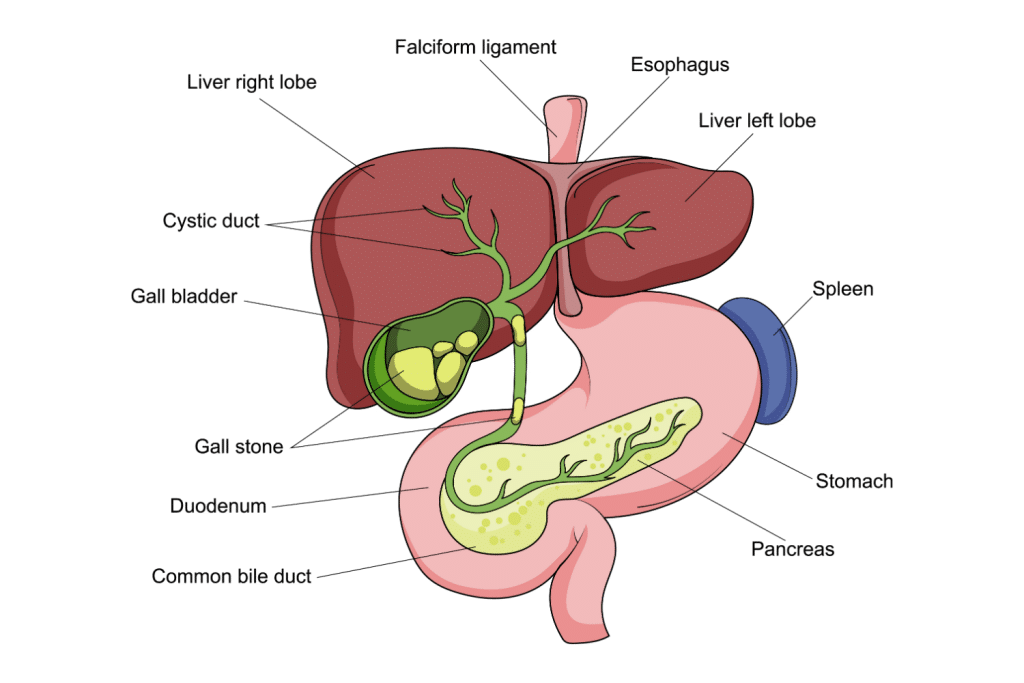
Kratom & Liver Damage: What Do the Studies Show?
I’ll mostly reference a recent review — Kratom (Mitragyna Speciosa) Liver Injury: A Comprehensive Review (Jan 9, 2020) [4]. The authors did all of the work for us and evaluated applicable epidemiologic, animal, mechanistic, and human reports relating to kratom and liver damage, using the Roussel Uclaf Causality Assessment (RUCAM) to determine hepatotoxicity in the case reports.
Here are the key points:
- Most users do not experience liver injury, though it’s likely underreported
- It’s unclear which user groups are at heightened risk
- There are no clear cases of death from kratom-induced liver injury
- Low-quality human evidence suggests kratom can cause liver injury
- Biopsies mostly show cholestatic injury
- Laboratory parameters show heterogeneous or mixed liver injury
- Animal studies are inconsistent, but some show high doses of kratom caused increased biochemical marker effects of liver injury.
- Patterns include centrilobular necrosis and bile duct proliferation
- We shouldn’t assume kratom-induced liver injury is an idiosyncratic reaction (a very rare drug reaction that doesn’t have to do with its therapeutic effects)
- Common symptoms of liver injury included jaundice, pruritis, dark urine, and abdominal discomfort; most liver problems showed up within 20 days of kratom use
- Treatments included N-acetyl cysteine (NAC), ursodiol, and glucocorticoids
- Most liver damage was reversed after the patient stopped using kratom
Acute Toxicity In High Doses
One study [5] looked at the effects of high doses of kratom extract on rats — 100 and 500 mg/kg did not significantly change the rats’ behavior, breathing, defecation, posture, or food and water intake, but 1000 mg/kg caused a significant decrease in their activity and produced rapid breathing lasting 30 minutes after administration.
There were no deaths, but the highest dose did cause severe hepatotoxicity after one dose.
Long-Term Effects & the Liver
Because kratom use is fairly new in the West, there’s not much to look at for research on its long-term effects.
A study published in 2019 found that liver injury from kratom use is rare but seems to be linked to high or chronic use [3]. It’s also possible that minor alkaloids or other substances in kratom could cause toxic effects in larger amounts [6].
Other studies note that health problems from kratom use tend to be more severe in North America than in other countries where it’s native. [7, 8]
Users who regularly chewed kratom leaves did not have more health complaints, and all kratom users were less likely to have a history of chronic diseases.
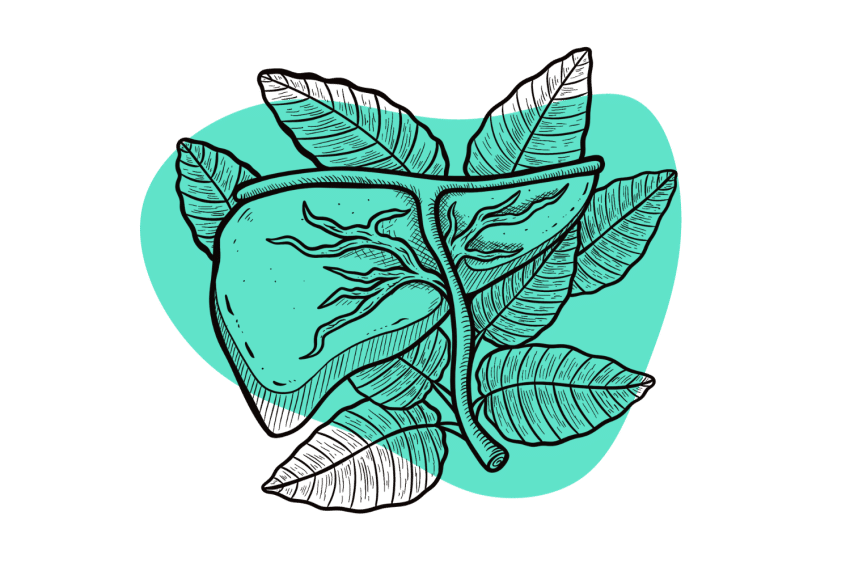
Kratom’s Effects On the Liver
The exact mechanism of how kratom could cause liver damage is unknown, but it could be related to liver enzyme polymorphisms — genetic variations that affect how a drug is metabolized — or something less complex, like how much kratom you take, how often you take it, and the method you use.
Kratom is metabolized mainly in the liver, but there haven’t been many studies on how it affects the hepatic transformers or the enzymes.
According to the review, there are several possibilities of how kratom could cause liver damage — thanks to its effects on the following. (The first two are at the top of their list. Which is why they’re at the top of ours.) [4]
- Pregnane X Receptor (PXR) Activation: This substance receptor regulates the drug-metabolizing enzymes and transporters and detoxification functions. Continuous activation could increase CYP3A4 expression, complicating the herb-drug interaction [9].
- Cytotoxicity: Research found kratom extract and mitragynine were cytotoxic to human neurons in vitro, and the enzyme CYP450 2E1 enhanced it.
- UDP Glucuronosyltransferases (UGTs): These perform glucuronidation in Phase 2 of the metabolic process. They bind to bilirubin and are a metabolic pathway for many drugs and endogenous substances, helping control their elimination. Unrealistically high doses of kratom mildly inhibited UGT activity in vitro in some instances but raised it in others. Mitragynine and 7-hydroxymitragynine also inhibited them, but again, the size of the doses made this clinically irrelevant.
- Glutathione S-transferases (GSTs): These are major Phase 2 detoxification enzymes. High concentrations of kratom extract inhibited them in vitro but inducted them at other times.
- P-glycoprotein (PgP): This multidrug transporter moves substances out of the cell and away from their target and is implicated in many drug-resistant diseases. Multiple studies show mitragynine inhibits it, and it’s suggested that this is partly why kratom interacts with many drugs.
These actions aren’t definitively linked to hepatotoxicity, but one theory is that they could create a greater risk due to other factors, like certain substances.

Kratom’s Side Effects & Risks — How to Avoid Them
Kratom has side effects beyond possible liver damage, but it’s relatively safe if you use it wisely — and the risks are mostly avoidable. You’ve probably heard otherwise, so let’s look at the details.
I’ll start by going over the risks and side effects that we know are linked to kratom. Unlike liver damage, these have been researched, at least more so. I’ll also tell you how to avoid them or give you the best shot at it.
1. Side Effects
Because so many prescription medications have nasty side effects, we can get a little nervous when we hear about them. Kratom won’t make you hemorrhage or have a loose(r) bladder.
In fact, kratom’s side effects are almost absurdly mild in comparison — partly because they go away as the kratom wears off — and include things like nausea, vomiting, dizziness, headaches, dehydration, anxiety, and insomnia.
How to avoid side effects:
Could these be severe? Well, sure, but it usually requires a larger dose or mixing it with other drugs, which I’ll cover. Most people don’t have to deal with these side effects when their dose is within a safe range (2-8 grams, depending on the individual and their needs) [10]. If you do end up nauseous, etc., try taking less next time.
2. Drug Interactions
Drug interactions could be kratom’s biggest downfall. Its alkaloids are metabolized by the same enzymes that take care of most medications (CYP450), meaning an interaction is very likely — and it can be deadly [11].
Whenever you hear about a death related to kratom, you can almost always assume another substance was involved, and it’s usually due to opioids (prescription and illegal; fentanyl is number one). Other offenders include cocaine, amphetamines, and benzodiazepines.
How to avoid drug interactions:
Do everyone a favor, and Don’t.Mix.Kratom.With.Oher.Substances. Even over-the-counter ones or herbal supplements. Talk to your doctor, do some research — whatever it takes to not go into it blindly.
3. Impure Products
In the US, kratom is like other herbal products in that there’s little oversight for its manufacturing or anything else. The FDA is pretty much hands-off despite its extreme dislike for the plant.
While I personally don’t mind them staying out of it, it makes for a dicey situation if you aren’t aware of the risks this imposes.
Anyone can buy kratom, package it, and sell it; there’s no legal obligation to label or test it. Some companies add things to boost the effects or sell moldy or contaminated kratom. There are stories of all of the above happening, so don’t write it off as an urban legend.
How to avoid contaminated or adulterated products:
Some states and other countries have passed laws to either outlaw it or implement regulations, but the majority have not.
Gas stations and head shops don’t generally have the best quality — or the best prices. Keep yourself safe and only buy from vendors that test their kratom and share the results. Plenty of online companies go the extra mile to prove their legitimacy, so don’t settle for less.
4. Addiction
Addiction is one of the top reasons people don’t like kratom. Because it’s an opioid receptor agonist, they assume it’s an opioid — and equally as dangerous.
However, kratom is an atypical opioid because it works on other receptors, making it much safer; it does not carry the same risks as opioids like morphine or oxycodone.
How to avoid addiction:
Limiting how much you use — in dosage and frequency — and taking the occasional break makes you less likely to become addicted. A good rule of thumb is to take a break from it for a few days every week.
And if you do end up struggling with addiction, the withdrawal is much milder than opioid withdrawal, and most people can go on with their lives, albeit uncomfortably. [10]
References
- Yin, R. K. (2009). Case study research: Design and methods (Vol. 5). Sage.
- Röhrig, B., Du Prel, J. B., Wachtlin, D., & Blettner, M. (2009). Types of study in medical research: part 3 of a series on evaluation of scientific publications. Deutsches Arzteblatt International, 106(15), 262.
- Veltri, C., & Grundmann, O. (2019). Current perspectives on the impact of Kratom use. Substance abuse and rehabilitation, 23-31.
- Schimmel, J., & Dart, R. C. (2020). Kratom (Mitragyna Speciosa) liver injury: a comprehensive review. Drugs, 80(3), 263-283.
- Harizal, S. N., Mansor, S. M., Hasnan, J., Tharakan, J. K. J., & Abdullah, J. (2010). Acute toxicity study of the standardized methanolic extract of Mitragyna speciosa Korth in rodent. Journal of ethnopharmacology, 131(2), 404-409.
- Kapp, F. G., Maurer, H. H., Auwärter, V., Winkelmann, M., & Hermanns-Clausen, M. (2011). Intrahepatic cholestasis following abuse of powdered kratom (Mitragyna speciosa). Journal of Medical Toxicology, 7, 227-231.
- Striley, C. W., Hoeflich, C. C., Viegas, A. T., Berkowitz, L. A., Matthews, E. G., Akin, L. P., … & McCurdy, C. R. (2022). Health effects associated with kratom (mitragyna speciosa) and polysubstance use: a narrative review. Substance abuse: research and treatment, 16, 11782218221095873.
- Saingam, D., Singh, D., Geater, A. F., Assanangkornchai, S., Jitpiboon, W., & Latkin, C. (2023). The Health Impact of Long-Term Kratom (Mitragyna Speciosa) Use in Southern Thailand. Substance Use & Misuse, 1-14.
- Basheer, L., & Kerem, Z. (2015). Interactions between CYP3A4 and Dietary Polyphenols. Oxidative medicine and cellular longevity, 2015, 854015.
- Henningfield, J. E., Chawarski, M. C., Garcia-Romeu, A., Grundmann, O., Harun, N., Hassan, Z., … & Huestis, M. A. (2023). Kratom withdrawal: Discussions and conclusions of a scientific expert forum. Drug and Alcohol Dependence Reports, 7.
- Tanna, R. S., Cech, N. B., Oberlies, N. H., Rettie, A. E., Thummel, K. E., & Paine, M. F. (2023). Translating kratom-drug interactions: from bedside to bench and back. Drug Metabolism and Disposition, 51(8), 923-935.