Psilocybin for Cluster Headaches: Current Research & Understanding
Cluster headaches cause sudden, severe pain to one side of the head and tend to come in repeating cycles lasting several weeks or months followed by a remission period.
This condition is debilitating, often leading to job loss or missed opportunities.
Anecdotal reports suggest psychedelics like magic mushrooms could offer a new form of treatment for this condition. While clinical research is lacking, there’s been several promising survey studies that confirm these effects.
Here’s everything we currently know about the use of magic mushrooms (and related psychedelics) for managing cluster headaches.
Can Psilocybin Help Prevent Cluster Headaches?
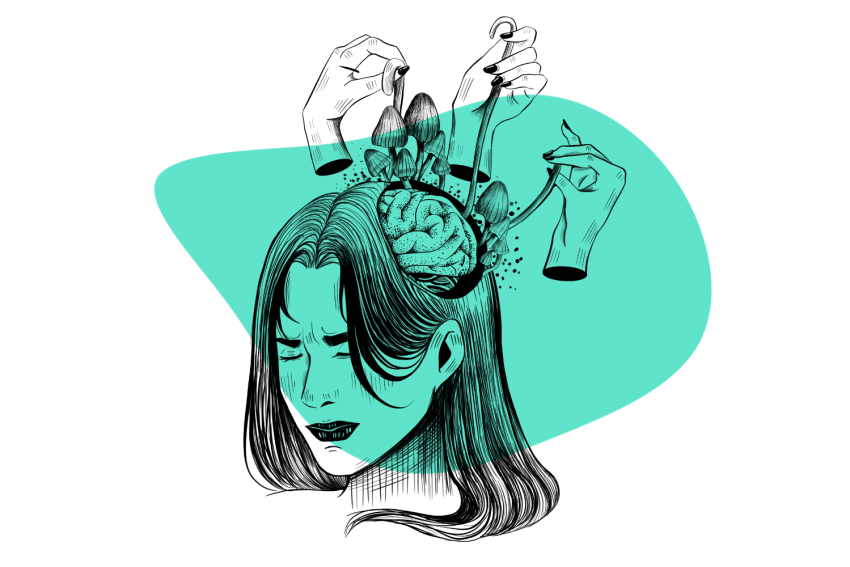
Psilocybin mushrooms appear to help prevent or reduce the severity of cluster headaches in some individuals, according to recent study findings. The mechanism for how they achieve this remains unknown.
A survey published in 2015 gave cluster headache sufferers (confirmed by a neurologist) a questionnaire seeking to find what treatments users were taking, and which ones worked for them, and which ones didn’t [2].
The study found that more than 50% of cluster headache sufferers (496 who took part in the study) experienced an improvement in their symptoms after using any of the indole-alkaloid psychedelics. This includes magic mushrooms, LSD, and LSA.
Here’s what the survey discovered:
- Psilocybin — most effective (33.7%
- Verapamil — second most effective (16.6%)
- LSA — 16.1%
- Steroids — 15.1%
- LSD — 6.5%
- Vitamins — 3.5%
Another study surveyed 53 cluster headache patients who had used either psilocybin or LSD to treat their condition [4]. Nearly 85% of people who took psilocybin experienced immediate symptoms relief. 52% of users who took psilocybin and 88% of users who took LSD reported remission of their condition.
While there haven’t been any significant clinical trials to study the use of psychedelics in a controlled setting, the results of these recent survey findings are significant and warrant further research.
What Are Cluster Headaches?
A cluster headache is defined as a severe headache affecting one side of the head. They normally appear in waves lasting 15 minutes to two hours in duration, most often at night or in the early hours of the morning.
The pain from these headaches can be severe. They’re sometimes referred to as “suicide headaches” because of how severe the pain can be.
The cause for cluster headaches is not well understood, but there are some clues as to its origin. Most cluster headache sufferers report some predictability in their attacks — usually at a certain period during the day, certain seasons of the year, or after exposure to certain smells, foods, alcohol, or stress.
Another key feature of cluster headaches includes alternating periods of attacks (cluster period) and remission. During a cluster period, attacks may take place every day or every couple of days. This is then followed by remission periods lasting several weeks or months in which no headaches appear.
There’s a lot we don’t know about cluster headaches. This condition is elusive and unpredictable. It’s estimated that most cases go undiagnosed and untreated, yet there’s a clear burden imposed by the condition.
A survey involving 1134 cluster headache sufferers found some intriguing results [3]:
- Nearly 20% of cluster headache respondents report having lost at least one job as a result of the headaches.
- 8% of respondents were out of work on disability currently as a result of the headaches.
- Beer is the most common alcohol trigger of cluster headaches.
- Weather changes and smells were reported as other common triggers.
- Suicidal thoughts were reported in 55% of respondents.
- Most of the people in the study had brown or blue eyes.
What Causes Cluster Headaches?
The cause for cluster headaches has eluded researchers — we still don’t know what’s actually causing this condition. But there are some clues for what may be involved.
The fact that most sufferers experience attacks in the early hours of the morning while asleep suggests the hypothalamus as a possible origin [1]. The hypothalamus is both our internal clock and the regulator of homeostasis in the body. It’s heavily involved with the regulation of our sleep/wake cycle, hormone production, neurotransmitter production, and more.
Unlike migraines, smells, alcohol, and foods aren’t as reliable of a trigger. Some people will experience attacks from exposure to certain compounds, but there’s enough variability in this that it’s not considered a reliable trigger.
Signs & Symptoms of Cluster Headaches
- Severe pain — usually focused behind or around one eye that radiates to the rest of the head and neck
- Pain on one side of the body only
- Restlessness and irritability
- Excessive tearing
- Stuffy or runny nose
- Increased sweating
- Drooping eyelids on the affected side of the head
- Flushing or pallor in the face
- Fatigue and lethargy
- Sensitivity to light and sound
Cluster Headaches vs. Migraines
Migraines and cluster headaches have a lot of similarities, but there are some key differences in these conditions.
The main difference with cluster headaches is the shorter duration and repetition of attacks. People affected by cluster headaches rarely experience attacks longer than an hour and a half but may experience new attacks every day or two.
Migraines are normally more sporadic — lasting up to three days but rarely appearing twice in the same week.
| Migraines | Cluster Headaches | |
| Severity of Pain | Moderate to Severe | Moderate to Severe |
| Duration of Attack | 4–72 hours | 15 minutes to 3 hours |
| Description of Pain | Throbbing Pain | Stabbing pain |
| Prevalence | Common — more than 37 million Americans affected | Rare — only 1 million Americans affected |
How Are Cluster Headaches Treated?
Treatment for cluster headaches is hit or miss. Some people find treatments that work; others have tried everything to no avail.
Conventional treatments for the condition include oxygen therapy (during acute attacks), a drug called Verapamil (calcium channel blocker), and corticosteroids.
Magic mushrooms are becoming a more popular form of treatment for the condition, usually used as a microdose whenever the first sign of attack starts to present. However, this isn’t an approved treatment. There’s still a lot of work to be done to assess both the safety of using psilocybin for cluster headaches, as well as the efficacy.
It’s not a good idea to take magic mushrooms if you’re on prescription medications for cluster headaches until you speak with your prescribing doctor first. While psilocybin itself is safe, the way it interacts with other substances or medications can be unpredictable and dangerous.
Can Psilocybin Cause Headaches?
Psilocybin can cause headaches too — which is ironic when there are so many reports of this compound “treating” some of the most severe and hard to treat types of headaches.
A study exploring this effect found that more than half of participants in the study reported a headache after the session [5]. The higher the dose, the more likely headaches were to result.
The good news is that these headaches were reported as mild and short-lived.
Researchers in this study suggested the cause of these headaches to be a buildup of nitric oxide.

Key Takeaways: Can Magic Mushrooms Treat Cluster Headaches?
Magic mushrooms and LSD are quickly becoming the go-to treatment for cluster headache sufferers. While this treatment is far from being approved, and there aren’t any clinical trials on this application yet — anecdotal reports and survey studies are promising.
Magic mushrooms have an impressive safety profile and are non-addictive. Based on some of the preliminary research and case studies suggesting them to be as effective, if not more effective, than conventional treatments without increasing risk makes them a promising candidate for future research.
The ability for shrooms to treat cluster headaches also opens a doorway for researchers attempting to study the condition — for which the cause remains completely elusive.
References
- May, A. (2005). Cluster headache: pathogenesis, diagnosis, and management. The Lancet, 366(9488), 843-855.
- Schindler, E. A., Gottschalk, C. H., Weil, M. J., Shapiro, R. E., Wright, D. A., & Sewell, R. A. (2015). Indoleamine hallucinogens in cluster headache: results of the Clusterbusters medication use survey. Journal of psychoactive drugs, 47(5), 372-381.
- Rozen, T. D., & Fishman, R. S. (2012). Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache: The Journal of Head and Face Pain, 52(1), 99-113.
- Sewell, R. A., Halpern, J. H., & Pope, H. G. (2006). Response of cluster headache to psilocybin and LSD. Neurology, 66(12), 1920-1922.
- Johnson, M. W., Sewell, R. A., & Griffiths, R. R. (2012). Psilocybin dose-dependently causes delayed, transient headaches in healthy volunteers. Drug and alcohol dependence, 123(1-3), 132-140.