Bretazenil: A Jumping-Off Point For New Social Psychoactive Drugs?
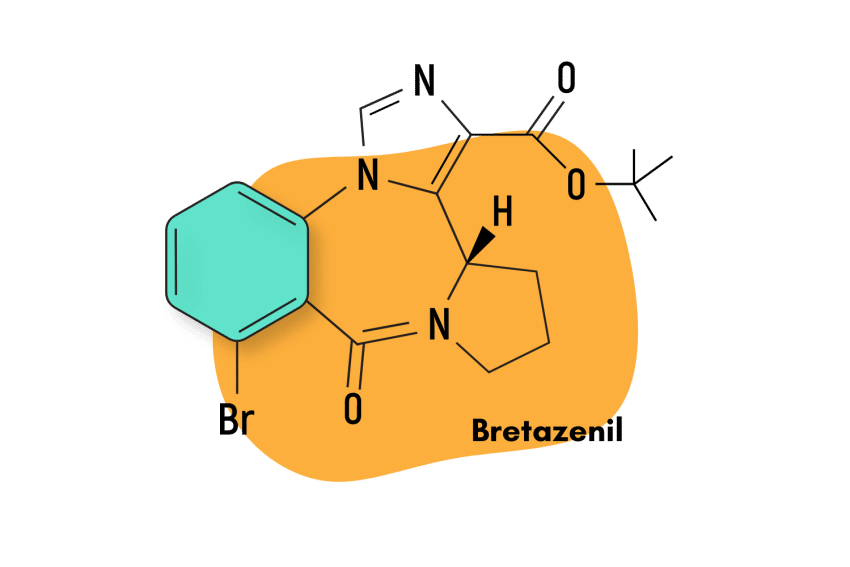
Bretazenil was invented in 1988 but never made it through clinical testing. It exists today as a designer benzodiazepine drug (DBZD) popular for its euphoric and inebriating qualities.
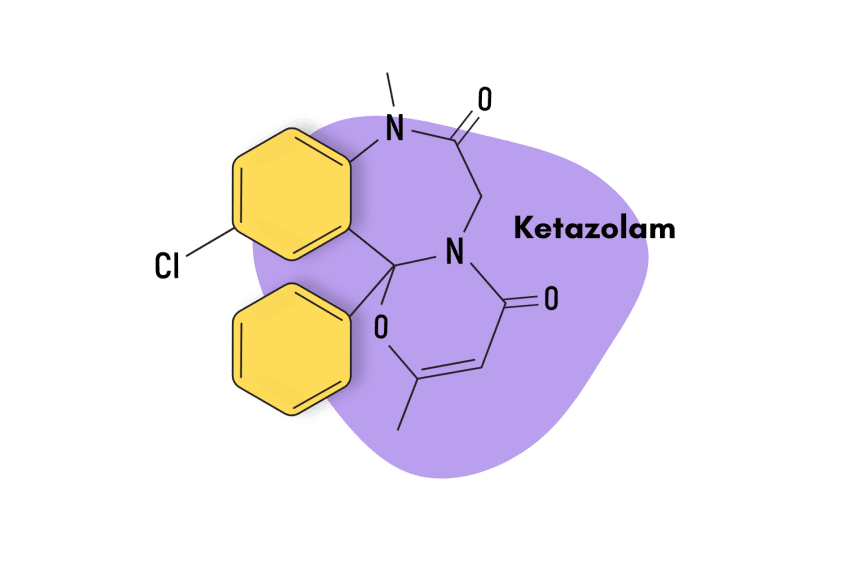
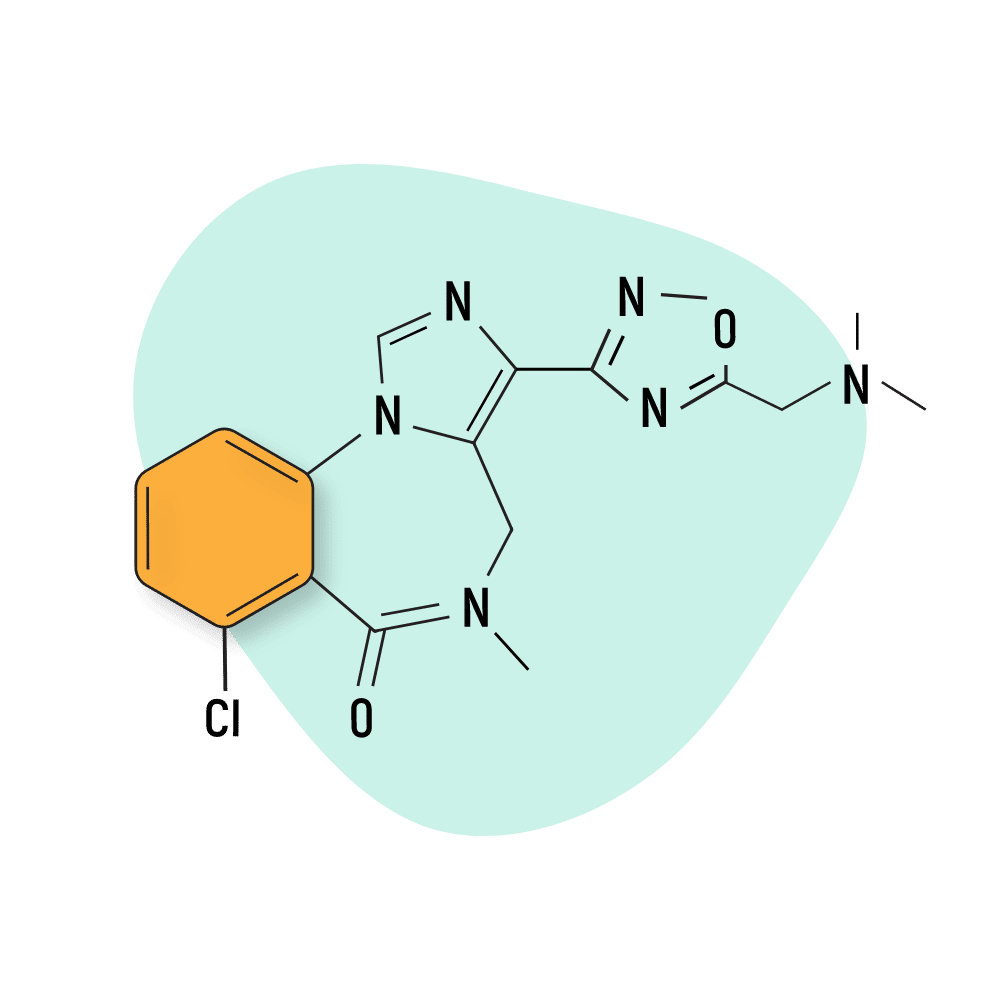
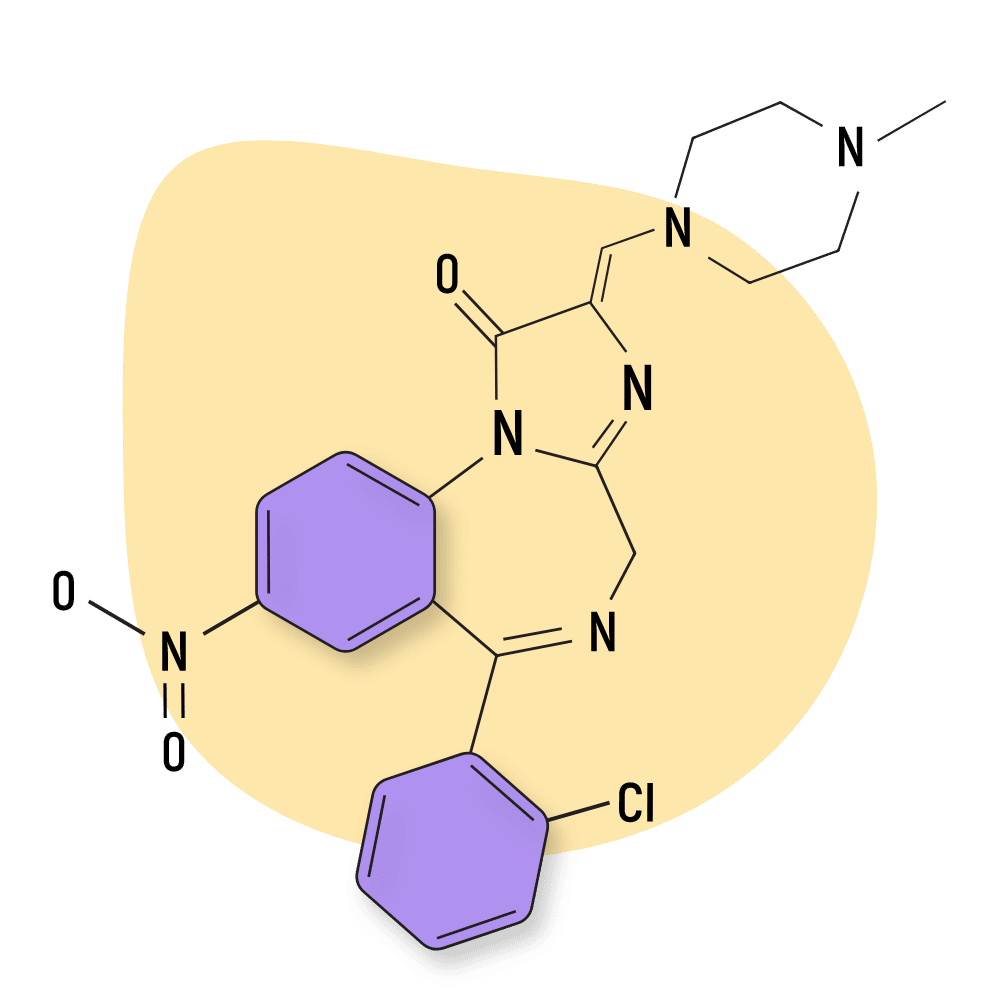
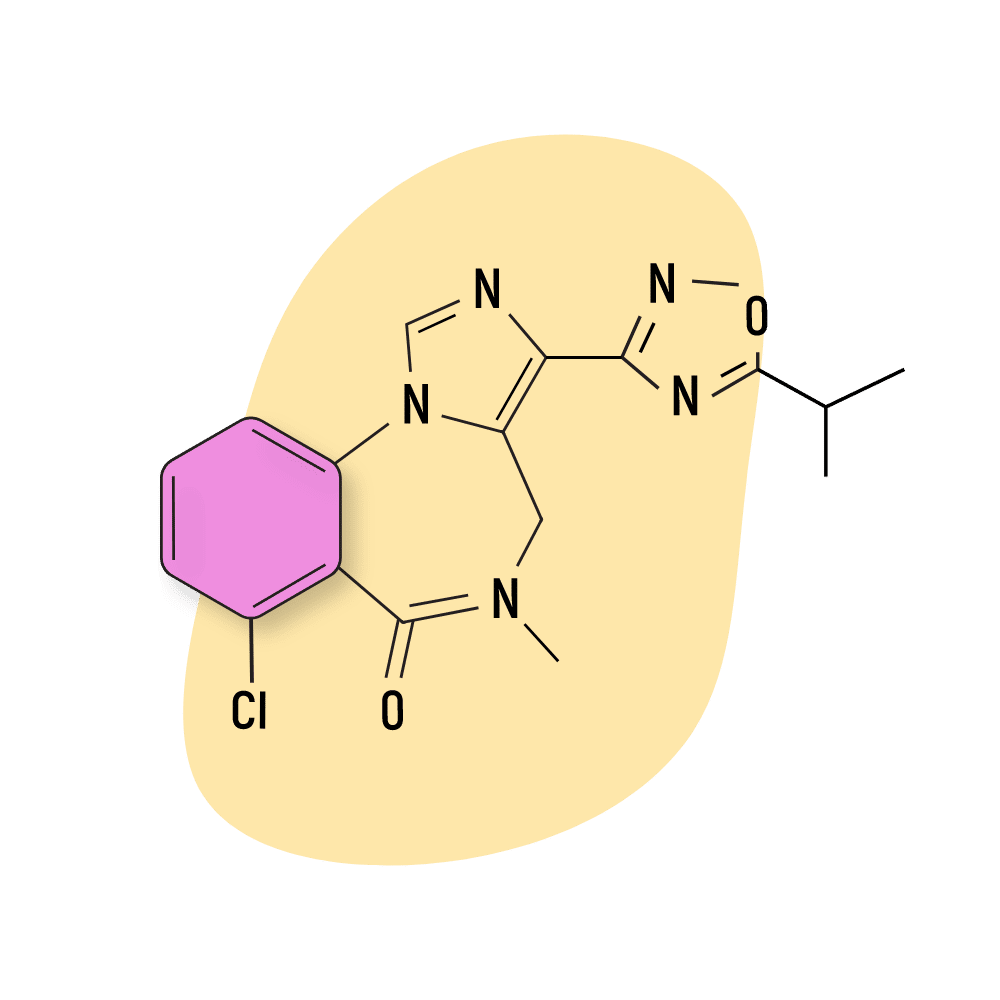
This compound is classified as an imidazopyrrolobenzodiazepine — which is a subclass of the larger benzodiazepine family. Structurally, bretazenil is most similar to the benzodiazepine antidote — flumazenil — but the effects share more overlap with other members, including alprazolam and clonazepam.
Psychedelic drug researcher, David Nutt, once suggested this high-potency benzodiazepine could serve as an excellent jumping-off point for developing other social drugs.
Bretazenil differs from traditional 1,4-benzodiazepines by exerting its effects through a different mechanism of action. Data suggests this gives bretazenil a more benign adverse effects profile and less of a potential to cause physical dependence and withdrawal symptoms (unconfirmed).
At the moment, bretazenil has not been clinically approved for use in the United States.
Bretazenil Specs
| Status | Research Chemical 🧪 |
| Common Dosage | Unspecified |
| PubChem ID | 107926 |
| CAS# | 84379-13-5 |
IUPAC Name: Tert-butyl(7S)-14-bromo-12oxo-2,4,11-triazatetracycloheptadeca-1(17),3,5,13,15-pentaene-5-carboxylate
Other Names: None.
Metabolism: Research on the pharmacokinetics of bretazenil is insufficient.
Duration of Effects: Short-acting (Unspecified duration). Research on this is unclear, but the elimination half-life is only 2.5 hours, suggesting its duration of effects is relatively fast compared to other benzodiazepines.
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Bretazenil Work?
Traditional benzodiazepines exert their effects through their interactions with GABA neurotransmitters, specifically GABA-A. They bind to GABA-A and produce an allosteric effect which potentiates the inhibitory effects of GABA-A on the neurons located in the brain and central nervous system (CNS). This, in turn, decreases the ability of neurons to fire and thus slows down overall brain activity. The slowdown is responsible for the typical benzodiazepine effects: reduction of anxiety and depression-related symptoms, as well as hypnotic and muscle relaxant properties.
During this process, traditional benzodiazepines bind to certain subunits within the GABA-A receptors and act as full agonists. Bretazenil has a different mechanism of action because it binds to a broader set of GABA-A subunits and acts as a partial agonist. Specifically, bretazenil binds to the α1, α2, α3, α4, α5, and α6 subunits, while 1,4- benzodiazepines only bind to α1, α2, α3, and α5 [1].
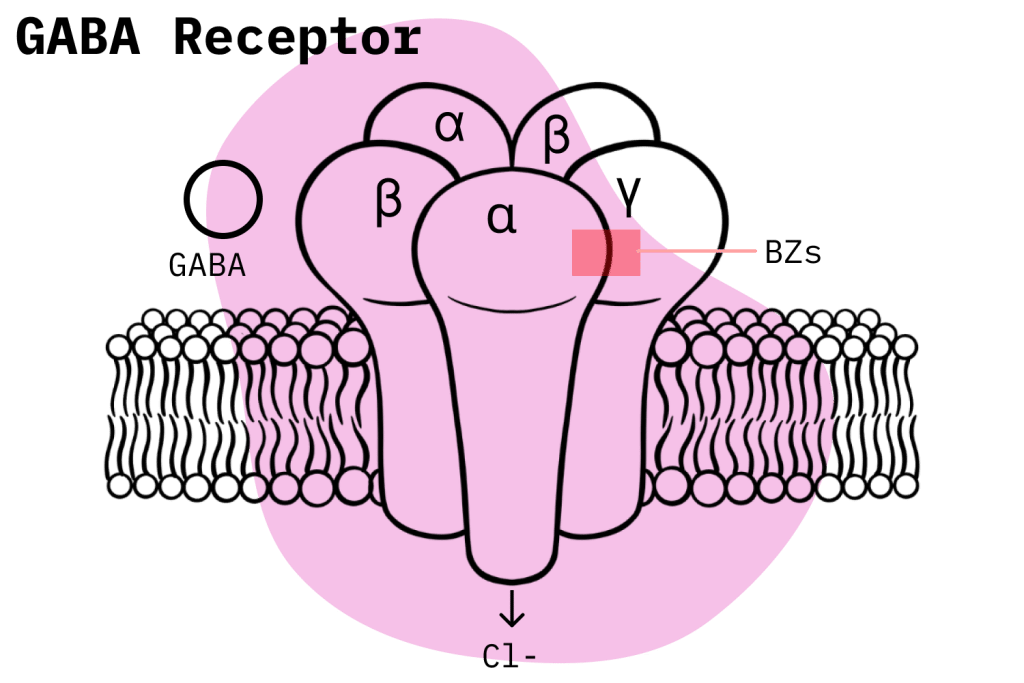
These differences are significant because, even though there is a lot about this process that isn’t yet understood, it has been shown that the variations benzodiazepines display when binding to the distinct GABA-A subunits account for the variety of effects that benzodiazepines can produce [2].
Additionally, being a partial agonist rather than a full agonist, when bretazenil binds to a GABA-A receptor, it only has partial efficacy relative to a full agonist. Certain studies contend that this decreased efficacy in relation to full agonists leads to bretazenil having a less severe adverse effects profile and a decreased potential to cause physical dependence [3].
Is Bretazenil Safe? Risks & Side Effects
Bretazenil has not been approved for commercial use, and limited clinical data makes it difficult to determine the risk level posed by it. However, we do have enough information to sketch out a rough idea. In general terms, the safety of bretazenil shouldn’t really be a concern for most people since it is not commercially available, and thus, procuring it is somewhat of an impossibility.
Bretazenil’s clinical development was discontinued not because it was considered unsafe for use but rather because there was little separation between its anxiolytic and sedative effects, making the drug clinically ineffective [4]. This wide spectrum of effects does make sense because, as explained before, bretazenil targets a broader range of GABA-A receptor subtypes.
However, there was positive evidence for bretazenil having a less dangerous side effects profile than traditional benzodiazepines, like diazepam, and less potential to cause physical dependence and withdrawal. It was also found that bretazenil was effective in treating generalized anxiety disorder (GAD) as well as panic disorder and had much better tolerability than 1,4- benzodiazepines [4].
Harm Reduction: Bretazenil
Harm reduction is an important concept to be aware of when dealing with benzodiazepines, even ones with less potential to cause adverse effects like bretazenil.
Here are some simple harm-reduction tips for benzodiazepine drugs:
- Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- Take frequent breaks — Benzodiazepines can form dependence quickly, so it’s important to stop using the drug periodically.
- Know the dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg, others can be fatal in doses as low as 3 mg.
- Know who should NOT use benzos for any reason — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Lookup “addiction hotline” for more information where you live. (USA: 1-800-662-4357; Canada: 1-866-585-0445; UK: 0300-999-1212).
General Recommendations
With prescription drugs like benzodiazepines, users must always take pains to follow their prescriptions closely. Taking more than the recommended dose or using your prescription for a different reason than the one it was given to you is still misuse, and it will put you at more risk of developing an unhealthy habit with benzodiazepines.
Due to the significant risk factors involved with benzodiazepines, the general rule of thumb with doctors is to try and prescribe them for the shortest time frame possible; even then, there is a chance that physical dependence will develop. One study concluded that nearly one-third of individuals who take benzodiazepines for longer than four weeks become dependent and experience withdrawal symptoms upon cessation [5].
If one is considering a benzodiazepine prescription, it is essential to conduct proper research beforehand and be cognizant of the risks it can entail. It is no secret that doctors sometimes operate under dubious incentives which reward them for handing out prescriptions with minimal consideration. As a minimum, users should investigate non-pharmacological alternatives for their ailment — like exercise, therapy, or plant-based medications — and give those a try.
Bretazenil Drug Interactions
Opioids and alcohol should never be consumed if one is currently on a benzodiazepine prescription. When combined, these drugs dramatically raise the incidence of potentially fatal events, like respiratory depression, the leading cause of overdose deaths.
Depending on what CYP enzymes they are metabolized by, prescription medications are normally also affected by compounds that either induce or inhibit the functioning of said enzymes. This can lead to the benzodiazepines losing effectiveness, or it can make it so that the compound stays inside the body longer, raising the probability of adverse effects. Users should always be aware of possible CYP interactions when taking prescription benzodiazepines.
Bretazenil Contraindications
Contraindications are a common way users unknowingly put themselves at risk. When taking benzodiazepines, always check the contraindications. Common ones include people with hepatic impairments, pregnant women, minors, driving or operating heavy machinery, etc.
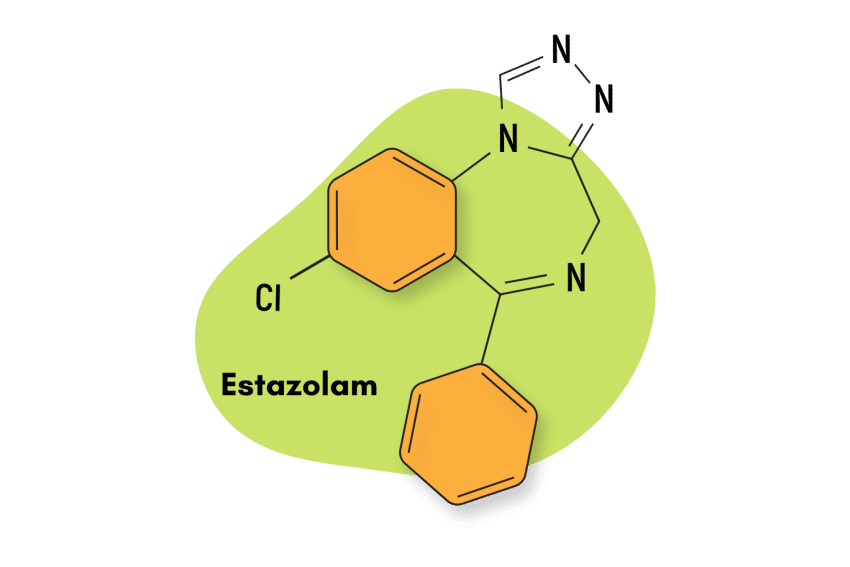
Similar Benzodiazepines
Imidazobenzodiazepines like bretazenil have certain characteristics that set them apart. For instance, this subtype contains a series of compounds that act as both agonists and inverse agonists to the GABA-A receptors, and many of them are also considered to be partial, rather than full benzodiazepine receptor agonists [6].
EVT-201
Like bretazenil, EVT-201 is an imidazobenzodiazepine that exerts its mechanism of action through the standard GABA-A pathway. EVT-201 is also not approved as a medication but it is currently undergoing trials to serve treat sleep-related conditions.
Loprazolam
Loprazolam belongs in the same subtype as bretazenil and shares some of its pharmacological properties like a reduced incidence of adverse effects. However, loprazolam is intermediate-acting while bretazenil is short-acting.
FG-8205
There is not a lot of information available on FG-8205 but we do know that it shares a similar structure as bretazenil. It also exhibits a similar pharmacological profile with similar potency but less tendency towards sedation.
Alternatives to Benzodiazepines
When considering non-pharmacological alternatives to benzodiazepines, the best option is to go with a plant-based remedy.
The kava plant stands out as an obvious choice. It is an all-natural species of plant hailing from the pacific islands and has been shown to produce anxiolytic effects while having a relatively benign side effects profile [7].
Another great alternative is Mitragyna speciosa, otherwise known as the kratom plant. Kratom has a broader range of effects than kava as it can also produce stimulant-like benefits in addition to its anxiolytic and sedative effects [8], but there are some drawbacks. Kratom targets opioid receptors and can thus be dangerous if used concomitantly with other CNS depressants like drugs or alcohol. Additionally, mid-to-high doses of kratom are required for it to achieve its anxiolytic effects.
Bretazenil FAQs
1. What was the original purpose of bretazenil?
Bretazenil was originally developed for use as an anti-anxiety drug and has also been studied for use as an anticonvulsant.
2. Is bretazenil still under clinical development?
No. Bretazenil, as well as other partial agonists like pazinaclone and abecarnil, were discontinued for a number of reasons, like its exceedingly broad and inseparable range of effects. However, research does continue for other partial agonist benzodiazepines.
References
- Pym, L. J., Cook, S. M., Rosahl, T., McKernan, R. M., & Atack, J. R. (2005). Selective labelling of diazepam‐insensitive GABAA receptors in vivo using [3H] Ro 154513. British journal of pharmacology, 146(6), 817-825.
- Sieghart, W., & Sperk, G. (2002). Subunit composition, distribution and function of GABA-A receptor subtypes. Current topics in medicinal chemistry, 2(8), 795-816.
- Haefely, W., Facklam, M., Schoch, P., Martin, J. R., Bonetti, E. P., Moreau, J. L., … & Richards, J. G. (1992). Partial agonists of benzodiazepine receptors for the treatment of epilepsy, sleep, and anxiety disorders. Advances in biochemical psychopharmacology, 47, 379-394.
- Ross, C. A., Margolis, R. L., Reading, S. A., Pletnikov, M., & Coyle, J. T. (2006). Neurobiology of schizophrenia. Neuron, 52(1), 139-153.
- Riss, J., Cloyd, J., Gates, J., & Collins, S. (2008). Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta neurologica scandinavica, 118(2), 69-86.
- Zhang, P., Zhang, W., Liu, R., Harris, B., Skolnick, P., & Cook, J. M. (1995). Synthesis of novel imidazobenzodiazepines as probes of the pharmacophore for” diazepam-insensitive” GABAA receptors. Journal of medicinal chemistry, 38(10), 1679-1688.
- Cairney, S., Clough, A. R., Maruff, P., Collie, A., Currie, B. J., & Currie, J. (2003). Saccade and cognitive function in chronic kava users. Neuropsychopharmacology, 28(2), 389-396.
- Swogger, M. T., & Walsh, Z. (2018). Kratom use and mental health: A systematic review. Drug and Alcohol Dependence, 183, 134-140.