Cloniprazepam: Benzodiazepine Review & Analysis
Despite the risks, many people use designer benzos like cloniprazepam. We want everyone to be safe, so here’s what you need to know.
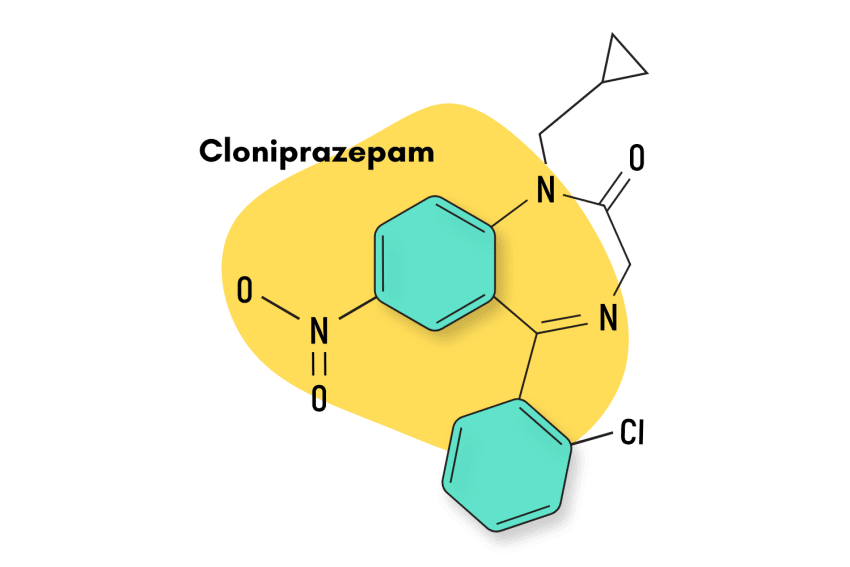
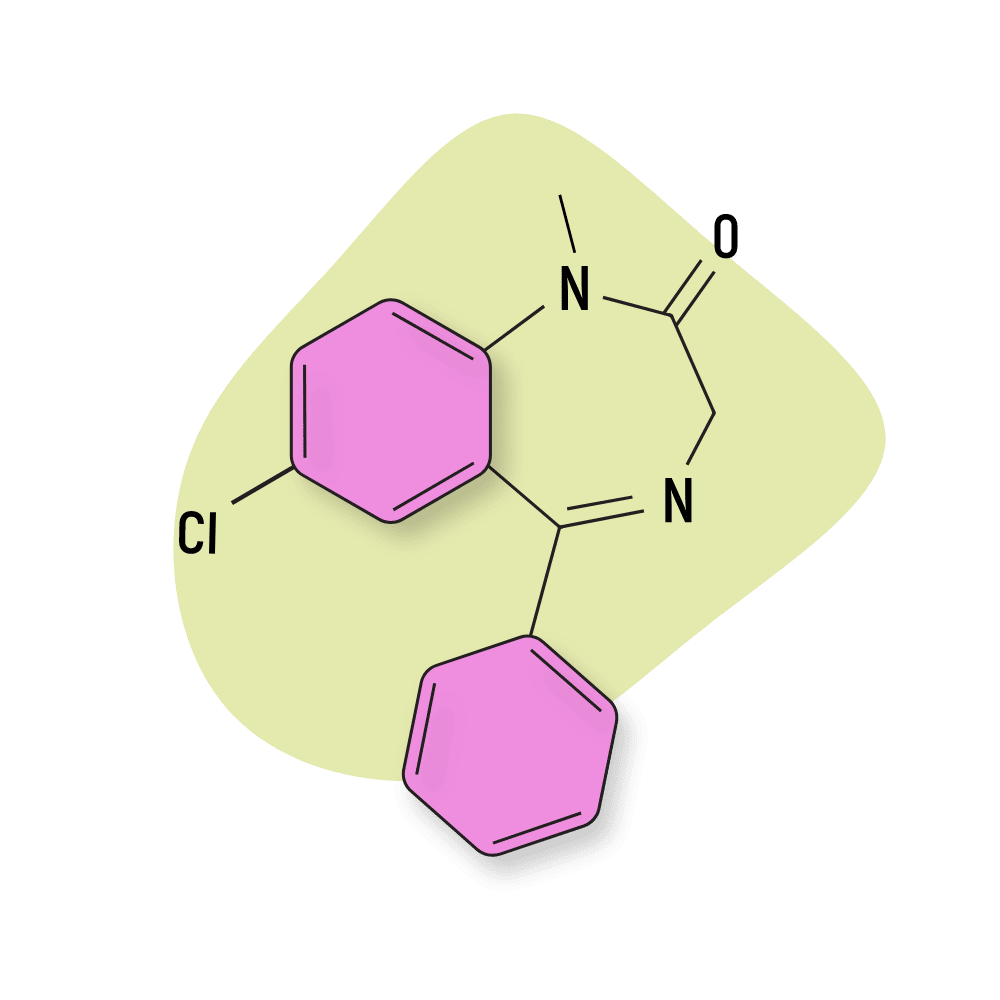
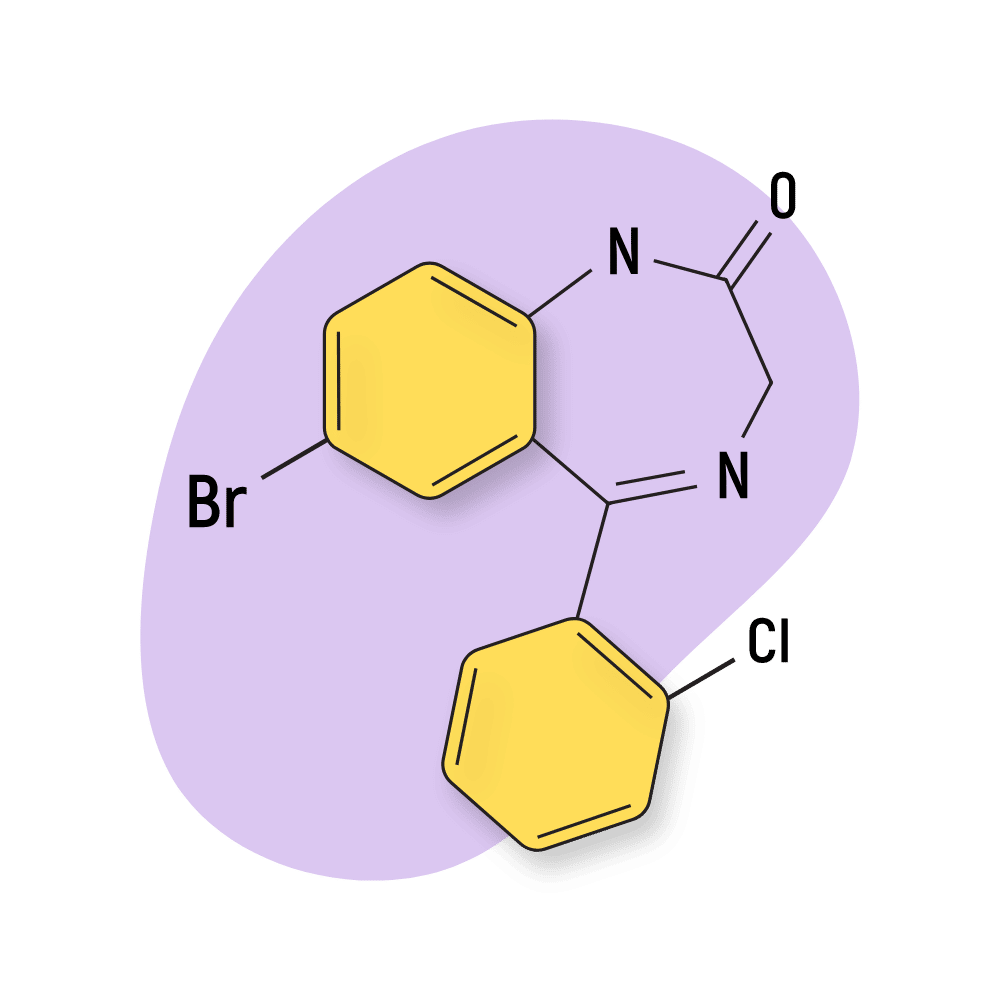
Cloniprazepam is a benzodiazepine drug and prodrug of the more common benzodiazepine, clonazepam (Klonopin).
Benzodiazepines like clonazepam are primarily used for treating panic disorders, anxiety, and seizures. Because of the accessibility and low price of designer benzodiazepines, people often self-prescribe or take benzodiazepines recreationally too.
There are not enough clinical studies for this drug to prove it’s safe for human consumption and carries significant risk for people looking to use this drug recreationally or off-label.
Cloniprazepam has never been approved as medicine in any country and is a designer drug [1].
Cloniprazepam Specs
| Status: | Not approved |
| Common Dosage: | 1 to 2 mg |
| PubChem ID: | 137700140 |
IUPAC Name: 5-(2-chlorophenyl)-1-(cyclopropylmethyl)-7-nitro-3H-1,4-benzodiazepin-2-one
Metabolism: Cloniprazepam is metabolized into 7-amino-cloniprazepam, hydroxy-cloniprazepam, 3-keto-cloniprazepam, clonazepam, hydroxy-clonazepam and 7-amino-clonazepam. The active metabolites are biotransformed into inactive metabolites by the cytochrome P450 enzymes, including the CYP3A4 enzyme [2].
Duration of Effects: It starts to work in 15 to 45 minutes, and the effects of the drug last for 6 to 9 hours [2].
What Is the Dose Of Cloniprazepam?
There is no approved dose of cloniprazepam.
However, for the sake of providing as much information about this drug as possible, here are some dosage recommendations for people taking this drug off-label. This information is based on user experience and binding affinity research involving cloniprazepam.
- Light dose — 0.5 to 1 mg
- Common dose — 1 to 2 mg
- Strong dose — 2 to 4 mg
How Does Cloniprazepam Work?
Like most other benzodiazepines, cloniprazepam works by binding and attenuating GABA A.
GABA is the body’s primary inhibitory molecule. When the mind becomes anxious and active, GABA steps in to slow things down.
GABA works by binding to the receptor, causing rapid hyperpolarization and reduction in neuronal excitation [3]. In other words, it inhibits the neurons’ ability to transmit information, thus stopping the transmission of messages throughout the brain and slowing down activity.
GABAergic drugs like cloniprazepam also lead to a variety of other effects — including sedation and skeletal muscle relaxation. This occurs because GABA receptors are located throughout the peripheral and central nervous systems (throughout the body and brain) [4].
Additionally, it reduces nerve transmission in the motor cortex, suppressing the spike and wave-like brain electrical patterns and minimizing the occurrence of seizures [5, 6].
Cloniprezapam is largely metabolized into the active compound clonazepam (Klonopin).
Is Cloniprazepam Safe? Risks & Side-Effects
Cloniprazepam has never been clinically tested or approved for medical use. It’s a research chemical and carries all the same risks as other research chemicals (unknown side effects and safety profile, issues with adulteration or impurities, etc.).
Although the pharmacological profile of the drug is similar to that of other benzodiazepines like clonazepam, it has not been studied properly or confirmed to be safe.
The side effects of the drug are likely very similar to its active metabolite, clonazepam. In high concentrations, clonazepam can result in sedation, breathing problems, intoxication, and coma.
Side Effects of Cloniprazepam
Common side effects of cloniprazepam include:
- Blurred vision
- Cognition problems, such as problems with memory, thinking, and attention
- Frequent urination
- Increased salivation
- Lightheadedness, drowsiness, and dizziness
- Low mood
- Muscle weakness, balance problems, and increased risk of fall
- Sexual issues such as reduced sex drive
- Sleep disturbances
Serious side effects appear to be rare but are not impossible. If you experience any of the following side effects, visit your doctor immediately.
Serious side effects of cloniprazepam:
- Anaphylaxis
- Coma
- Confusion and slurring of speech
- Delirium
- Dementia
- Disinhibition and increased risk-taking behavior
- Extreme sedation or dizziness
- Respiratory distress
- Signs of liver problems, such as yellowish discoloration of the skin and eyes
Harm Reduction: Cloniprazepam
Since the drug is not approved for clinical use, it is better to use other approved benzodiazepines under prescription, such as clonazepam, alprazolam, and diazepam. However, the following instructions can reduce the risk associated with cloniprazepam.
Benzodiazepine Harm Reduction Tips:
- 🥣 Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- ⏳ Take frequent breaks or plan for a short treatment span — Benzodiazepines can form dependence quickly, so it’s important to stop using the drug periodically.
- 🥄 Always stick to the proper dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- 💊 Be aware of contraindications — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- 🧪 Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- 💉 Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Only take benzos orally.
- 🌧 Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- ⚖️ Understand the laws where you live — In most parts of the world, benzodiazepines are only legal if given a prescription by a medical doctor.
- 📞 Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Look up “addiction hotline” for more information. (USA: 1-800-662-4357; Canada: 1-866-585-0445; UK: 0300-999-1212).
Reducing the Risk Of Benzodiazepine Dependence
Taking the drug for a short time can reduce the risk of dependency. Furthermore, reducing the dose slowly before completely stopping the drug might also be helpful.
Avoiding Certain Activities
Cloniprazepam can cause sedation and drowsiness. Avoid activities requiring attention, such as driving, swimming, and operating heavy machinery.
Avoid Drinking Alcohol When Taking Cloniprazepam
Alcohol can aggravate the sedative effects of cloniprazepam and can cause deep sleep or coma. So, it is better to avoid alcohol consumption while taking cloniprazepam.
Discuss Your Drug & Allergy History With Your Doctor
Sedatives such as other benzodiazepines, opioids, SSRIs, antihistamines, phenobarbitol, and phenytoin can cause deep sleep, breathing problems, and coma. Avoid these medicines while taking cloniprazepam. Discuss with your doctor any other medicines, supplements, or herbs you take.
Take Precaution for Certain Medical Conditions
Inform your doctor if you have any health conditions, as cloniprazepam may worsen them.
You need to be especially careful before consuming cloniprazepam if you have any of the following medical conditions:
- Acute angle closure glaucoma
- Chronic Kidney disease
- Chronic liver disease
- Conditions affecting breathing, such as COPD and sleep apnea
- Pregnancy and lactation
- Psychosis
Similar Benzodiazepines
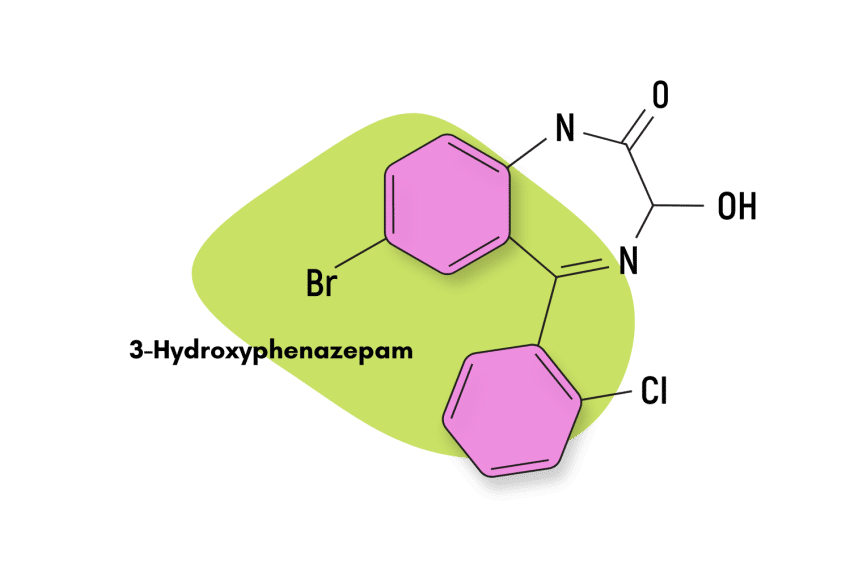
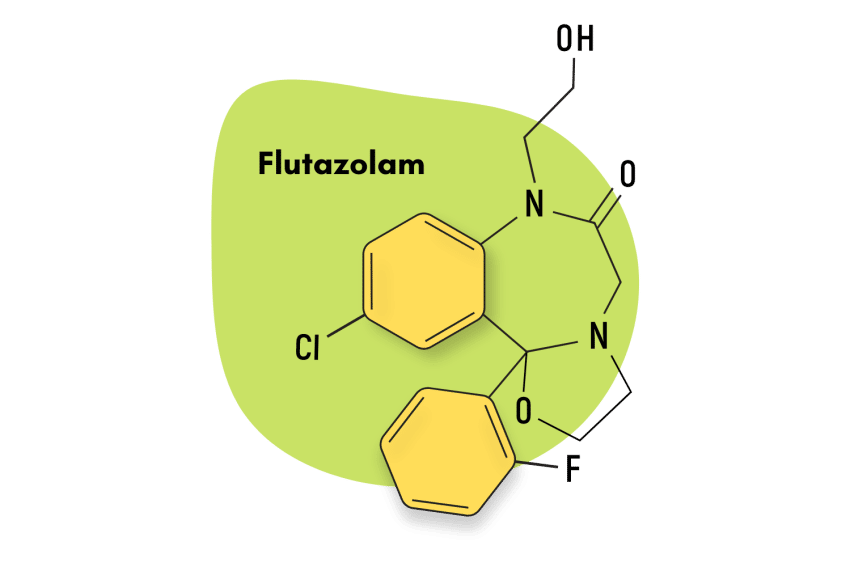
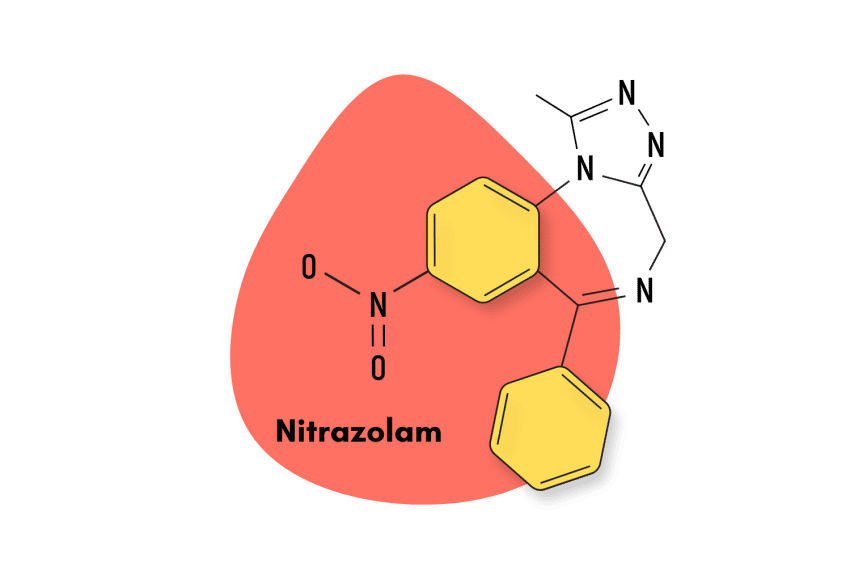
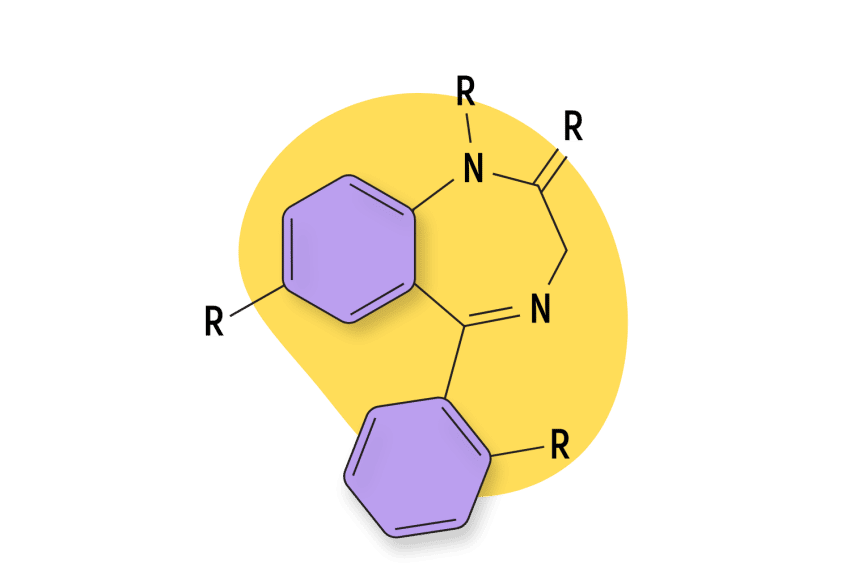
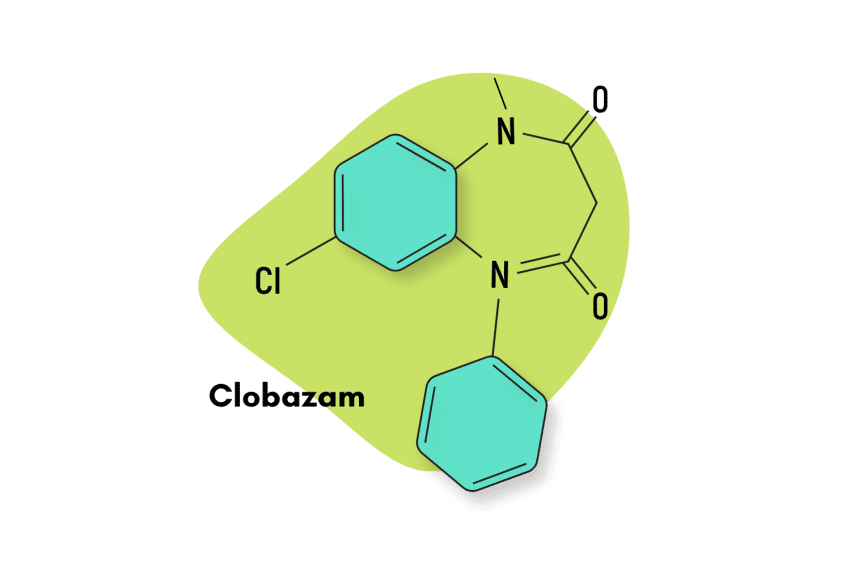
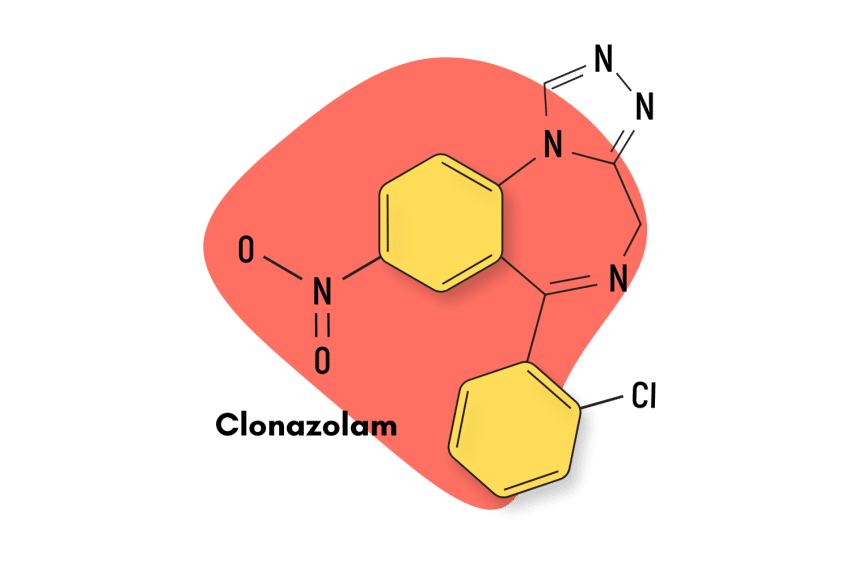
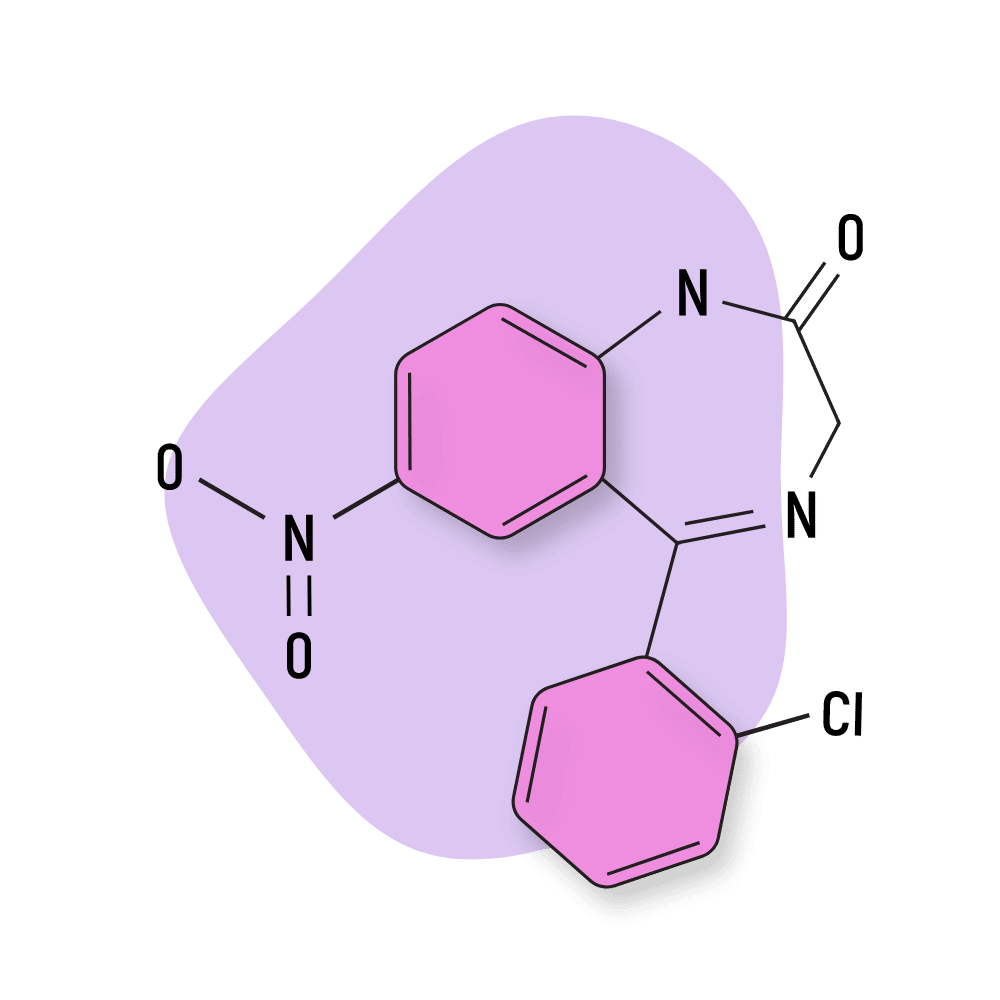
Recently, many novel psychoactive substances fall under the benzodiazepine class, with activity similar to cloniprazepam. These are mostly formed by modifying the core structure of the existing controlled benzodiazepines.
Some of the common novel psychoactive substances with activities similar to those of cloniprazepam are
1. Clonazepam
Clonazepam is a widely used benzodiazepine to treat anxiety, panic disorders, and insomnia.
Like most benzos, it also has a risk of causing dependence. Because it is a long-acting benzo with an intermediate onset of action, it is commonly used in treating sleep disorders.
2. Diazepam
Diazepam (Valium) was one of the first-ever benzodiazepines to hit the market. This compound is still popular today and serves as the baseline when comparing the effects of other benzodiazepines.
Diazepam is long-lasting and tends to hit a little harder in terms of intoxicating effects than cloniprazepam.
3. Alprazolam
Alprazolam (Xanax) is, by far, one of the most used benzos on the market today (both legally and illegally). It’s mildly euphoric, fast-acting, and relatively safe when used responsibly.
This short-acting benzo does carry a higher risk of abuse and dependence, however. Users who take this drug often need to re-dose 2 or 3 hours later — which can quickly lead to habit formation and, eventually, dependency.
4. Bromazepam
Bromazepam (Lectopam) is most similar to diazepam but shares some similarities to cloniprazepam as well. This compound is ubiquitous, and hundreds of drug manufacturers around the world make generic forms.
5. Chlordiazepoxide
Chlordiazepoxide (Librium) was the first benzo to enter the market and boasts one of the longest-duration of effects of any benzodiazepine drug.
6. Phenazepam
Phenazepam is a very long-acting, potent benzodiazepine with a similar effect profile to cloniprazepam. This drug is known to remain active for 18 hours or longer and is often used to potentiate (make stronger) the effects of opiates (high-risk combination).
Some users suggest phenazepam as a tool for reducing the withdrawal symptoms of opiates or to balance cocaine ‘highs’ [7].
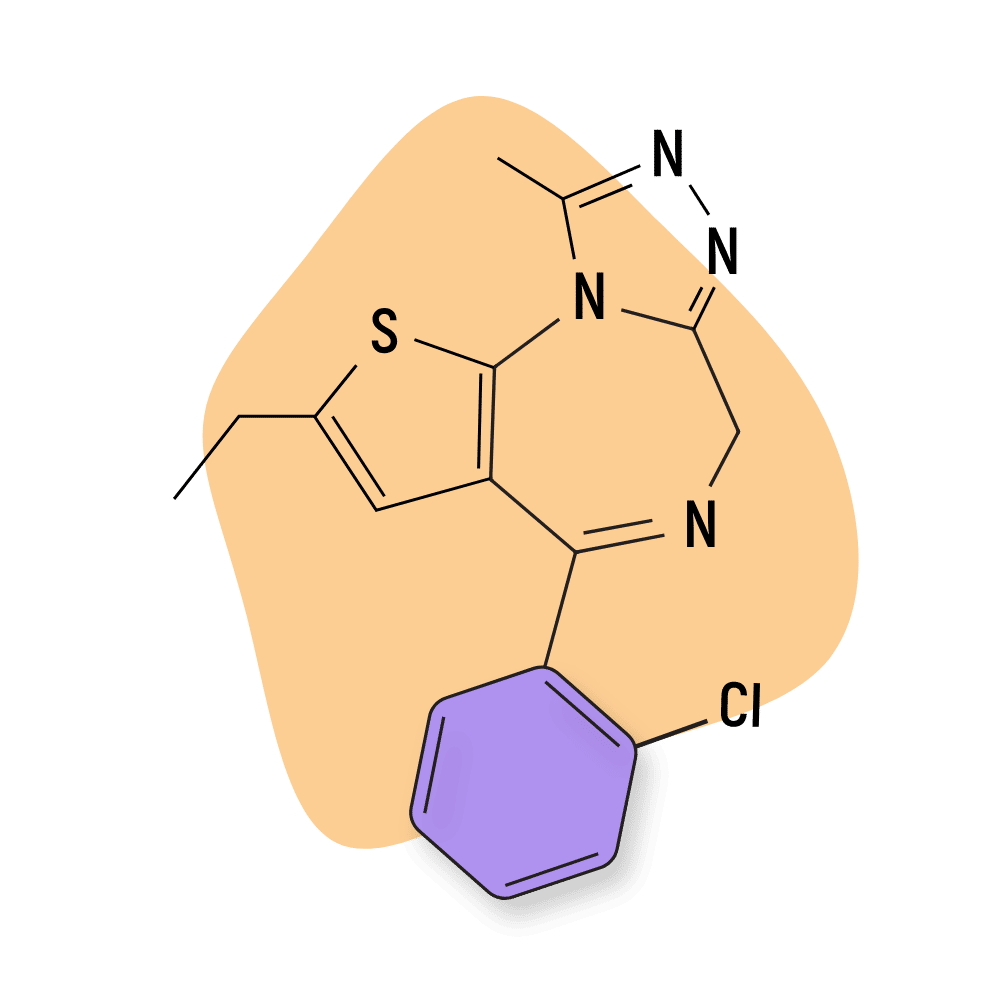
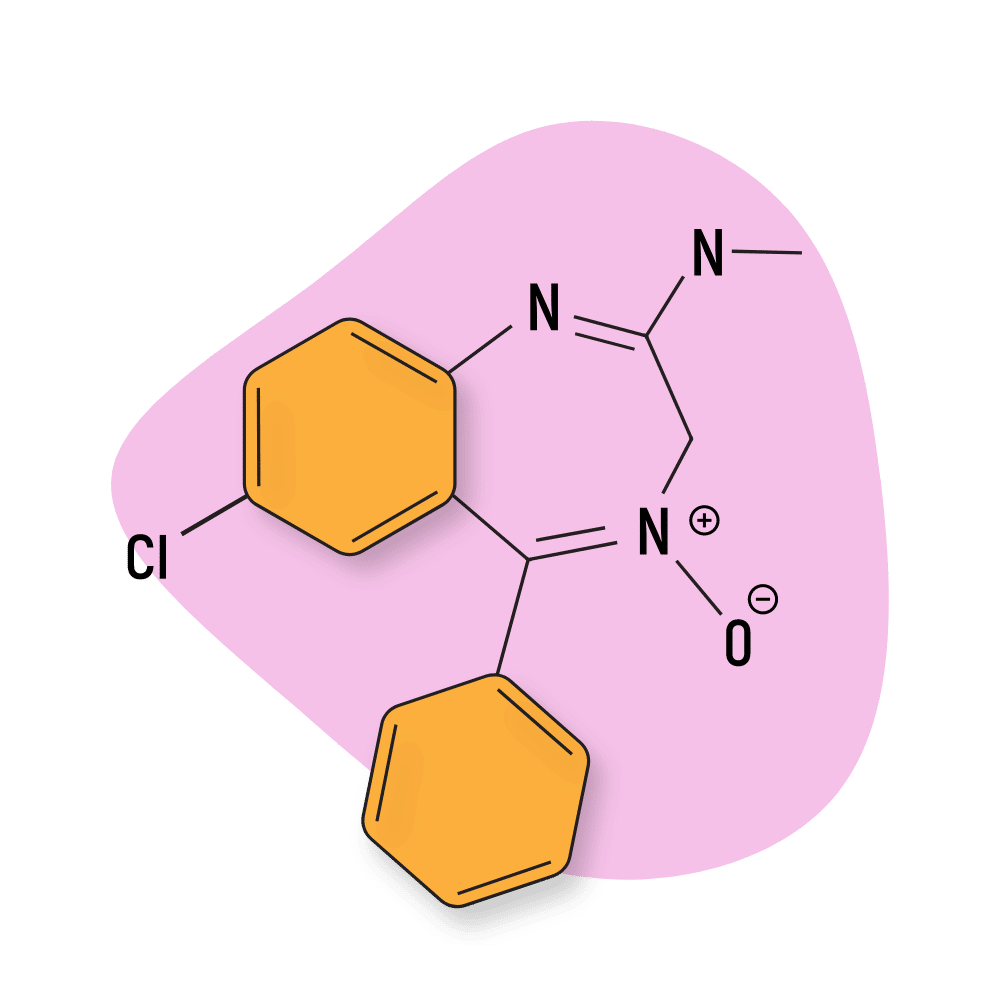
7. Etizolam
Etizolam is one of the more popular designer benzodiazepines, especially in Europe [8]. It was one of the first to enter the ‘legal drug’ market in the mid-2000s and has remained popular ever since.
New laws place etizolam as a Schedule IV drug in the United States, which makes it illegal unless prescribed by a doctor. Because etizolam isn’t approved by the FDA, there are no accepted legal reasons for being in possession of this drug.
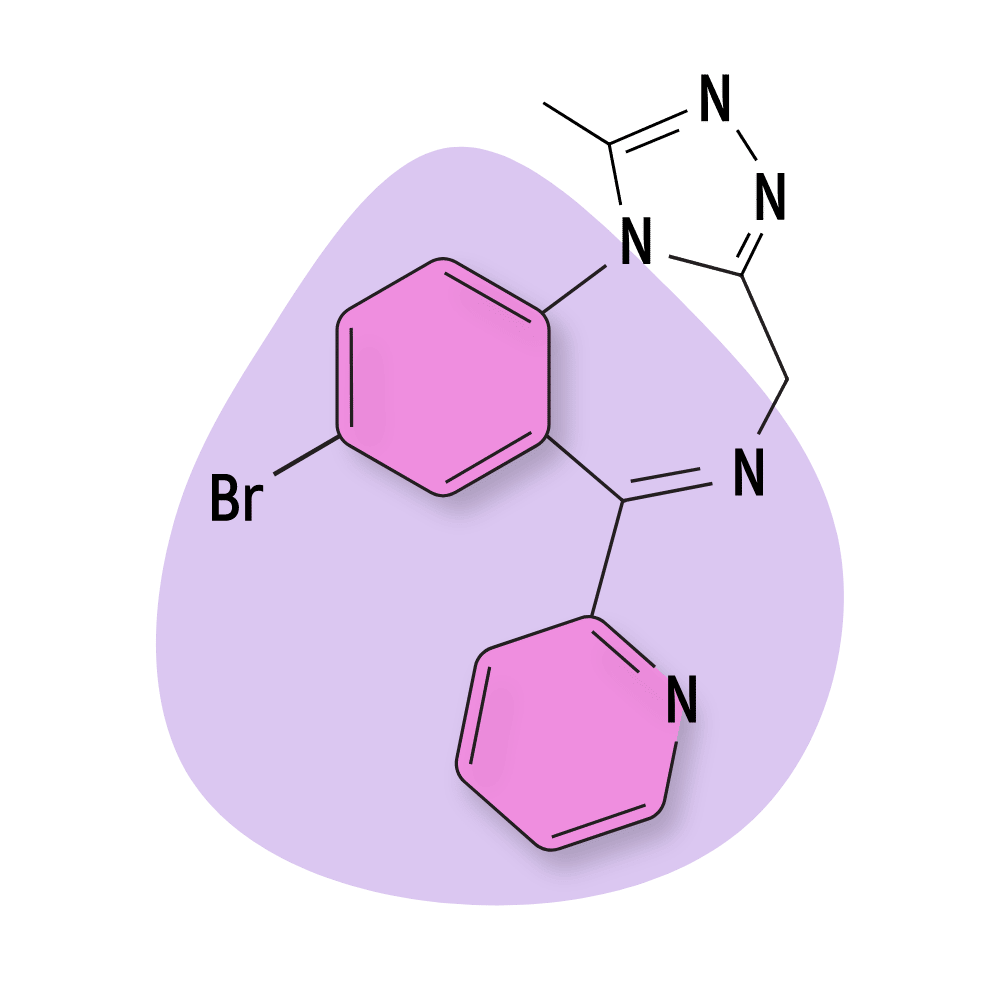
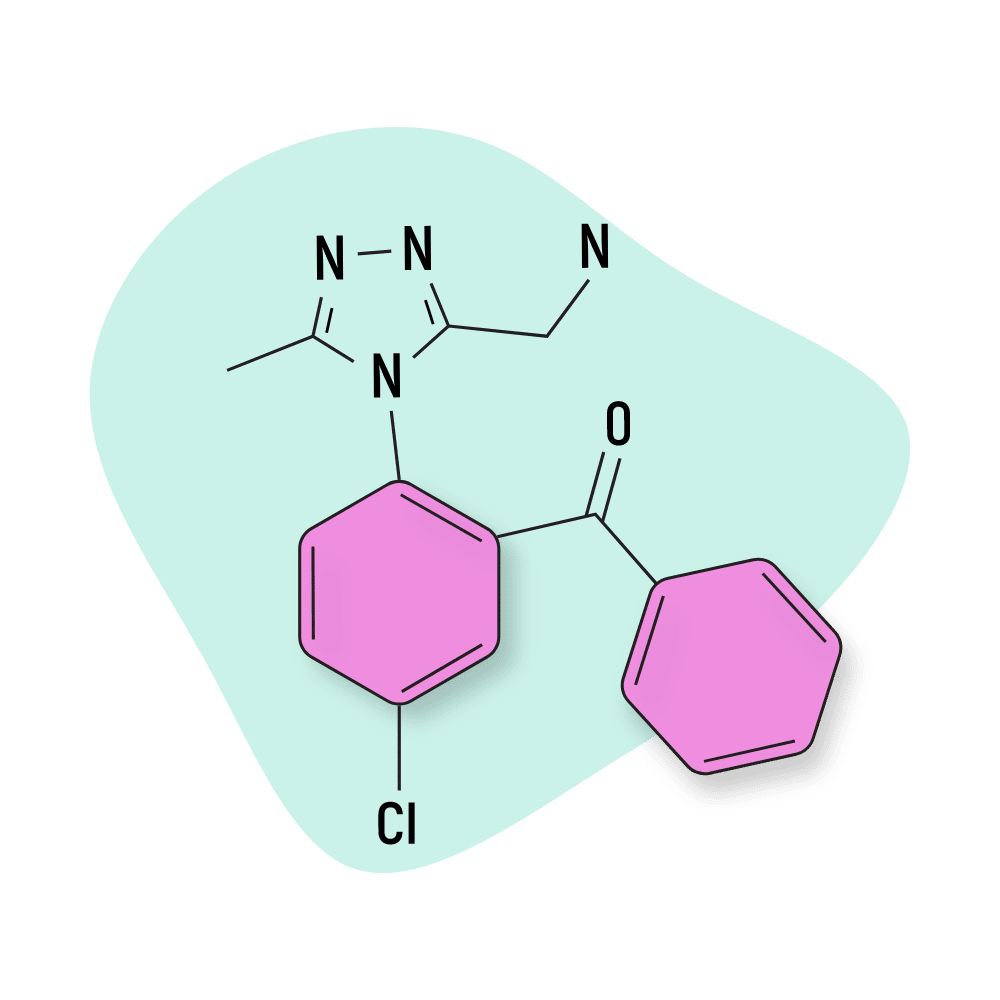
8. Pyrazolam
Users who take pyrazolam often suggest this compound is less likely to result in problems associated with sedation. It’s often considered more of a “social” benzodiazepine in the sense that it causes many of the same carefree, relaxed, and buzzed feelings benzos are known for, but it doesn’t make you pass out while you’re spending time with other people.
The effects of pyrazolam generally last around 6 or 7 hours in total.
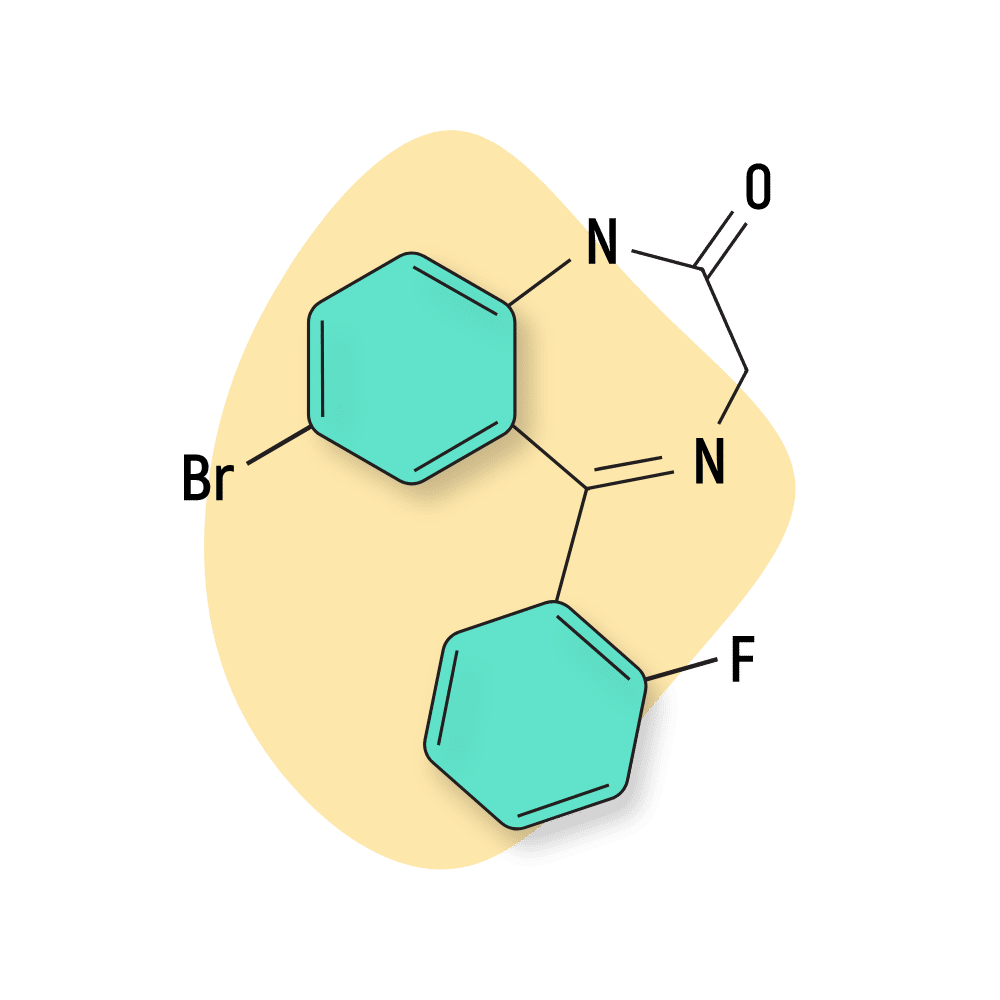
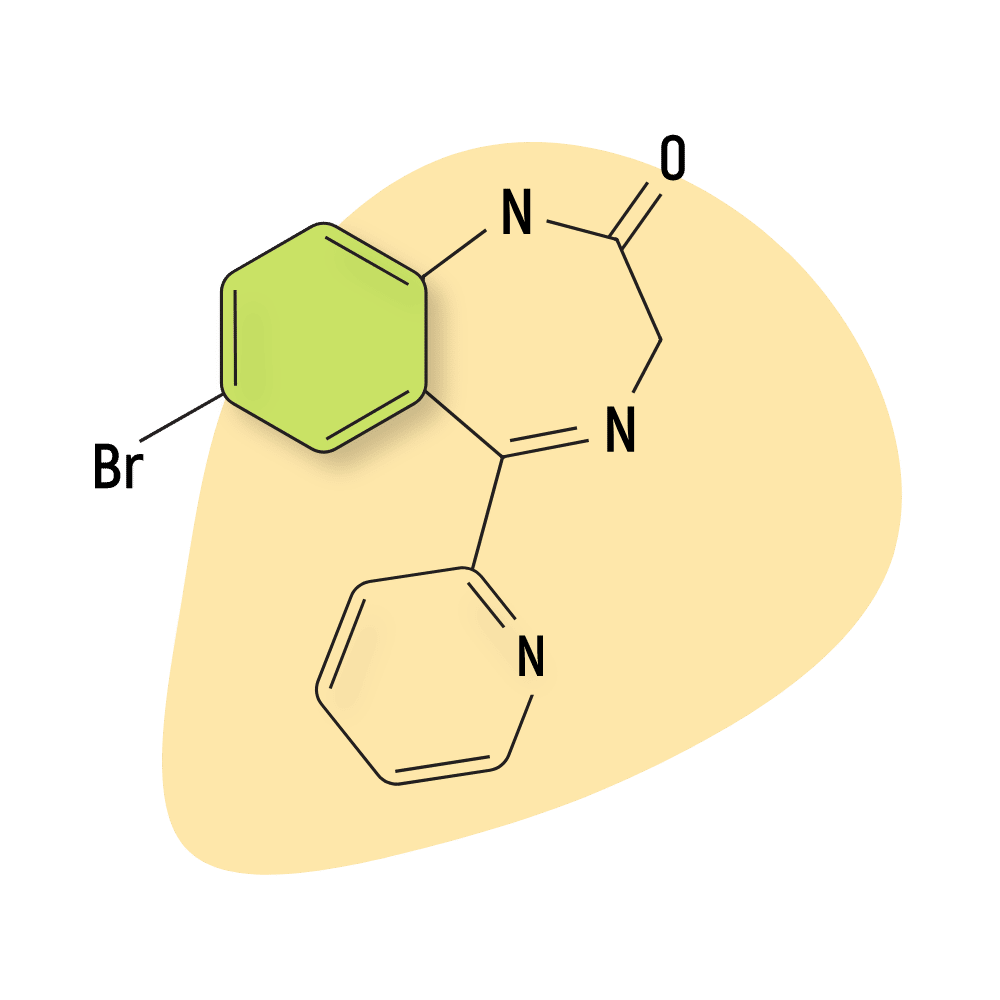
9. Flubromazepam
Flubromazepam is a long-acting drug with similar effects to cloniprazepam but can cause mild euphoria and short-term memory loss. This compound is more obscure than others on this list, but there’s evidence that public interest is increasing. It’s likely the euphoric component of flubromazepam is the leading factor in this growth.
Cloniprazepam vs. Other Short To Intermediate-Acting Benzodiazepines [9,10]:
| Cloniprazepam | Alprazolam | Bromazepam | Diazepam | Chlordiazepoxide | |
| Chemical composition: | 15-(2-Chlorophenyl)-1-(cyclopropylmethyl)-7-nitro-3H-1,4-benzodiazepin-2-one | Benzodiazepine with a triazole ring attached to its structure | 1,4-benzodiazepine | 1,4-benzodiazepine | 1,4-benzodiazepine |
| Route of administration: | Oral | Oral | Oral | IV, IM | Oral, IV |
| Onset of action: | 115 to 45 minutes | 20 to 60 minutes | 60 minutes | 15 to 60 minutes | 1 to 2 hours |
| Peak concentration: | 11 to 2 hours | 1 to 2 hours | 1 to 4 hours | 1 to 1.5 hours | 2 hours |
| Duration of effects: | Intermediate-acting (6 to 17 hours) | Short-acting (6 to 27 hours) | Intermediate-acting (8 to 19 hours) | Long-acting (20 to 80 hours) | Long-acting (36 to 200 hours) |
| Mechanism of action: | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist | GABA-A receptor agonist |
| Medical Uses: | Panic disorders, seizures, anxiety | Panic disorders, anxiety disorders, insomnia | Anxiety disorder, alcohol withdrawal | Seizures, alcohol withdrawal, insomnia, muscle spasms, panic disorder, anxiety disorders | Panic disorders, alcohol withdrawal, anxiety disorders |
Natural Alternatives To Benzodiazepines
There are few natural alternatives that cause relaxation and sedation like benzodiazepines.
Some natural alternatives to cloniprazepam are
1. L-Theanine
It is an amino acid found in Camellia sinensis (the tea plant), and popular for its calming and relaxing effects. It helps reduce anxiety by enhancing GABA’s inhibitory effects [11].
2. Kava
Kava (Piper methysticum) is a traditional tea used for many years for several health benefits. You can get it as an over-the-counter herbal medicine for anxiety, stress, and sleep problems. It exerts sedative effects by increasing the activity of GABA through various kavalactones [12].
3. Gotu Kala
Gotu Kala (Centella asiatica) is an ancient Chinese herb used to treat anxiety, depression, and mental fatigue. It also helps with insomnia by providing a calming effect through GABAergic mechanisms [13].
4. Psychobiotics
Psychobiotics are specific probiotics that are beneficial for mental health disorders. These consist of bacterial strains which synthesize neurotransmitters such as GABA. Lactobacillus brevis and Bifidobacterium dentium are two common bacteria that synthesize GABA. Additionally, probiotics also reduce the level of stress hormones to reduce stress and provide calming effects [14].
5. GABA Supplements
Although GABA is the major inhibitory neurotransmitter, providing relaxing effects, GABA supplements are not as effective as benzodiazepines. These medications cannot cross the blood-brain barrier (BBB) when taken orally.
However, some studies show that a higher dose of GABA supplements is comparable to benzodiazepines for managing anxiety or depression [15].
Cloniprazepam FAQs
Here are some of the most common questions we get asked about cloniprazepam and related benzodiazepines:
1. Is cloniprazepam approved for medicinal use?
Cloniprazepam is legal to use and possess. However, it is not approved for clinical use, and further study is underway to study its effectiveness and safety profile. The drug is approved for use for research purposes only.
2. How does cloniprazepam differ from clonazepam?
Clonazepam is an active drug, but cloniprazepam is a prodrug that metabolizes to clonazepam. So, the drug has a longer duration of action. Clonazepam is an approved drug and should only be used if you have a prescription. However, cloniprazepam is not approved for medical use.
3. Is there a risk of getting addicted to cloniprazepam?
Yes, there is a risk of getting addicted to cloniprazepam. However, minimize the risks by taking the drug for a short period of time. Additionally, you should not abruptly stop the drug intake to avoid withdrawal symptoms. You should gradually reduce the dose of the drug before stopping it completely.
4. Are there any precautions that should be followed while taking cloniprazepam?
You should avoid activities that require attention and are associated with high risks, such as driving, working with electricity, and operating heavy machinery. Additionally, you should avoid other sedatives such as alcohol, opioids, and antihistamines while taking cloniprazepam.
5. When did cloniprazepam first appear on the grey market?
Swedish police first identified cloniprazepam on December 2nd, 2015, and is not listed under the 1971 United Nations Convention on Psychotropic Substances or the 1961 Single Convention on Narcotic Drugs.
References
- Orsolini, L., Corkery, J. M., Chiappini, S., Guirguis, A., Vento, A., De Berardis, D., … & Schifano, F. (2020). ‘New/Designer Benzodiazepines’: an analysis of the literature and psychonauts’ trip reports. Current neuropharmacology, 18(9), 809-837.
- Mortelé, O., Vervliet, P., Gys, C., Degreef, M., Cuykx, M., Maudens, K., … & Lai, F. Y. (2018). In vitro Phase I and Phase II metabolism of the new designer benzodiazepine cloniprazepam using liquid chromatography coupled to quadrupole time-of-flight mass spectrometry. Journal of pharmaceutical and biomedical analysis, 153, 158-167.
- DeVane, C. L., Ware, M. R., & Lydiard, R. B. (1991). Pharmacokinetics, pharmacodynamics, and treatment issues of benzodiazepines: alprazolam, adinazolam, and clonazepam. Psychopharmacology bulletin, 27(4), 463-473.
- E Nardi, A., Machado, S., Ferreira Almada, L., Paes, F., Cardoso Silva, A., Jose Marques, R., … & Arias-Carrión, O. (2013). Clonazepam for the treatment of panic disorder. Current Drug Targets, 14(3), 353-364.
- Hosford, D. A., Wang, Y., & Cao, Z. (1997). Differential effects mediated by GABAA receptors in thalamic nuclei in lh/lh model of absence seizures. Epilepsy research, 27(1), 55-65.
- Jenner, P., Pratt, J. A., & Marsden, C. D. (1986). Mechanism of action of clonazepam in myoclonus in relation to effects on GABA and 5-HT. Advances in neurology, 43, 629-643.
- Maskell, P. D., De Paoli, G., Seetohul, L. N., & Pounder, D. J. (2012). Phenazepam: the drug that came in from the cold. Journal of forensic and legal medicine, 19(3), 122-125.
- Nielsen, S., & McAuley, A. (2020). Etizolam: a rapid review on pharmacology, non‐medical use and harms. Drug and Alcohol Review, 39(4), 330-336.
- Griffin, C. E., Kaye, A. M., Bueno, F. R., & Kaye, A. D. (2013). Benzodiazepine pharmacology and central nervous system–mediated effects. Ochsner Journal, 13(2), 214-223.
- National Center for Biotechnology Information (2022). PubChem Compound Summary for CID 137700140, Cloniprazepam.
- Higashiyama, A., Htay, H. H., Ozeki, M., Juneja, L. R., & Kapoor, M. P. (2011). Effects of l-theanine on attention and reaction time response. Journal of Functional Foods, 3(3), 171-178.
- Chua, H. C., Christensen, E. T., Hoestgaard-Jensen, K., Hartiadi, L. Y., Ramzan, I., Jensen, A et al. (2016). Kavain, the major constituent of the anxiolytic kava extract, potentiates GABAA receptors: functional characteristics and molecular mechanism. PLoS One, 11(6), e0157700.
- Gohil, K. J., Patel, J. A., & Gajjar, A. K. (2010). Pharmacological review on Centella asiatica: a potential herbal cure-all. Indian journal of pharmaceutical sciences, 72(5), 546.
- Perez-Burgos A, Wang B, Mao YK, Mistry B, McVey Neufeld KA, Bienenstock J, Kunze W. Psychoactive bacteria Lactobacillus rhamnosus (JB-1) elicits rapid frequency facilitation in vagal afferents. Am J Physiol Gastrointest Liver Physiol. 2013 Jan 15;304(2):G211-20. doi: 10.1152/ajpgi.00128.2012. Epub 2012 Nov 8. PMID: 23139216.
- Boonstra, E., De Kleijn, R., Colzato, L. S., Alkemade, A., Forstmann, B. U., & Nieuwenhuis, S. (2015). Neurotransmitters as food supplements: the effects of GABA on brain and behavior. Frontiers in psychology, 1520.