Flubrotizolam (FANAX) Fact Sheet & Harm Reduction Guide
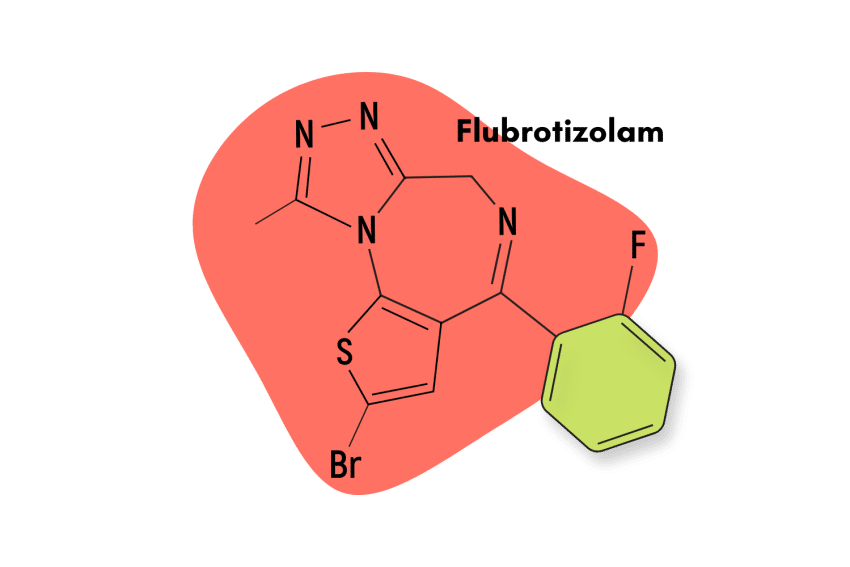
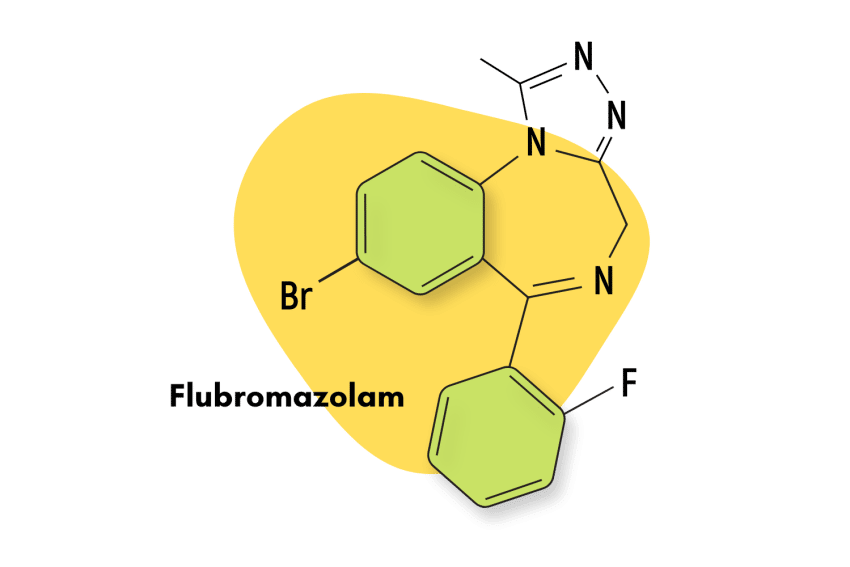
Flubrotizolam is a research chemical and novel benzodiazepine drug with effects similar to brotizolam (Lendormin) but many times more potent.
The high potency of this compound makes it a common adulterant in other grey-market benzodiazepine preparations. Less than 1 mg of this compound can produce powerful sedative and inebriating effects, especially if combined with other powerful benzodiazepine derivatives.
The safety of this compound has not yet been established, and there are no indications this drug will ever be studied and brought to market.
Flubrotizolam is relatively popular within the designer drug community.
Flubrotizolam Specs:
| Status: | Research Chemical |
| Common Dosage: | 0.5 mg |
| PubChem ID: | 3044878 |
| CAS# | 57801-95-3 |
IUPAC Name:
4-bromo-7-(2-fluorophenyl)-13-methyl-3-thia-1,8,11,12-tetrazatricyclo[8.3.0.02,6]trideca-2(6),4,7,10,12-pentaene
Metabolism:
Flubrotizolam is metabolized in the liver by an oxidative process carried out by the CYP450 enzyme family, particularly by CYP3A4 [4].
Duration of Effects:
The effects are expected to have a short duration of 5 to 8 hours. However, concrete data about the duration of active effects aren’t available.
What’s The Dose Of Flubrotizolam?
The exact dose of Flubrotizolam is unclear, but most grey market vendors carry this compound in doses of 0.5 mg each. This would make flubrotizolam roughly comparable in potency to drugs like alprazolam (Xanax) or triazolam (Halcion).
How Does Flubrotizolam Work?
Flubrotizolam acts as a central nervous system suppressant. It inhibits electrical activity in the brain, slowing down racing thoughts, reducing anxiety, and helping users fall asleep.
This same effect also inhibits other aspects of brain function, including memory formation, abstract thinking, and decision-making.
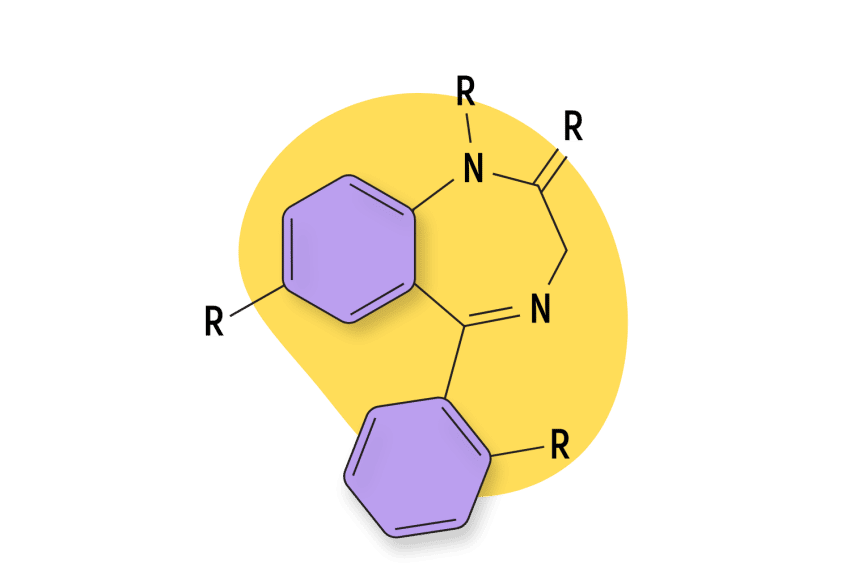
Most benzodiazepines, including flubrotizolam, work through the same mechanism. They potentiate a receptor called GABA-A, which the neurotransmitter, GABA, binds to in order to regulate electrical transmission in the brain.
When we’re stressed or anxious, GABA binds to these receptors to calm us down again. It’s often referred to as the “brake pedal for the brain” because of this effect.
When GABA activates the GABA receptors, chloride ion channels open up to hyperpolarize the neuron [6]. This causes the neurons to require a higher action potential in order to transmit electrical signals to neighboring nerve cells [7]. This effect also makes benzodiazepines useful for controlling seizure disorders.
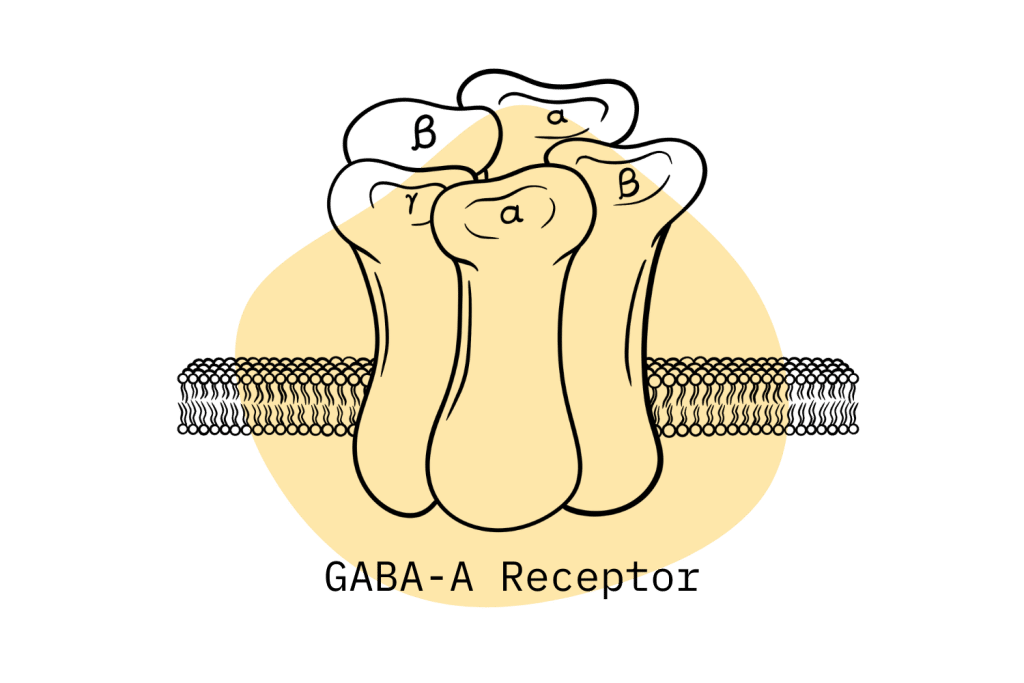
There are two subtypes of the GABA receptor — GABA-A and GABA-B. The GABA-A receptor is made up of a variety of subunits, specifically 2 alpha, 2 beta, and 1 gamma units which are further divided into subtypes [5]. Each benzodiazepine binds to these receptor subtypes a little bit differently — which is what results in a variable set of effects. Some benzos are more sedative; others are more intoxicating. The details of flubrotizolam’s binding affinities are not yet well understood.
Is Flubrotizolam Safe? Risks & Side-Effects
As reported by recreational users, the most common side effects of flubrotizolam include sleepiness, dizziness, and headaches. Memory loss, dependency, and rebound anxiety are common in people who take the drug frequently.
All benzodiazepines carry an inherent level of risk. The main concern is the potential for dependency and addiction and overdoses when used in combination with other sedative drugs (including recreational drugs like alcohol, opiates, and GHB).
Flubrotizolam also carries additional risks due to its status as a research chemical (insufficient safety testing and availability from unscrupulous vendors) and its high potency.
Side Effects Of Flubrotizolam
There is no official side effects list for this unapproved drug; however, experts suggest the side effects of this drug follow the same patterns as benzodiazepines in general.
Common side effects of benzodiazepines may include the following:
- An increase in salivation
- Cognitive impariment & inebriation
- Disinhibition
- Feeling sleepy or weak
- Headaches
- Low libido
- Memory loss
- Motor coordination problems
- Muscle weakness
- Poor sleep quality
- Sadness or depression
Serious side effects of flubrotizolam may include the following:
- Anaphylaxis & allergic reaction
- Bleeding from gums or nose
- Confusion & irritability
- Delusions or hallucinations
- Jaundice & liver damage
- Respiratory depression
- Suicidal ideation
- Tachycardia or heart arrhythmias
Harm Reduction: Flubrotizolam
Flubrotizolam, like many other medicines in its family, has the danger of addiction and the possibility of withdrawal symptoms.
Follow these simple benzodiazepine harm-reduction tips to reduce your risk of serious consequences when taking drugs like flubrotizolam:
- 🥣 Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- ⏳ Take frequent breaks or plan for a short treatment span — Benzodiazepines can form dependence quickly, so it’s important to stop using the drug periodically.
- 🥄 Always stick to the proper dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- 💊 Be aware of contraindications — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- 🧪 Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- 💉 Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- 🌧 Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- ⚖️ Understand the laws where you live — In most parts of the world, benzodiazepines are only considered legal if given a prescription by a medical doctor.
- 📞 Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Look up “addiction hotline” for more information where you live. (USA: 1-800-662-4357; Canada: 1-866-585-0445; UK: 0300-999-1212).
Flubrotizolam Drug Interactions
Using this medication with any other sedative medications, especially other benzodiazepines, alcohol, antihistamines, opiates, GHB, phenibut, or barbiturates, is highly dangerous. These drugs compound off each other to produce significant cognitive inhibition. This can lead to respiratory depression, coma, and death.
On their own, benzodiazepines carry a relatively low level of risk for overdose-related injury and death — however, when combined with other drugs, this risk increases substantially.
Flubrotizolam Contraindications
Unless you have a prescription, it’s advised to should stay away from this medication. Keep in mind that using this medication while you have certain health issues will make them worse.
It’s wise to avoid flubrotizolam if you’re pregnant, nursing, or trying to conceive.
It’s also wise to avoid this medication if you have pre-existing kidney problems, liver disease, or are above the age of 65.
Consult your doctor before taking any benzodiazepine medication (legal or otherwise).

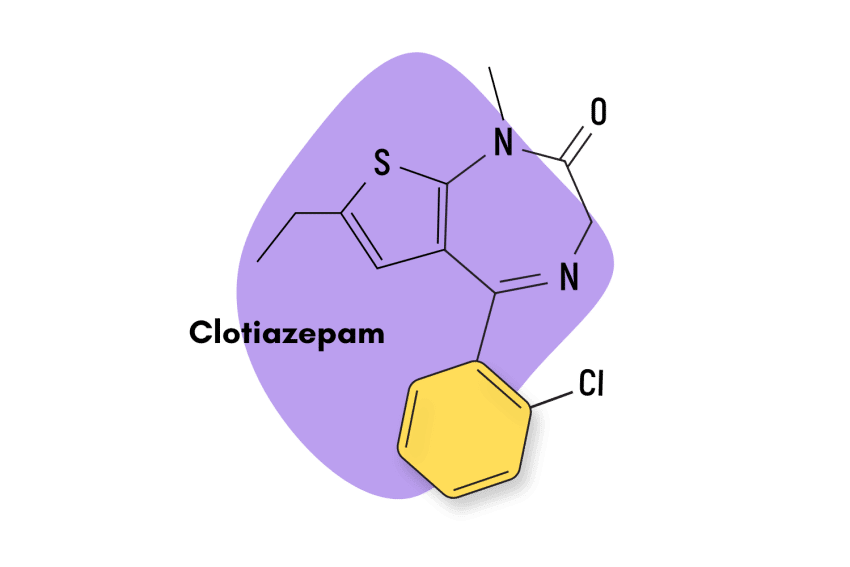
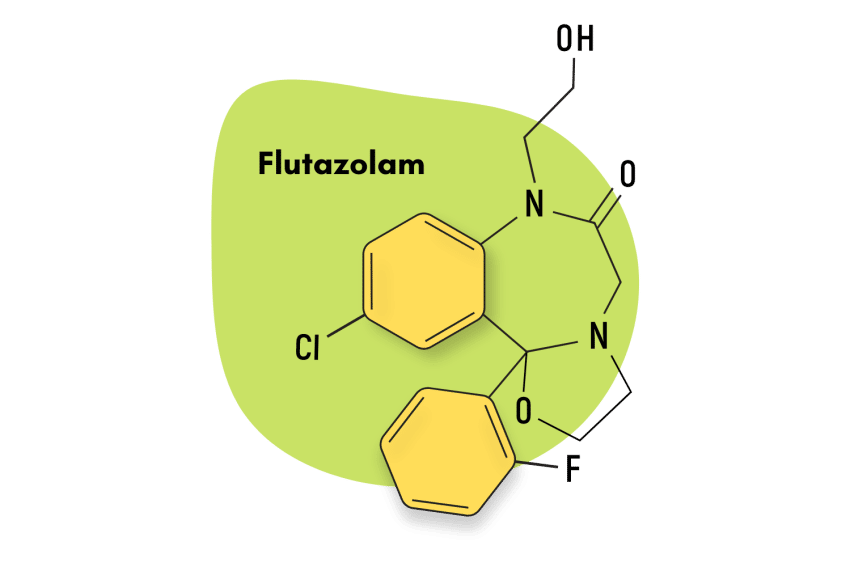
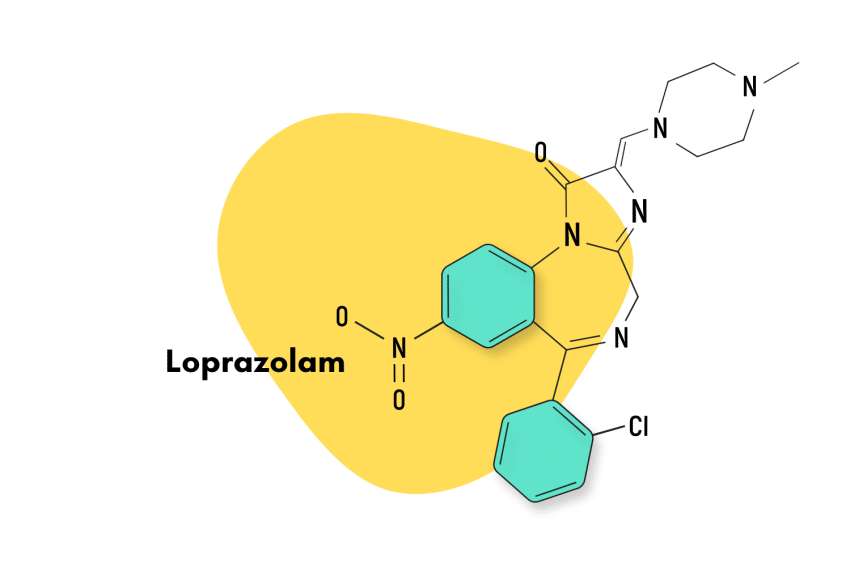
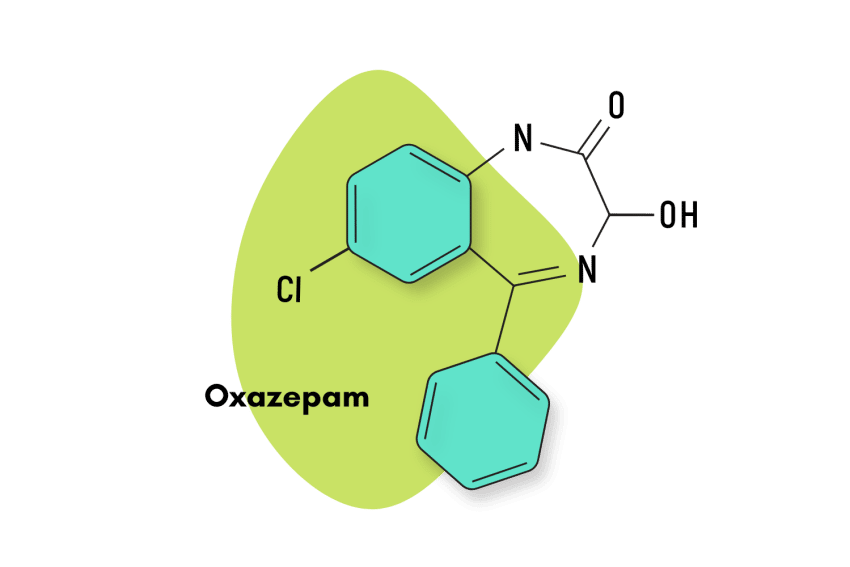
Similar Benzodiazepines
Flubrotizolam is a short-acting 1,4-benzodiazepine with a half-life of about 5 hours.
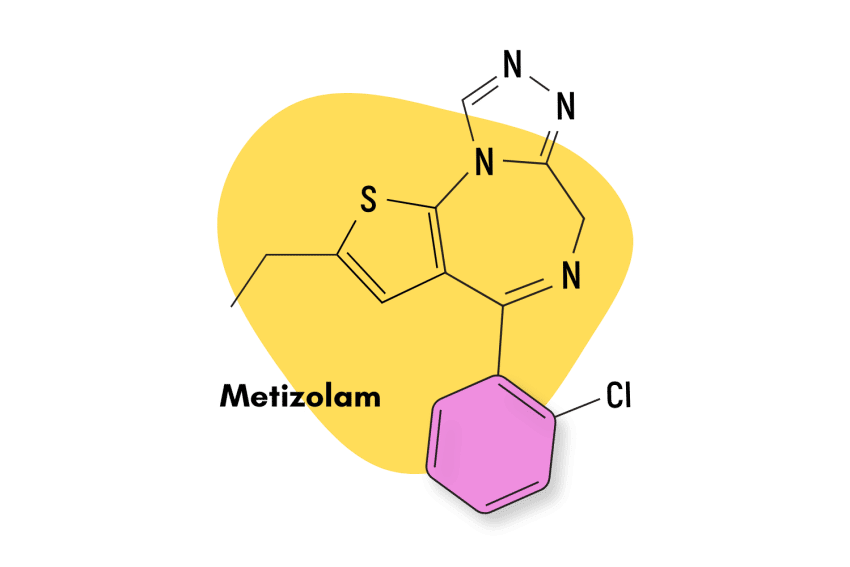
Other benzodiazepines having similar properties as those of flubrotizolam include metizolam, fluclotizolam, and etizolam.
The most common benzodiazepines include alprazolam (Xanax), clonazepam (Klonopin), chlordiazepoxide (Librium), lorazepam (Ativan), and diazepam (Valium).
Flubrotizolam vs. Other Short To Intermediate-Acting Benzodiazepines:
| Flubrotizolam | Metizolam | Fluclotizolam | Etizolam | |
| Chemical composition: | 1,4-benzodiazepine | 1,4-benzodiazepine | 1,4-benzodiazepine | 1,4-benzodiazepine |
| Route of administration: | Oral | Oral | Oral | Oral |
| Onset of action: | 10 to 30 minutes | 30 to 90 minutes | 10 to 30 minutes | 10 to 40 minutes |
| Peak concentration: | 1 to 3 hours | 30 minutes to 2 hours | Unknown | 3 to 4 hours |
| Duration of effects: | Short-acting (5 to 8 hours) | Short-acting (5 to 8 hours) | Short-acting (6 to 14 hours) | Short-acting (5 to 8 hours) |
| Mechanism of action: | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist |
| Medical Uses: | Anxiety disorder, hypnosis, insomnia, sedative, muscle relaxation | Muscle relaxation, sedation | Sedation, hypnosis | Anxiety disorder, insomnia, treatment of withdrawal symptoms |
Natural Alternatives to Benzodiazepines
Some natural supplements to flubrotizolam are listed below. These compounds have been reported to have some effects like those of benzodiazepines; however, there is a paucity of clinical evidence to support their effectiveness.
No herb or supplement is going to offer comparable strength to synthetic benzodiazepines like flubrotizolam — however, many of these substances offer benefits through the same mechanisms of action. They may serve as a viable alternative to try first or to gradually help wean off benzodiazepine use.
1. St. John’s Wort
St. John’s Wort, or Hypericum perforatum, is a flowering plant with star-shaped yellow flowers native to Europe. This small, unassuming plant is considered one of the premier herbs for managing chronic depression. It contains a host of active ingredients, many of which work as serotonin reuptake inhibitors (SSRIs) — which is the same mechanism of action used by many popular pharmaceutical antidepressants.
A recent study found that St. john’s wort, in combination with Valerian (Valeriana officinalis), was effective for treating mild to moderate depression with anxiety [8] — making it an alternative worthy of consideration.
2. Kava
The kava plant (Piper methysticum) is a medicinal rhizome found on various islands of the South Pacific. In places like Vanuatu and Fiji, the kava plant is considered a powerful relaxant, anxiolytic, and social lubricant.
The active ingredients in kava (called the kavalactones) work through similar mechanisms as benzodiazepines. They attenuate and modify the GABA-A receptors to enhance the natural calming action of GABA.
In a double-blind, placebo-controlled study, patients who were treated with a special extract of kava showed improvement in non-psychotic anxiety [9].
3. Valerian Root
Valerian (Valeriana officinalis) is often referred to as the closest plant-based alternative to benzodiazepines. It has a long history of use as a treatment for both anxiety and insomnia [10].
Many of the active ingredients of valerian have been found to exert their effects through the GABA-A receptors as well as various 5-HT serotonin receptors.
4. Ashwagandha
Ashwagandha, or Withania somnifera, is a traditional herb used in Ayurvedic medicine for the treatment of anxiety, insomnia, and chronic stress [11]. It’s revered as a premier adrenal tonic in traditional medical systems throughout Southeast Asia.
5. Chamomile
Chamomile or Matricaria chamomilla has a long history of use in Europe as a treatment for anxiety-related disorders. Its active ingredients, chamazulene, and several germacranolides act as GABAergic anxiolytics very similar to benzodiazepines.
Chamomile has also shown good efficacy in patients with generalized anxiety disorder (GAD) [11].
Flubrotizolam FAQs
Can I be prescribed flubrotizolam?
No, your doctor cannot prescribe flubrotizolam to you as it has not yet been approved for medical use.
How long will it take for flubrotizolam to be legally available?
It may take a few years for flubrotizolam to be legally available. This is because before being made available to the general public, all pharmaceuticals must undergo significant testing and several clinical trials.
Will I become addicted after taking flubrotizolam?
Like the majority of benzodiazepines, flubrotizolam has the possibility of addiction.
Can I buy flubrotizolam from online vendors?
It is best to avoid purchasing flubrotizolam from online vendors because flubrotizolam is not yet approved for medical use. Purchasing it through unverified sources increases the risk of serious adverse effects.
References
- Catabay, A., Taniguchi, M., Jinno, K., Pesek, J. J., & Williamsen, E. (1998). Separation of 1, 4-benzodiazepines and analogs using cholesteryl-10-undecenoate bonded phase in microcolumn liquid chromatography. Journal of chromatographic science, 36(3), 111-118.
- Langley, M. S., & Clissold, S. P. (1988). Brotizolam. Drugs, 35(2), 104-122.
- Ueki, S., Watanabe, S., Yamamoto, T., Shibata, S., & Shibata, K. (1984). Behavioral effects of brotizolam, a new thienotriazolodiazepine derivative. The Japanese Journal of Pharmacology, 35(3), 287-299.
- Orsolini, L., Corkery, J. M., Chiappini, S., Guirguis, A., Vento, A., De Berardis, D., … & Schifano, F. (2020). ‘New/Designer Benzodiazepines’: an analysis of the literature and psychonauts’ trip reports. Current neuropharmacology, 18(9), 809-837.
- Whiting, P. J. (2006). GABA-A receptors: a viable target for novel anxiolytics? Current opinion in pharmacology, 6(1), 24-29.
- Mehta, A. K., & Ticku, M. K. (1999). An update on GABAA receptors. Brain research reviews, 29(2-3), 196-217.
- Goetz, T., Arslan, A., Wisden, W., & Wulff, P. (2007). GABAA receptors: structure and function in the basal ganglia. Progress in brain research, 160, 21-41.
- Sarris, J., Kavanagh, D. J., Deed, G., & Bone, K. M. (2009). St. John’s wort and kava in treating major depressive disorder with comorbid anxiety: A randomised, double‐blind placebo‐controlled pilot trial. Human Psychopharmacology: Clinical and Experimental, 24(1), 41-48.
- Geier, F. P., & Konstantinowicz, T. (2004). Kava treatment in patients with anxiety. Phytotherapy Research: An International Journal Devoted to Pharmacological and Toxicological Evaluation of Natural Product Derivatives, 18(4), 297-300.
- Kinrys, G., Coleman, E., & Rothstein, E. (2009). Natural remedies for anxiety disorders: potential use and clinical applications. Depression and anxiety, 26(3), 259-265.
- Sarris, J., McIntyre, E., & Camfield, D. A. (2013). Plant-based medicines for anxiety disorders, part 2: a review of clinical studies with supporting preclinical evidence. CNS drugs, 27(4), 301-319.