Bromazepam 101: Safety, Risks, Dosage & More
Bromazepam — sold commercially as Lexotan — is a prescription benzodiazepine medication used to treat anxiety-related symptoms and disorders.
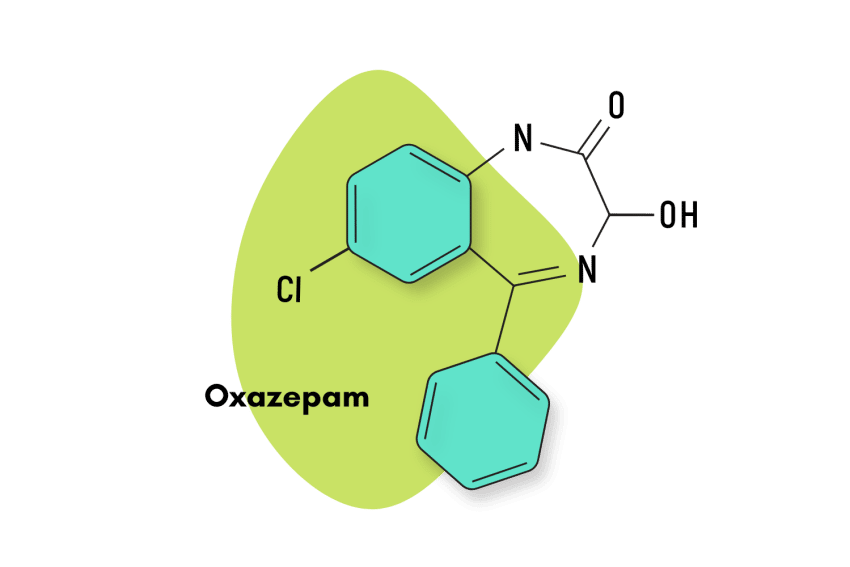
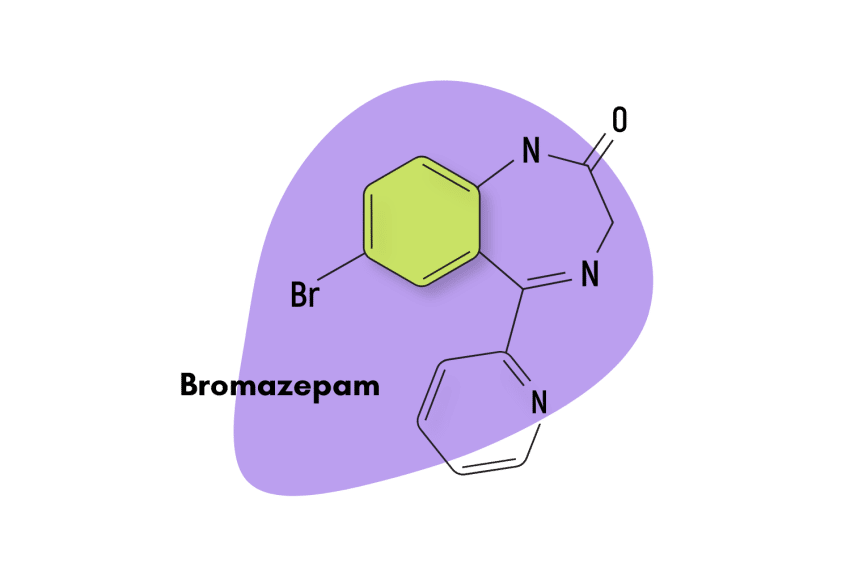
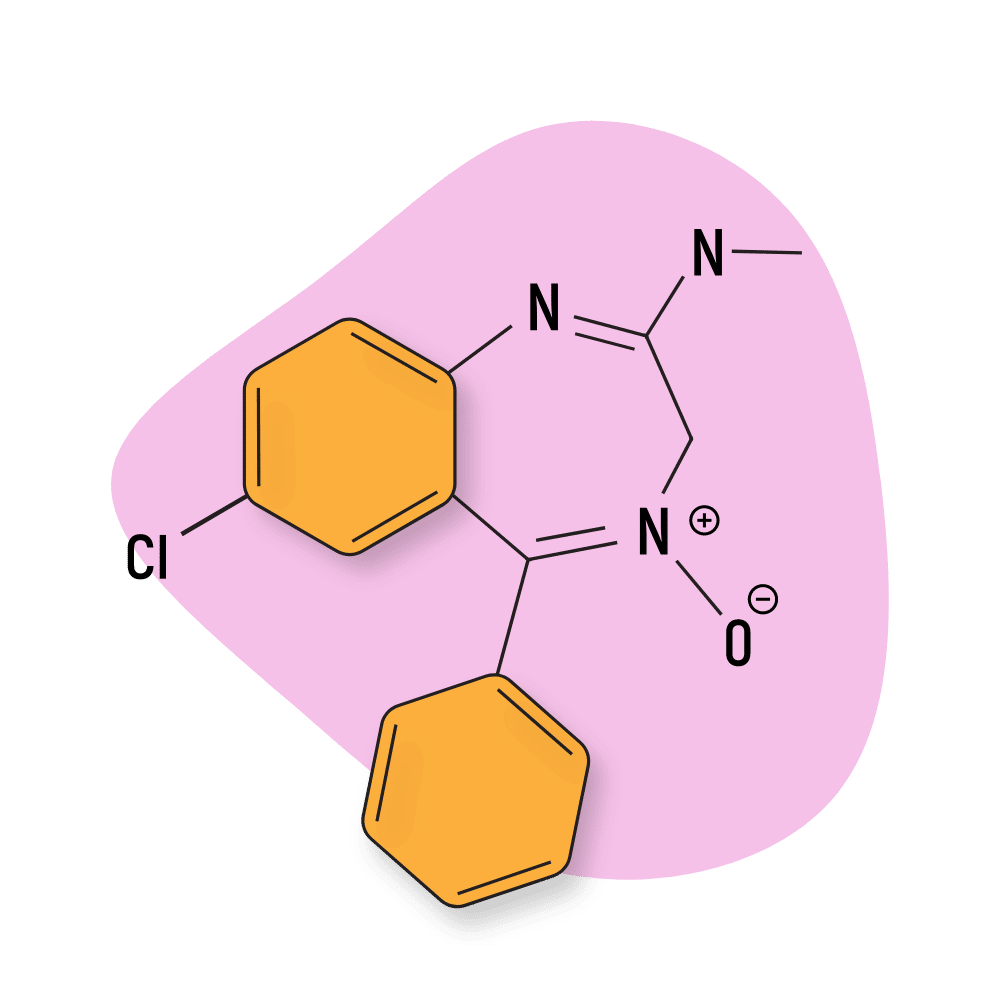
First patented in 1961 and then approved for medical use in 1974, bromazepam is a traditional 1,4 benzodiazepine similar to diazepam. This means the nitrogens on the seven-sided diazepine ring are in the 1 and 4 positions.
Bromazepam is classified as a high-potency benzodiazepine with comparable potency to drugs like lorazepam and triazolam. It’s also notoriously long-lasting because several of its metabolites are active too.
Like most other benzodiazepines, in high doses, bromazepam exhibits sedative and muscle-relaxant properties. This drug has a high risk for addiction and abuse.
Bromazepam Specs
IUPAC Name: 7-bromo-5-pyridin-2-yl-1,3-dihydro-1,4-benzodiazepin-2-one
Other Names: Brozam, Lectopam, Lexomil, Lexotan, Lexilium, Lexaurin, Brazepam, Rekotnil, Bromaze, Somalium, Lexatin, Calmepam, Zepam, & Lexotanil.
Metabolism: According to its manufacturer, the specific enzymes involved in the metabolism of bromazepam have not been fully elucidated. There is evidence to suggest that CYP2D6 does inhibit its metabolism, but more research is needed [9].
Duration of Effects: Intermediate-Acting (20–40 hours). The onset of action with bromazepam occurs in 15-30 minutes.
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Bromazepam Work?
By and large, benzodiazepines all share the same basic mechanism of action, which produces their signature anxiolytic, hypnotic, anti-seizure, and muscle relaxant properties through an inhibitory effect on the brain and central nervous system (CNS.)
A couple of benzodiazepines have novel and distinct ways to go about this. Still, the majority of them exert their actions through the gamma-aminobutyric acid neurotransmitter, also known as GABA. GABA receptors are the chief inhibitory compound in the mature vertebrate central nervous system.
As a traditional benzodiazepine, bromazepam is known to bind with the α1, α2, α3, and α5 GABA-A subunits but not with α4 and α6. What is less understood, though, are the reasons for this specificity and the exact way each subunit triggers a different effect [3].
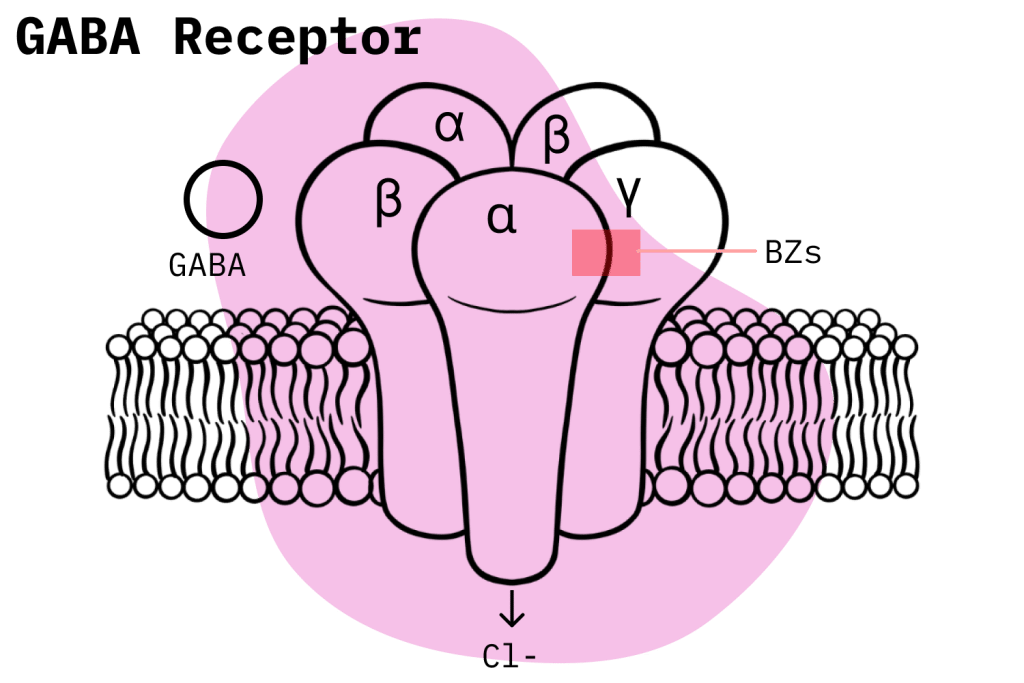
Out of the two types of GABA receptors, benzodiazepines bind to GABA-A at a different site where GABA-A binds and produce an allosteric effect. In other words, they potentiate the natural inhibitory mechanism of the GABA-A compounds. This is an important point of difference: unlike barbiturates, benzodiazepines are not GABA receptor activators; they work by increasing the natural activity of the GABA neurotransmitter [1].
GABA-A receptors have a complicated structure, and there still is a lot we don’t know about the way benzodiazepines exert their effects. However, we do know the GABA-A receptors are made up of a total of 19 different subunits. And we also know that differences in the activation of these distinct subunits accounts for the variations in the effects profile of benzodiazepines. In other words, which subunits a benzodiazepine binds to has a major role in determining its effects [2].
Once a benzodiazepine binds to a GABA-A molecule, the passage of negatively charged chloride ions into the neurons increases. This causes the neuron to become hyperpolarized and thus less likely to fire off an action potential: the electrical signals that are used by the body’s neurons communicate.
With the neurons in the brain and CNS now less likely to send an action potential, total brain activity is reduced, and the effects of the benzodiazepines are achieved. Also, long-lasting benzodiazepines are generally more attuned to use as anxiolytic agents, while shorter-acting benzodiazepines are more used as hypnotics.
Is Bromazepam Safe? Risks & Side-Effects
It’s important to understand the general situation regarding benzodiazepine misuse in the United States before we look at the specific situation of bromazepam.
Benzodiazepine Misuse Statistics
The National Institute on Drug Abuse (NIDA) has documented how drug overdose deaths involving benzodiazepines have steadily risen since 1999. The deaths plateaued for a while in 2010 but started rising again in 2014. An important point to note is that after 2014, deaths involving both benzodiazepines and opioids account for a much larger percentage of fatalities.
Recently, a 2020 survey by the CDC showed that benzodiazepines were involved in 12.290 deaths in the US. Additionally, the NIDA published another study that claims 16% of overdose deaths involving opioids also had the presence of benzodiazepines.
In response to these worrying trends, in 2016, the FDA issued a black box warning to deter users from the potentially fatal dangers of concomitant opioid and benzodiazepine use. In general, combining any two nervous system depressants is a bad idea as it increases the risk of respiratory depression, the leading cause of drug overdose deaths.
Bromazepam Misuse
Under the Controlled Substances Act, bromazepam is currently listed as a Schedule IV compound. This means that bromazepam has widely accepted medical uses but is still capable of causing physical dependence and has the potential for misuse. In general, the consensus among experts is that deaths stemming from single-drug benzodiazepine use are rare but do happen.
As a benzodiazepine, bromazepam has largely fallen out of use in recent years and is no longer available in the United States. Consequently, almost no figures can tell us how it fits in among other benzodiazepines in terms of toxicity. However, there are some things we can reasonably infer.
As a high-potency benzodiazepine with pharmacologically active metabolites, it could be reasoned that bromazepam is among the more dangerous in its class. Also, acute bromazepam poisoning can cause a prolonged coma [4]. A 2015 study conducted over a two-year time period pointed to bromazepam as the leading benzodiazepine in drug poisoning among the elderly [5].
Side Effects of Bromazepam
According to its manufacturer (Roche Pharmaceuticals), the following adverse effects have been identified with bromazepam usage:
- Allergic directions and anaphylaxis (rare)
- Anterograde amnesia
- Anxiety
- Ataxia
- Blurred vision
- Cardiac failure, including cardiac arrest, hypotension, palpitations, and tachycardia
- Decreased alertness
- Decreased hemoglobin and hematocrit, increased and decreased WBC
- Depression
- Diplopia
- Dizziness
- Drowsiness
- Elevations of alkaline phosphatase, bilirubin, SGOT, and SGPT
- Emotional and mood disturbances
- Falling
- Fatigue
- Incontinence
- Increased and decreased blood sugar levels
- Muscle weakness and muscle spasms
- Pruritus
- Seizures
Roche states that adverse effects are more common when starting bromazepam treatment and usually disappear with repeated administration.
Benzodiazepine Withdrawal & Dependence
Benzodiazepine dependence and withdrawal are very serious matters. Doctors consider benzodiazepines, alcohol, and opioids as having the most dangerous withdrawal symptoms; in rare cases, they can even be deadly.
The schedule IV classification of benzodiazepines really doesn’t portray how dangerous they can be in this regard. Multiple studies show how benzodiazepine dependence and withdrawal symptoms tend to develop in a significant proportion of users who have a prescription. In one study, one-third of individuals who used benzodiazepines for longer than four weeks became physically dependent after concluding treatment [6].
Since the immediate cessation of benzodiazepines can be quite dangerous, users who develop withdrawal symptoms must engage in a slow drug-tapering process to safely get off the drug. This process can take as long as 24 weeks, and complications can always develop, even though it is generally safe.
Harm Reduction: Bromazepam
Here is some important information that users must know if they want to stay safe when using benzodiazepines, either recreationally or via prescription.
Guidelines For the Responsible Use of Benzodiazepines:
- Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- Take frequent breaks — Benzodiazepines can form dependence quickly, so it’s important to stop using them periodically.
- Know the dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- Know who should NOT use benzos for any reason — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Look up “addiction hotline” for more information where you live. (USA: 1-800-662-4357;
General Considerations
When it comes to taking potent prescription drugs like benzodiazepines, users should always be aware of the general harm reduction measures they must implement to stay safe. The most common-sense considerations are also the most important to follow.
Firstly, avoid taking benzodiazepines for recreational purposes and only engage in benzodiazepine use following a legitimate prescription in their name. It’s imperative to follow the dosage recommendations outlined by the doctor and not take prescribed benzodiazepine for reasons other than its intended purpose.
Doctors are aware of benzodiazepine risks and try to prescribe them for the shortest time possible. In terms of time and quantity, the more a drug is consumed, the more likely it is that dependence will develop.
Users should think long and hard about seeking out a benzodiazepine prescription. Even when following the instructions in their prescription, there is still a considerable chance they will still have to endure dependence and withdrawal symptoms.

Bromazepam Drug Interactions
Make sure to be aware of the following drug interactions when using bromazepam.
Depressant Drugs
Prescription drugs like benzodiazepines usually have many harmful interactions to be aware of. Recent drug overdose trends suggest a particularly dangerous combination that all benzodiazepine users must steadfastly avoid — concomitant use of alcohol or opioids.
Benzodiazepines don’t work on the body’s opioid receptors, but they still exert a depressive effect on the body’s CNS. Opioids produce a similar effect, and when both drugs act upon the body simultaneously, the risk of a potentially life-threatening event rises exponentially. The same goes for alcohol.
Additionally, there are always certain esoteric drug combinations that pharmacological research has identified as dangerous. Disclose all the drugs you’re taking to your doctor so they can be aware of this and protect you accordingly.
CYP Drug Interactions
Users must also consider possible CYP drug interactions.
CYP enzymes are responsible for breaking down and metabolizing most pharmacological prescription drugs. As a result, inhibition or induction of these enzymes can affect how a prescription drug functions in the body.
If a drug is a CYP competitor — or inhibits the CYP enzyme responsible for clearing bromazepam — metabolization is less efficient, leading to higher levels of the drug within the body and a greater chance for adverse effects. The reverse is true when drugs induce or encourage the function of that CYP enzyme. In this case, bromazepam would be cleared from the body more efficiently and, in turn, become less effective.
Contraindications of Bromazepam
Contraindications are also important to be aware of. They are avoidable since doctors are cognizant of them and prescribe drugs in a way that avoids them; it’s different for the large proportion of users who misuse benzodiazepines.
Typical contraindications include things like hepatic impairment, pregnancy, very old or very young age groups, driving, heavy machinery use, etc. Different drugs have different contraindications, so users should take the time to research the specifics geared towards their prescription medication.
Roche has identified the following contraindications for bromazepam:
- Concomitant use of alcohol and other CNS depressants
- Driving or operating heavy machinery
- Medical history of drug abuse
- Myasthenia gravis
- Narrow-angle glaucoma
- Nursing women
- Patients less than 18 years of age
- Pregnant women
- Sensitivity to benzodiazepines
- Severe hepatic impairment
- Severe respiratory insufficiency
- Sleep apnea syndrome
Proper Bromazepam Dosage
Taking bromazepam in its proper dosage is one of the best things you can do to stay safe.
For adults, the recommended initial dosage is 6 to 18 mg in equally divided doses, depending on the severity of symptoms and response of the patient. Treatment should be initiated at lower doses and adjusted as necessary. The optimal dosage may range from 6 to 30 mg daily in divided doses.
With elderly and debilitated patients, the initial daily dose should not exceed 3 mg in divided doses. This dosage can be carefully adjusted depending on the patient’s tolerance and response.
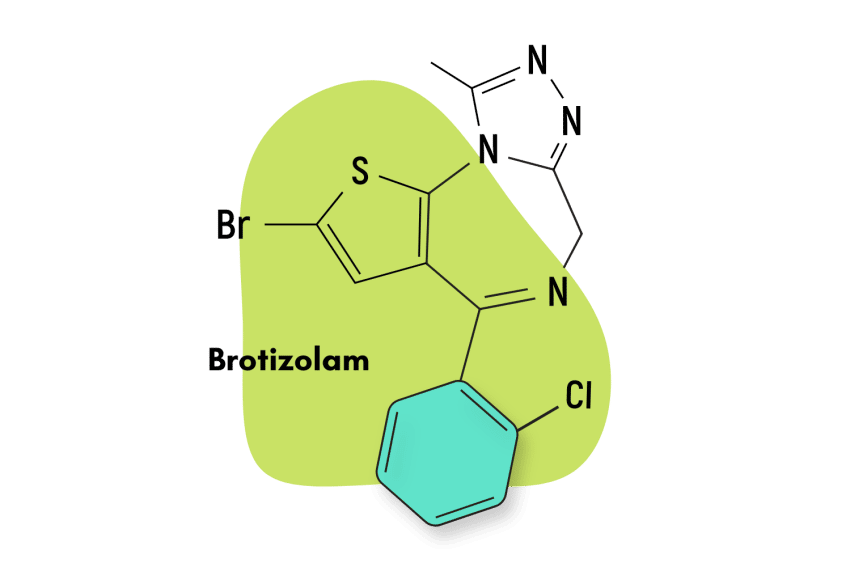
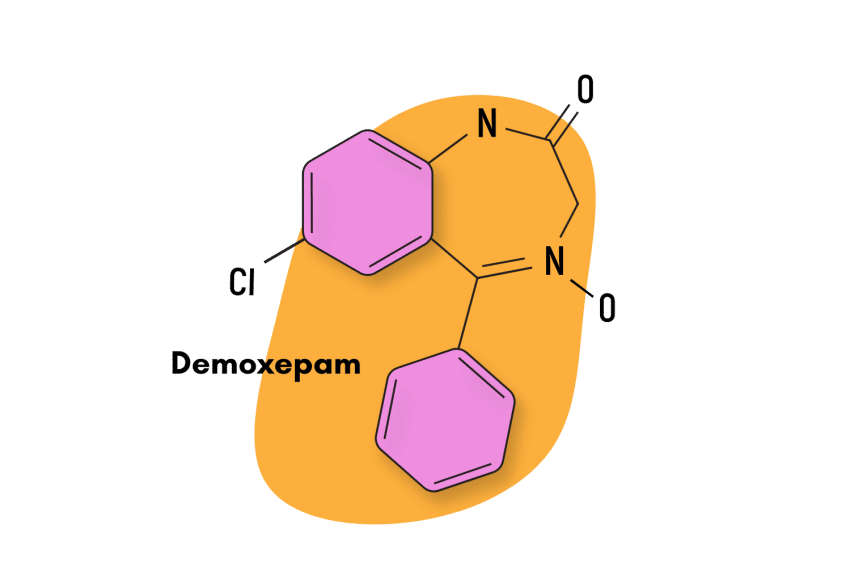
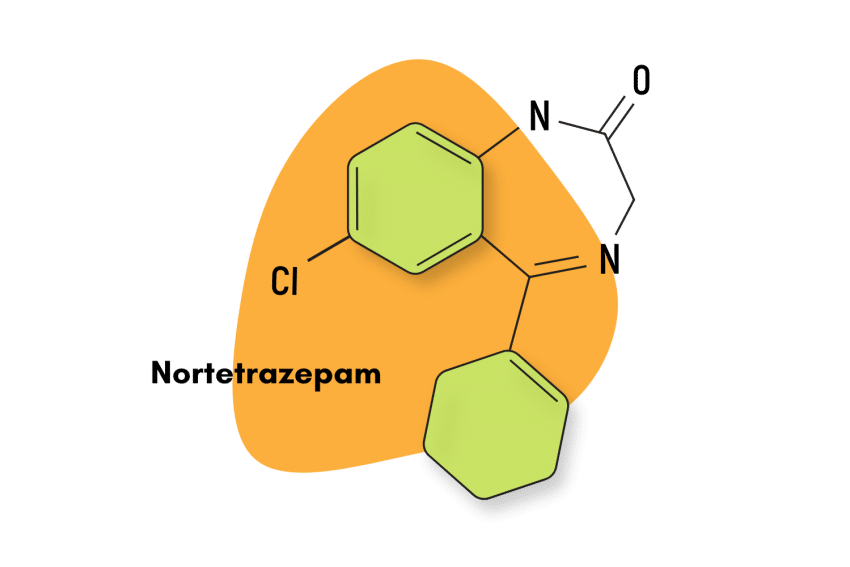
Similar Benzodiazepines
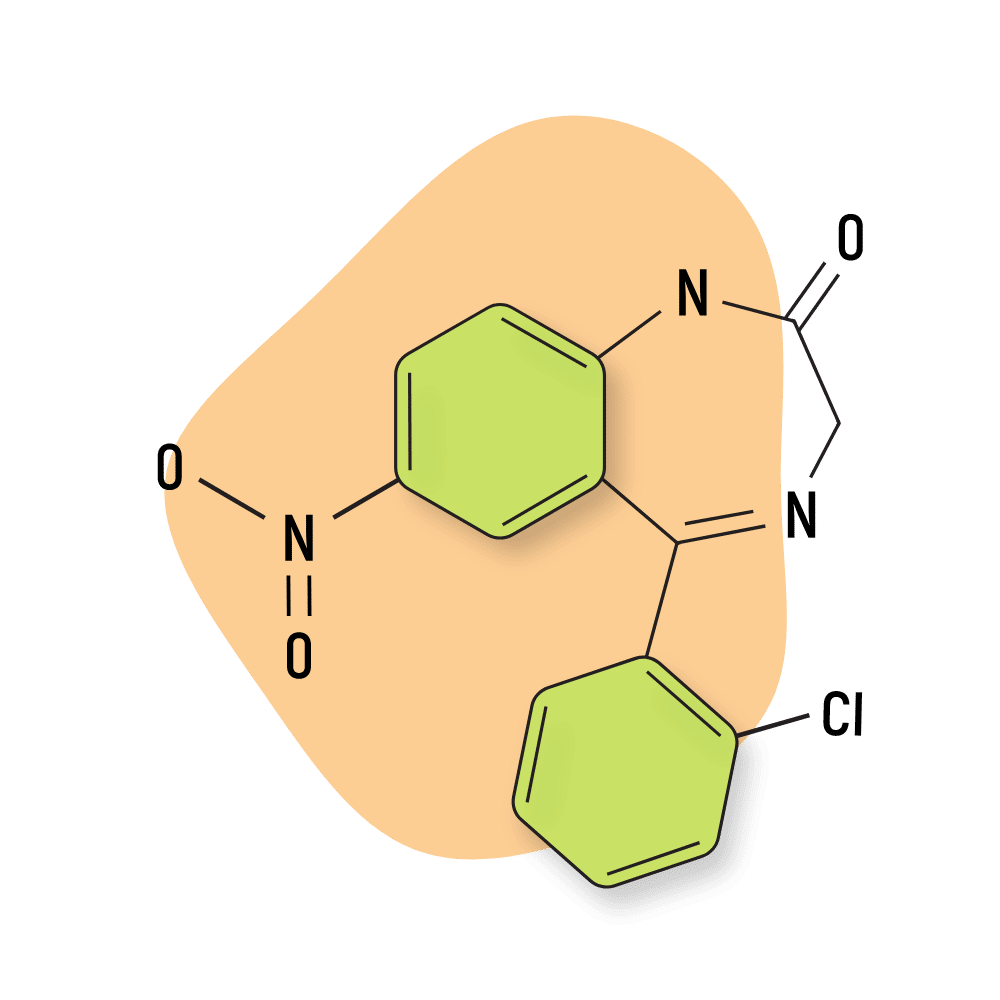
Bromazepam is classified as an intermediate-acting 1,4-benzodiazepine, which makes it most similar to drugs like clonazepam (Klonopin) and fludiazepam (Erispan).
Chlordiazepoxide (Librium)
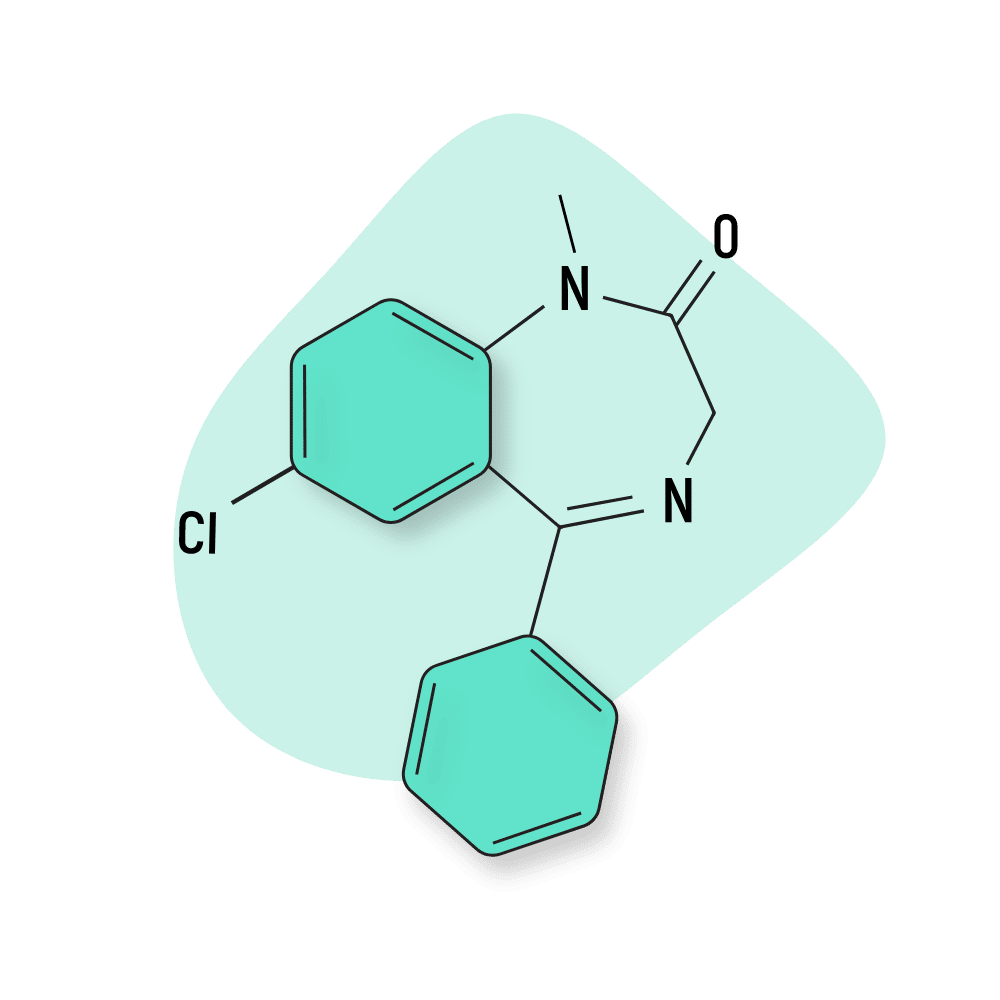
Chlordiazepoxide is one of the oldest benzodiazepines ever brought to market, and it remains one of the most popular today. It’s known for it’s exceptionally long-lasting effects. Chlordiazepoxide is slowly metabolized into nordiazepam, which has an even longer duration of effects. The total duration of effects of chlordiazepoxide is between 24 and 36 hours long.
This compound isn’t as popular as bromazepam among recreational users because it doesn’t offer nearly as powerful inebriating effects as the former.
Fludiazepam (Erispan)
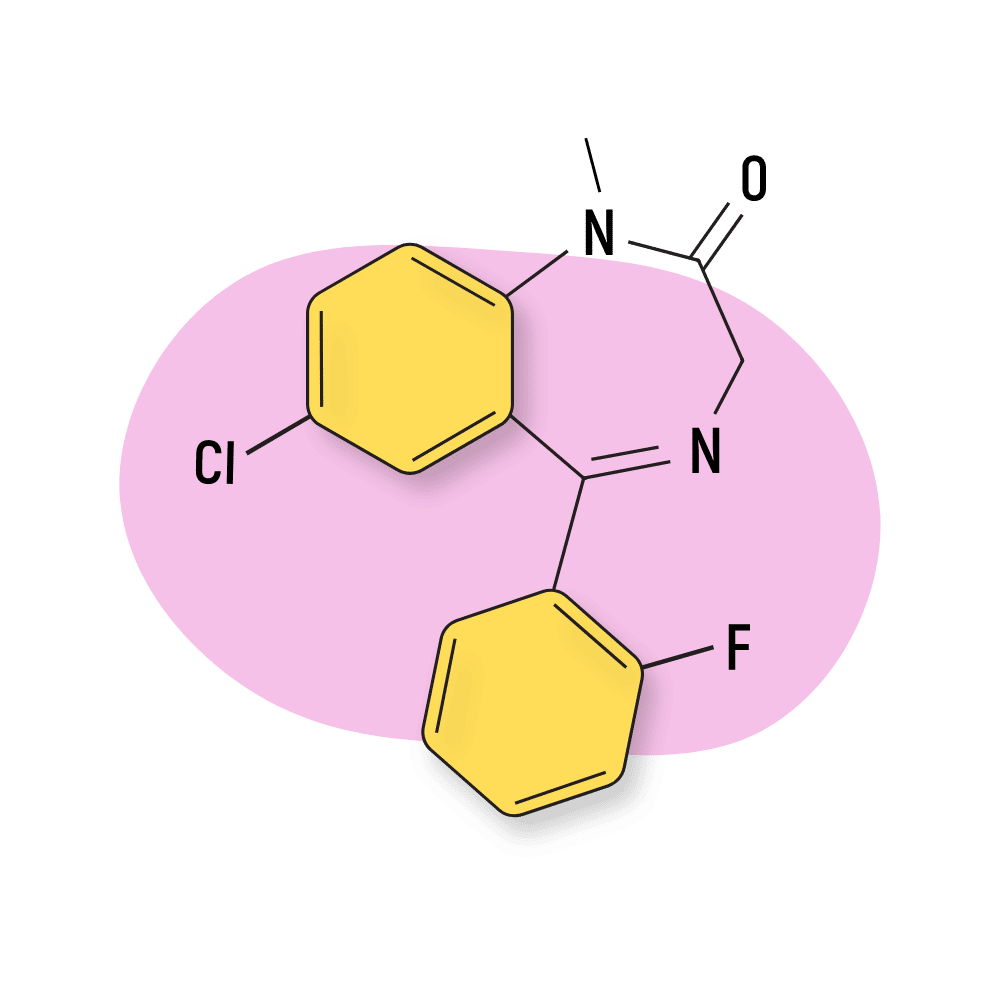
Fludiazepam is an isomer of diazepam (Valium) with roughly 4X the strength (unconfirmed). This compound was invented in Japan in the 60s but never brought to market. It’s seen a dramatic uptick in popularity in recent years in the designer drug community for its inebriating and euphoric action.
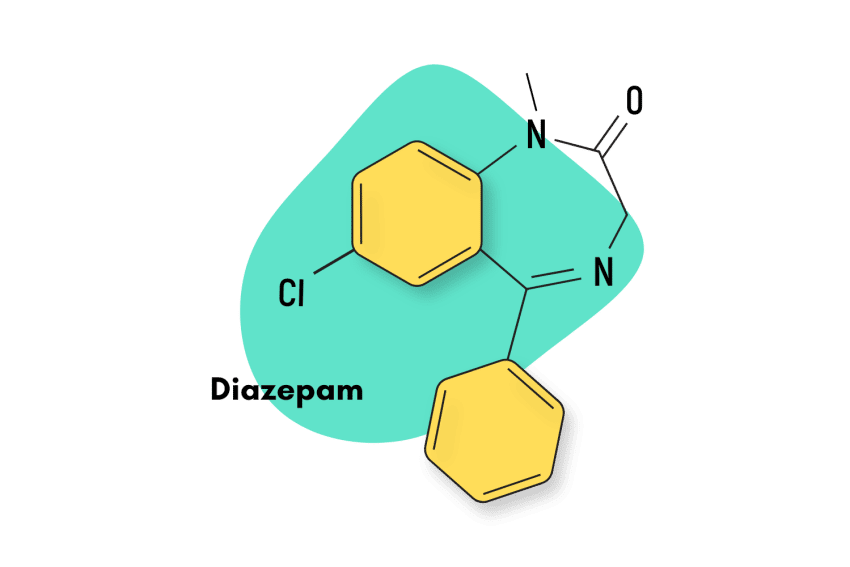
Diazepam (Valium)
Bromazepam’s side effects profile has been frequently compared to that of diazepam. They are also of the same benzodiazepine subtype and exert their effects through the same mechanism of action. However, they are quite different in other regards. Bromazepam has a much shorter half-life and is considered to be around 3x as potent.
Clonazepam (Klonopin)
Clonazepam, like bromazepam, is another high-potency benzodiazepine. Because of this, both are indicated for the treatment of panic disorders. They also have fairly similar half-lives, with clonazepam taking slightly longer to eliminate.
Natural Alternatives to Benzodiazepines
A number of effective plant-based alternatives have started to gain popularity in recent years.
The kava plant is one of these herbal options. Research shows this plant has certain alkaloids that can induce both anxiolytic and sedative effects on users — with minimal adverse side effects compared to pharmacological drugs like benzodiazepines [7]. Recognition for plant-based options is slow, but recently the WHO came out in favor of the kava plant as an alternative treatment option.
Users could also go with the kratom plant. Since it acts on the body’s opioid receptors, this plant has a slightly more risky profile than the kava plant. However, when taken by itself in responsible doses, it is an incredibly safe compound. Research shows the kratom plant has a stunning range of pharmacological properties. It can produce stimulating and euphoric effects in lower doses and anxiolytic and sedating properties with larger amounts [8].
References
- Poisbeau, P., Gazzo, G., & Calvel, L. (2018). Anxiolytics targeting GABAA receptors: Insights on etifoxine. The World Journal of Biological Psychiatry, 19(sup1), S36-S45.
- Sieghart, W., & Sperk, G. (2002). Subunit composition, distribution and function of GABA-A receptor subtypes. Current topics in medicinal chemistry, 2(8), 795-816.
- Masiulis, S., Desai, R., Uchański, T., Serna Martin, I., Laverty, D., Karia, D., … & Aricescu, A. R. (2019). GABAA receptor signaling mechanisms revealed by structural pharmacology. Nature, 565(7740), 454-459.
- Lakhal, K., Pallancher, S., Mathieu-Daude, J. C., Harry, P., & Capdevila, X. (2010). Protracted deep coma after bromazepam poisoning. International journal of clinical pharmacology and therapeutics, 48(1), 79.
- Perković-Vukčević, N., Vuković-Ercegović, G., Šegrt, Z., Đorđević, S., & Jović-Stošić, J. (2016). Benzodiazepine poisoning in elderly. Vojnosanitetski pregled, 73(3), 234-238.
- Riss, J., Cloyd, J., Gates, J., & Collins, S. (2008). Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta neurologica scandinavica, 118(2), 69-86.
- Cairney, S., Clough, A. R., Maruff, P., Collie, A., Currie, B. J., & Currie, J. (2003). Saccade and cognitive function in chronic kava users. Neuropsychopharmacology, 28(2), 389-396.
- Swogger, M. T., & Walsh, Z. (2018). Kratom use and mental health: A systematic review. Drug and Alcohol Dependence, 183, 134-140.
- van Harten, J. (1995). Overview of the pharmacokinetics of fluvoxamine. Clinical pharmacokinetics, 29(1), 1-9.