Lorazepam (Ativan): Harm Reduction, Dosage, Effects
Why is lorazepam so popular, and what can be used instead?
Lorazepam (sold as Ativan, Tavor, Temesta, and others) is a prescription benzodiazepine drug indicated for the management of anxiety disorders or for the short-term relief of depression.
This drug is also used to treat several conditions in an off-label (non-FDA-approved) manner. It’s sometimes used as a tranquilizer, for managing alcohol withdrawal symptoms, treating insomnia, panic disorder, delirium, chemotherapy-induced nausea and vomiting, and psychogenic catatonia [1]. None of these uses have been approved by the FDA.
Lorazepam is also a popular recreational drug and drug of abuse. It’s taken alongside stimulants to dull the side effects or on its own as an inebriant with GHB-like effects.
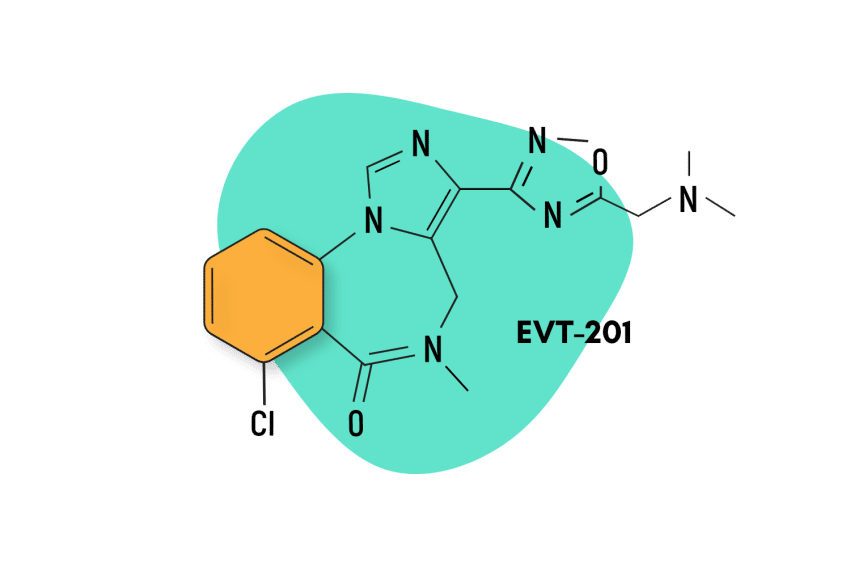
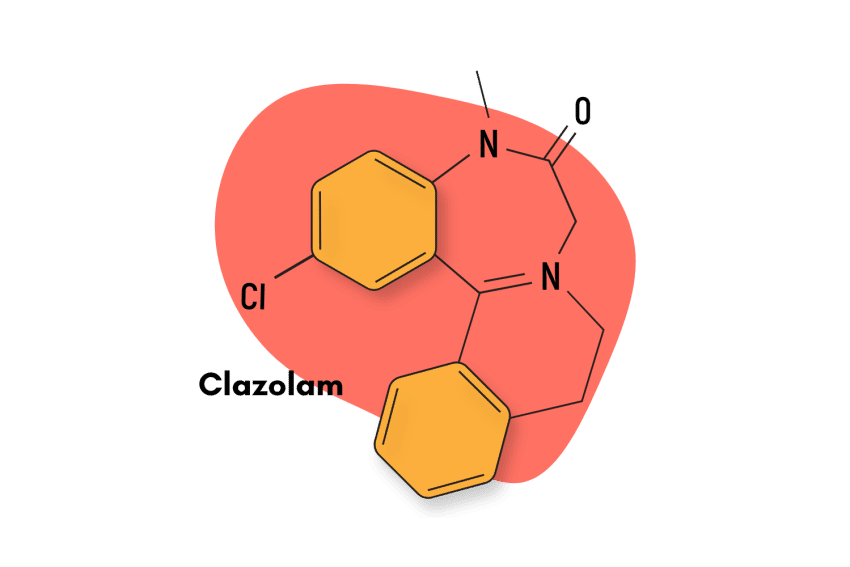
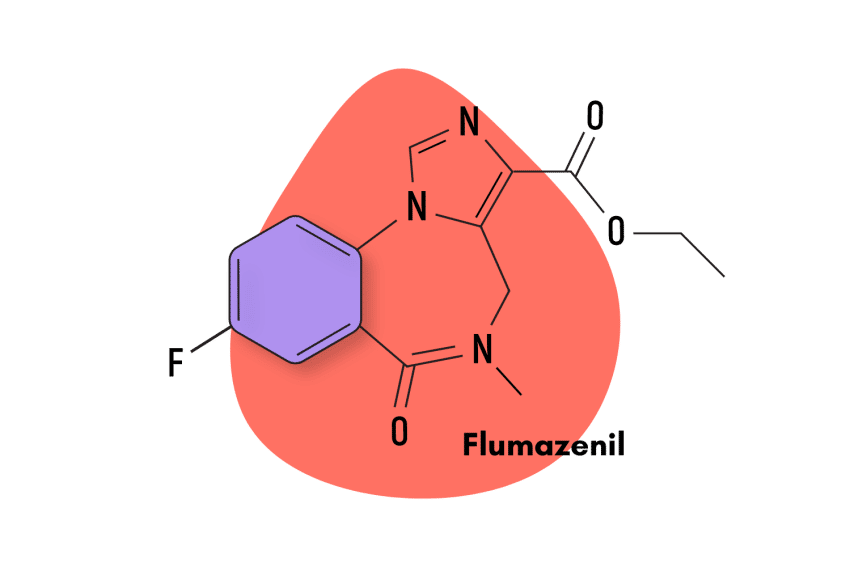
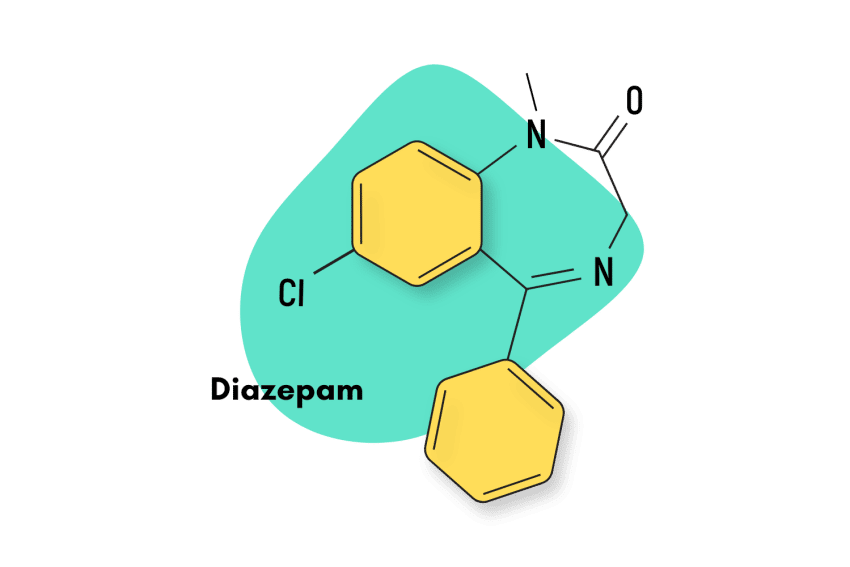
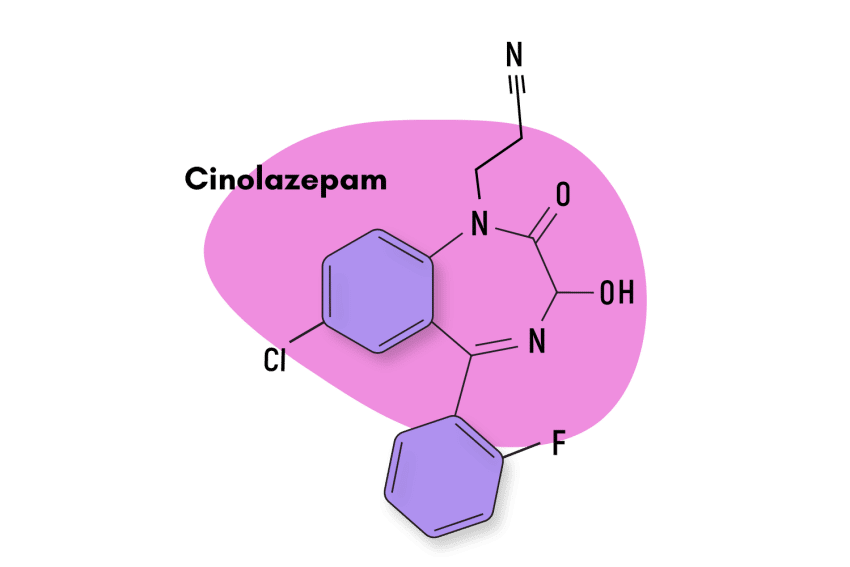
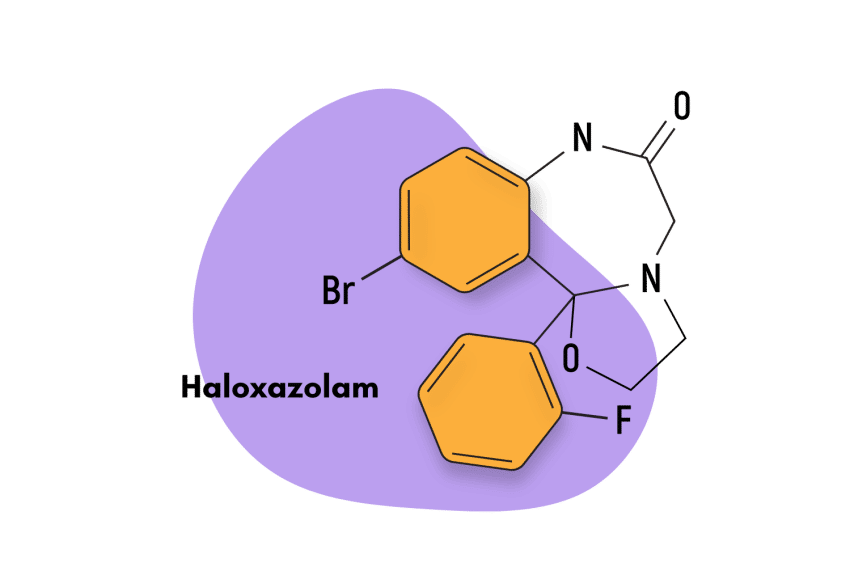
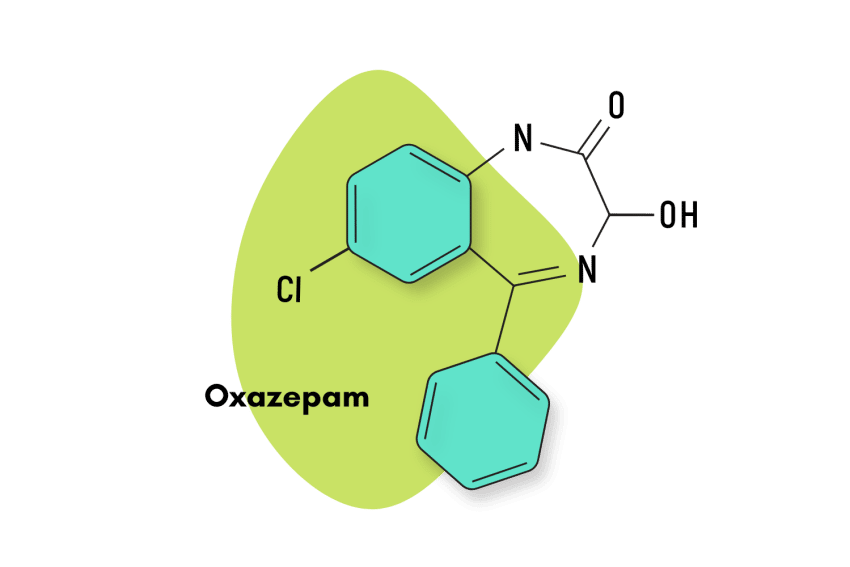
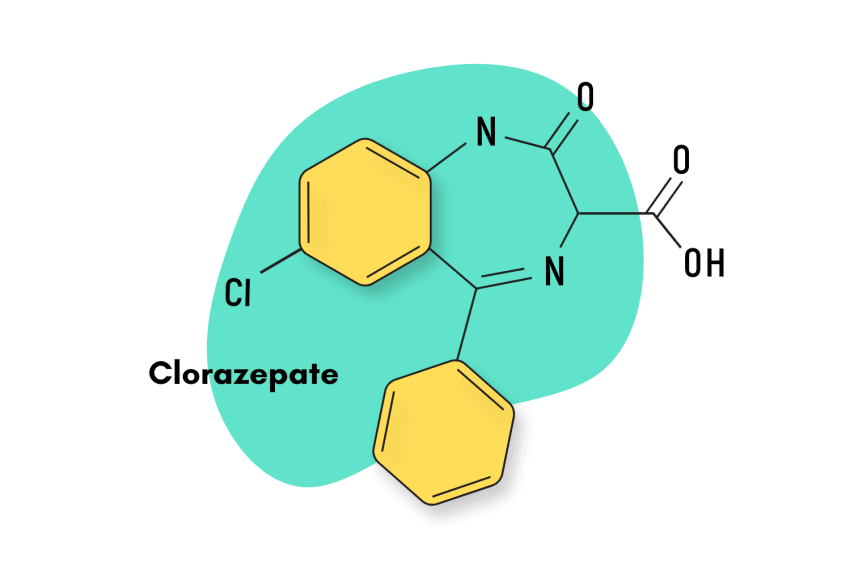
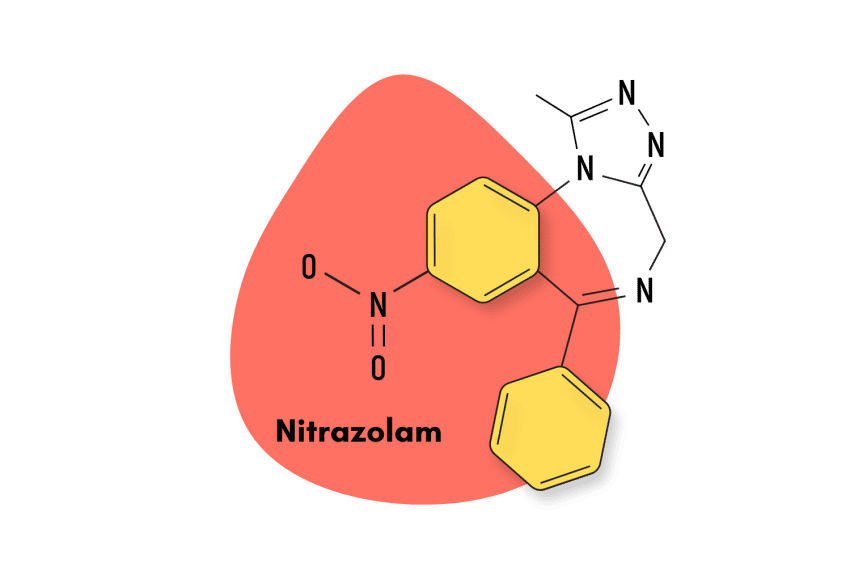
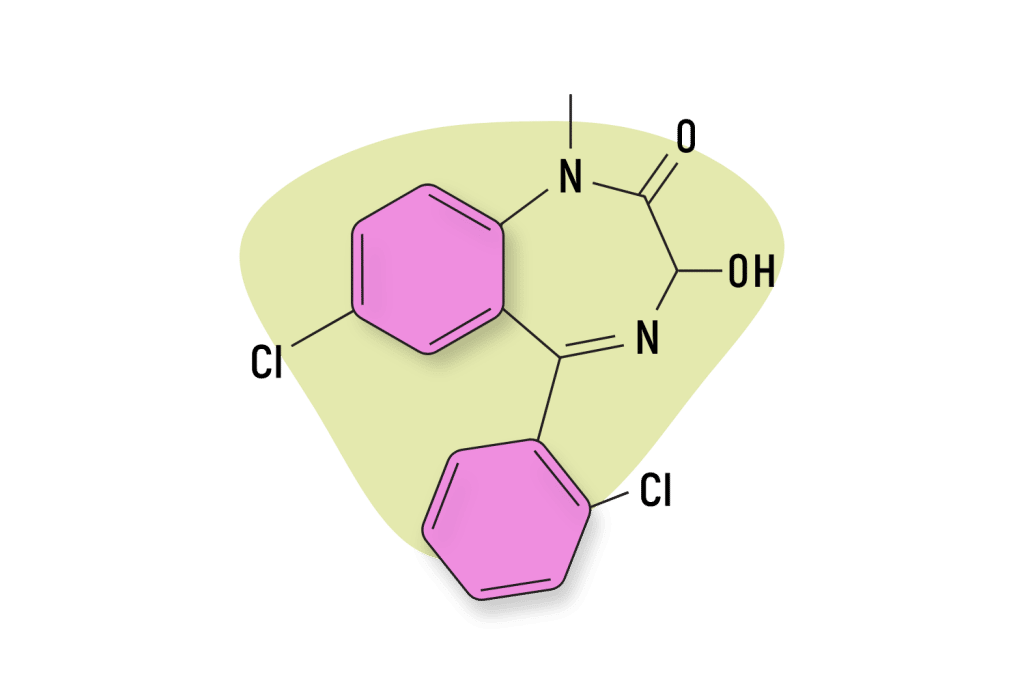
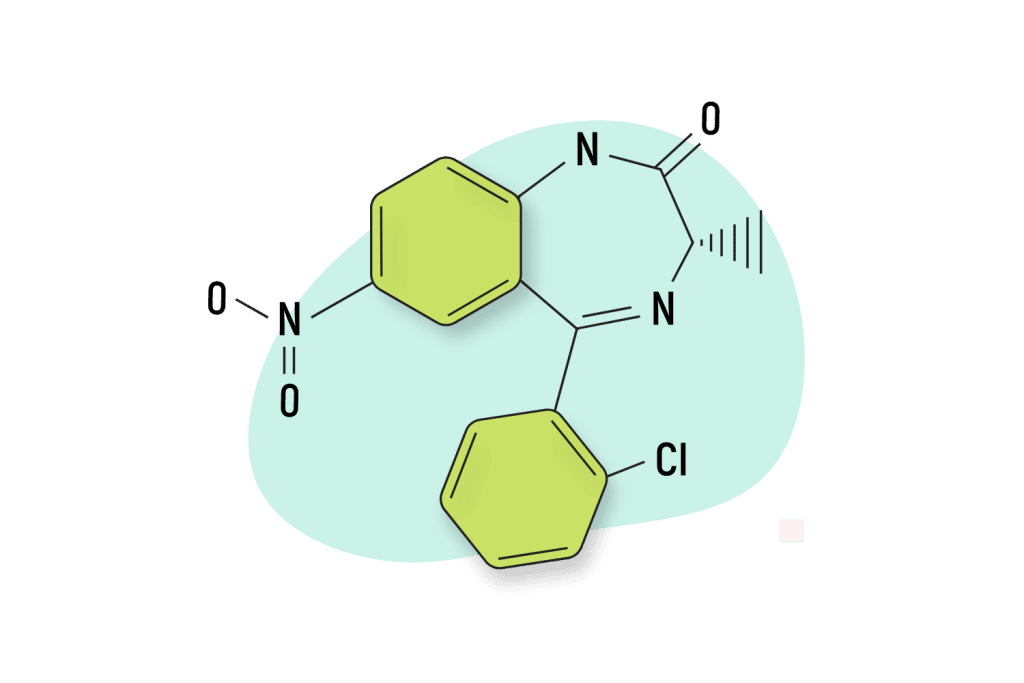
In terms of chemical structure lorazepam is a 1,4- benzodiazepine derivative similar to diazepam (Valium), clonazopam (Klonopin), or bromazepam (Lectopam). It specifically features a 3-hydroxy configuration similar to oxazepam and temazepam [2].
Lorazepam Specs
IUPAC Name: 7-chloro-5-(2-chlorophenyl)-3-hydroxy-1,3-dihydro-1,4-benzodiazepin-2-one
Other Names: Ativan, Orfidal, Lorenin, Lorsilan, Temesta, Tavor, & Lorabenz.
Metabolism: Lorazepam’s metabolism is not CYP mediated. It directly undergoes glucuronide conjugation.
Duration of Effects: Intermediate-Acting (10–20 hours). Lorazepam starts to work in 20 to 30 minutes and reaches peak concentration at around 1 to 1.5 hours. The half-life is 10-20 hours, mainly depending on age.
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Lorazepam Work?
The mechanism of action of lorazepam is comparable to that of most other benzodiazepines. Essentially, lorazepam binds to benzodiazepine receptors located on the postsynaptic GABA-A ligand-gated chloride channel and produces an allosteric effect that leads to the hyperpolarization of the neuron and, resulting in reduced brain and central nervous system activity (CNS) [3].
Let’s break this process down so it makes more sense. We have to start with the GABA receptors.
GABA is the primary neuro-inhibitory molecule in the brain. It acts as the brake pedal, slowing brain activity to prepare us for sleep and reverse stress states.
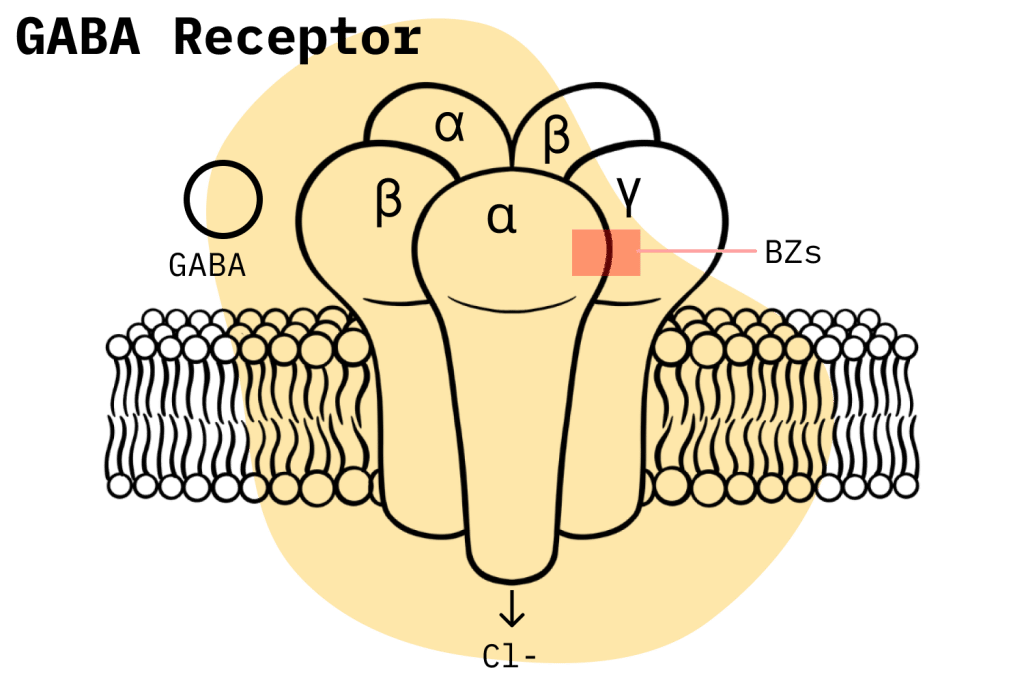
Benzodiazepines bind to these receptors, but rather than activating them directly, they work to increase the binding affinity for natural GABA. It would be like increasing the sensitivity of the brake pedal so even small presses of the feet bring the car to a stop.
The technical word for how benzodiazepines work is called “allosteric modulation.”
An allosteric effect is when a ligand (in this case, a benzodiazepine) binds to one site on a protein molecule (GABA-A), affecting the properties of another site of the same protein. In the case of benzodiazepines and GABA-A, the allosteric effect produced is an increased opening frequency of the chloride channel located on the GABA-A receptor, which, through a series of activities, leads to reduced levels of activity in the brain.
This generalized inhibitory effect gives rise to all the pharmacological properties associated with benzodiazepines.
Lorazepam Pharmacodynamics & Pharmacokinetics
Lorazepam’s pharmacological specificities are explained mainly by pharmacokinetic properties: poor water and lipid solubility, high protein binding, antioxidative metabolism to a pharmacologically inactive metabolite, and elevated relative potency.
For instance, its poor lipid solubility means the volume of distribution occurs mostly through the vascular compartment, which causes relatively long-lasting peaks. If we compare this to diazepam, a far-more lipid soluble benzodiazepine, we can see that although diazepam is more readily absorbed, it is soon redistributed to other areas in the body, particularly body fat. With these effects in mind, we can understand why one dose of lorazepam has more long-lasting peak effects despite a shorter elimination half-life than an equivalent dose of diazepam [4].
Is Lorazepam Safe? Risks & Side Effects
All benzodiazepines carry a certain level of risk. Under the Controlled Substance Act, they are Schedule IV compounds, which means they are approved but can potentially cause dependence and provoke misuse.
In general terms, benzodiazepines are relatively safe when taken in strict accordance with a prescription (i.e., when there’s no misuse). However, the risk level rises considerably when the potential for abuse is factored in.
In the United States, recent statistics have revealed the grave extent of benzodiazepine misuse and its consequences. For instance, a 2020 survey by the CDC found that, in that year, benzodiazepines were involved in 12,290 drug overdose deaths.
Another study from the National Institute on Drug Abuse revealed that benzodiazepines were also found in 16% of overdose deaths. The opioid crisis is certainly a bigger problem, but the media attention has masked the fact that benzodiazepine misuse is also becoming a serious problem in the United States.
It’s hard to draw meaningful conclusions about how lorazepam contributes to the overall situation concerning benzodiazepine misuse. However, based on its pharmacology and pharmacokinetics, we can compare the relative misuse potential of lorazepam with other benzodiazepines.
Based on what we know from clinical evidence, the pharmacokinetics of lorazepam make it relatively riskier when we compare it to other benzodiazepines. The high potency of lorazepam, its confinement to the blood, its relatively short half-life, and its pharmacologically inactive metabolites make it a prime candidate for abuse because these characteristics are more likely to provoke withdrawal symptoms, next-dose cravings, and the reinforcement of psychological dependence [5].
Side Effects of Lorazepam
Most adverse reactions to benzodiazepines are dose-dependent and tend to subside after the first initial doses.
In a sample size of about 3,500 patients, the FDA identified the following side effects:
- Agranulocytosis
- Allergic skin reactions
- Alopecia
- Amnesia
- Asthenia
- Ataxia
- Changes in libido
- Confusion
- Constipation
- Convulsions
- Depression
- Disinhibition
- Disorientation
- Dizziness
- Drowsiness
- Dysarthria
- Euphoria
- Fatigue
- Hyponatremia
- Hypothermia
- Impotence
- Increases in alkaline phosphatase
- Increases in bilirubin
- Increases in liver transaminases
- Jaundice
- Memory impairment
- Pancytopenia
- Sedation
- Suicidal ideation
- Thrombocytopenia
- Tremors
- Unsteadiness
- Vertigo
- Weakness
Benzodiazepine Withdrawal & Dependence: Lorazepam
The potential for benzodiazepines to cause physical dependence and withdrawal symptoms is a widely recognized phenomenon in the medical world. As such, doctors generally try to mitigate this risk by prescribing benzodiazepines for the shortest possible time, usually 2-4 weeks.
People considering a benzodiazepine prescription should be aware that even if they don’t engage in any misuse, the potential to develop a dependence is still significant. Studies have shown that the proportion of patients who develop an addiction after more than four weeks of using benzodiazepines is as high as 33% [5].
When a physical dependence develops, a patient must go through a long, drawn-out drug tapering procedure to get off benzodiazepines safely. Drug tapering is relatively safe when done under the guidance of a licensed physician, but complications can develop, and the process can take as long as 18-24 weeks.
If you’re currently on a benzodiazepine medication, it is not recommended that you abruptly stop taking them. If you want to stop using benzodiazepines, contact your doctor and let him/her know.
Harm Reduction: Lorazepam
In this article, we hope to help keep people safe by providing safe-to-use and practical recommendations for dealing with benzodiazepines.
The most important advice we could offer is to consider whether a benzodiazepine prescription is even worth it. It is no secret that doctors sometimes act under dubious incentives when prescribing drugs, and many people try to solve their ailments through pharmacological medications without even considering other safer options.
Before jumping for a benzodiazepine prescription, we highly recommend users attempt behavior-related solutions to their ailments or go for a herbal, plant-based substitute.
Also, one of the most critical questions users have to ask themselves is this: how likely is it that they won’t engage in any misuse? This is a key question because misuse, especially recreational misuse, is the most likely to put users in serious danger. Additionally, it is worth noting that people with clinical histories of drug and alcohol abuse are more likely to engage in misuse.
Lorazepam Drug Interactions
One of the most high-risk drug combinations people often engage in is the concomitant use of CNS depressants. One only needs to look at the drug overdose statistics coming out of the United States to understand how deadly this combination can be. As CNS-depressant compounds, benzodiazepines, under no circumstance, should be mixed with other CNS depressants such as opioids and alcohol.
The possibility of CYP drug interactions also has to be taken into account. CYP enzymes, which metabolize a vast amount of prescription drugs, can be inhibited or induced by certain foods and compounds. If the CYP enzyme that metabolizes a given benzodiazepine is interfered with, this could have detrimental effects on the health of the patient and the outcome of their treatment.
Contraindications of Lorazepam
Contraindications are a common way users put themselves at risk. However, this information is readily available online. If a user needs clarification on the contraindications of their prescription medication, they can quickly look up this information.
However, certain contraindications are pretty common and should always be considered if they apply to you. These are special statuses like pregnancy, lactation, very young or very old age groups, renal or hepatic impairment, etc.
The FDA has identified the following contraindications for lorazepam:
- Acute narrow-angle glaucoma
- Hypersensitivity to benzodiazepines or any components of the formulation
- Pregnancy
Lorazepam Dosage
Maintaining proper dosage is essential to stay safe when using benzodiazepines. This can sometimes be harder than it sounds, as there are many complicating factors such as age, body weight, special statutes, indications, formulation, etc. In this sense, the best option is to always stick with whatever is indicated in your prescription.
However, there are good resources on the internet that can give you an idea of an appropriate dose. Just remember that formulaic internet recommendations can never consider all the possible factors related to your situation.
The Mayo Clinic lists the following recommended doses for the treatment of anxiety with lorazepam:
For oral dosage form (oral solution):
| 👩🏻🦱 Adults and children 12 years and older | 2 to 6 milligrams (mg) in divided daily doses. Your doctor may adjust your dose as needed. |
| 👨🏽🦳 Older adults | At first, 1 to 2 mg in divided doses per day. Your doctor may adjust your dose as needed. |
| 🧒🏼 Children younger than 12 years of age | Your doctor must determine the use and dose. |
For oral dosage form (tablets):
| 👩🏻🦱 Adults and children 12 years of age and older | At first, 2 to 3 milligrams (mg) in divided doses per day. Your doctor may adjust your dose as needed. |
| 👨🏽🦳 Older adults | At first, 1 to 2 mg in divided doses per day. Your doctor may adjust your dose as needed and tolerated. |
| 🧒🏼 Children younger than 12 years of age | Your doctor must determine the use and dose. |
For insomnia caused by anxiety or transient situational stress:
| 👩🏻🦱 Adults and children 12 years of age and older | 2 to 4 milligrams (mg) taken as a single dose at bedtime. Your doctor may adjust your dose as needed. |
| 🧒🏼 Children younger than 12 years of age | Your doctor must determine the use and dose. |
For oral dosage form (extended-release capsules):
| 👩🏻🦱 Adults | One capsule once a day in the morning. The dose is based on the total daily dose of lorazepam tablets, which you take three times a day in equally divided doses. Your doctor may adjust your dose as needed. |
| 🧒🏼Children | Use and dose must be determined by your doctor. |
Similar Benzodiazepines
Lorazepam is most closely-related to loprazolam but shares similarities in effects with common drugs like clonazolam (Klonopin), diazepam (Valium), alprazolam (Xanax), and many others.
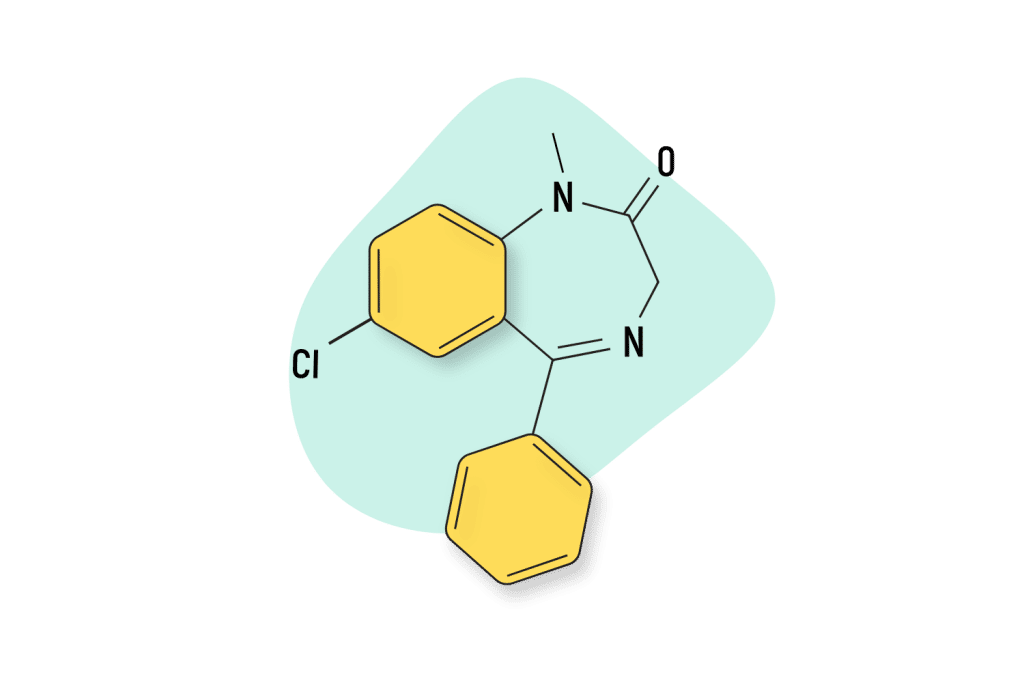
Lormetazepam
Lorazepam (Ativan) shares a similar chemical structure with lormetazepam (Loramet) — a relatively obscure sleeping pill used in some countries outside the United States.
Certain differences in loprazolam, mostly related to pharmacokinetics, make it more suited to its role as a hypnotic, while lorazepam is more successful as an anxiolytic.
Alprazolam (Xanax)
Alprazolam (Xanax) also shares a similar structure and mechanism of action as lorazepam. Both these drugs have comparable elimination half-lives. However, alprazolam is considerably more potent, which means it is taken at a reduced dose compared to lorazepam. A significant difference is that alprazolam is generally only prescribed to adults, while lorazepam has been found safe in children 12 and older.
Diazepam (Valium)
As a 1,4-benzodiazepine derivative, lorazepam shares many similarities with diazepam (Valium). However, there are meaningful differences as well. Lorazepam is classified as intermediate-acting benzo, while diazepam is a long-acting benzodiazepine. This implies significant differences in their pharmacokinetics and makes them better suited for slightly different clinical scenarios.
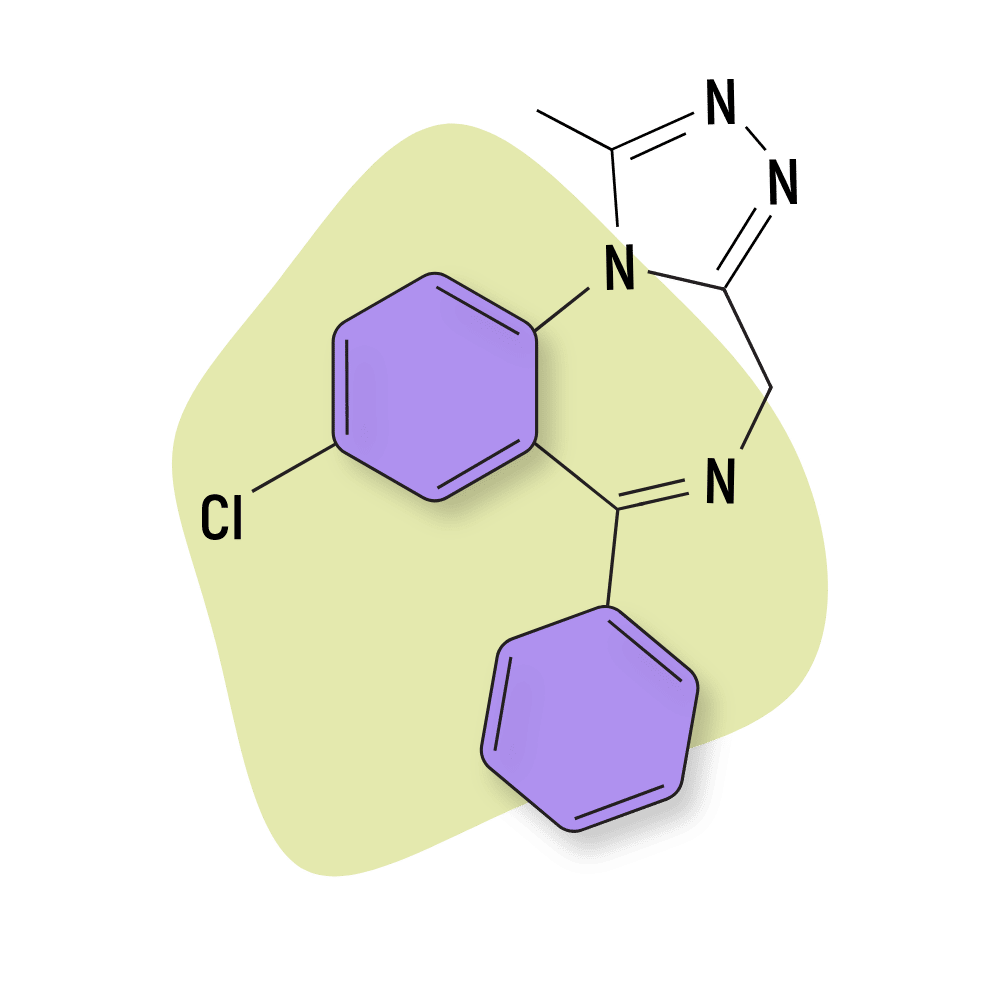
Meclonazepam (DBZD)
Meclonazepam is a designer benzodiazepine drug that takes after clonazepam. The purpose of designer drugs is to imitate other compounds while still being different enough to skirt legal regulations. Meclonazepam’s likeness to clonazepam means it is an intermediate-acting benzodiazepine with comparable pharmacokinetics to lorazepam.
Natural Alternatives to Benzodiazepines
The kava plant is a great option for those looking to try out a plant-based anxiolytic. In recent years, this plant has exploded in popularity because it can offer effective anxiolytic and sedative benefits while exhibiting a far-less dangerous side effects profile when compared with pharmacological alternatives [6].
There’s also the kratom plant, which offers anxiolytic and sedative benefits as well but can also offer stimulant and euphoric benefits depending on the dose [7].
Lorazepam FAQs
1. What formulations is lorazepam available in?
Lorazepam is available in 0.5 mg, 1 mg, and 2 mg tablets. It is also used in liquid solutions for intramuscular or intravenous injections in intrahospital settings.
2. Does lorazepam have any intrahospitalary indications?
Yes. It is used to disrupt the formation of memories during surgery and assist sedation in mechanical ventilation.
3. Is lorazepam a commercially popular benzodiazepine?
In 2019, lorazepam accounted for 20.9% of all benzodiazepine prescriptions.
4. Is lorazepam considered to be a high-potency benzodiazepine?
Yes, along with other benzodiazepines like alprazolam and clonazepam, lorazepam is considered a high-potency benzodiazepine, with a 1.3 mg dose roughly comparable to a 10 mg dose of diazepam.
References
- Ghiasi, N., Bhansali, R. K., & Marwaha, R. (2021). Lorazepam. In StatPearls [Internet]. StatPearls Publishing.
- Ameer, B., & Greenblatt, D. J. (1981). Lorazepam: A Review of its Clinical. Drugs, 21(3), 161-200.
- Campo-Soria, C., Chang, Y., & Weiss, D. S. (2006). Mechanism of action of benzodiazepines on GABAA receptors. British journal of pharmacology, 148(7), 984-990.
- Funderburk, F. R., Griffiths, R. R., McLeod, D. R., & George, E. (1988). Relative abuse liability of lorazepam and diazepam: an evaluation in ‘recreational’drug users. Drug and alcohol dependence, 22(3), 215-222.
- Riss, J., Cloyd, J., Gates, J., & Collins, S. (2008). Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta neurologica scandinavica, 118(2), 69-86.
- Cairney, S., Clough, A. R., Maruff, P., Collie, A., Currie, B. J., & Currie, J. (2003). Saccade and cognitive function in chronic kava users. Neuropsychopharmacology, 28(2), 389-396.
- Swogger, M. T., & Walsh, Z. (2018). Kratom use and mental health: A systematic review. Drug and Alcohol Dependence, 183, 134-140.