Delorazepam (Dadumir) Fact Sheet & Harm Reduction Guide
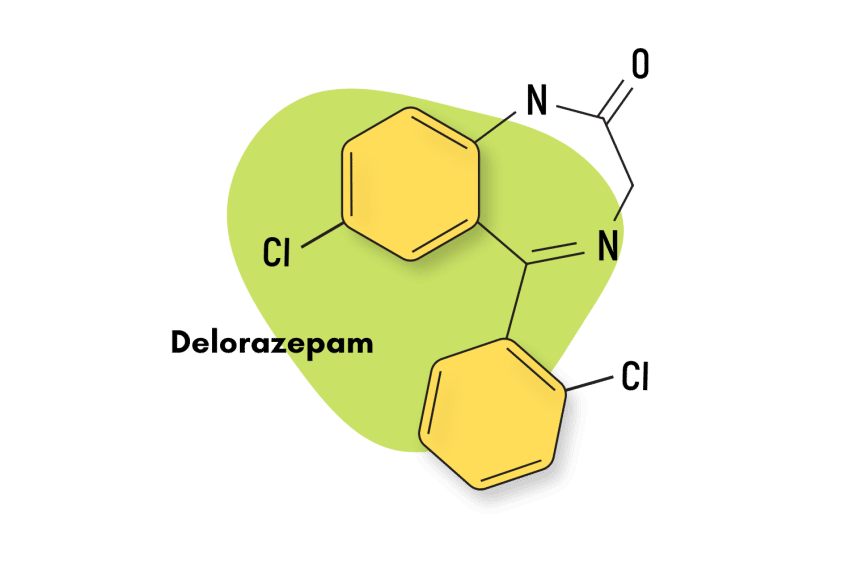
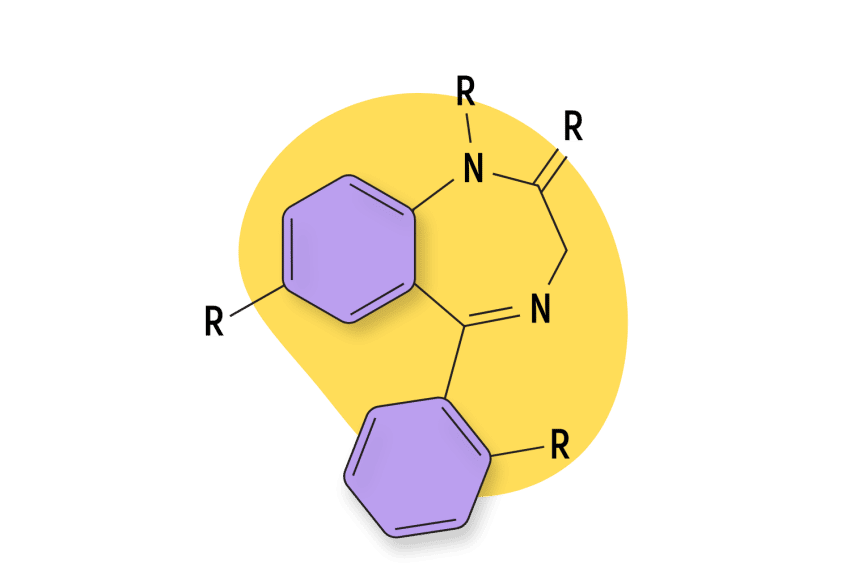
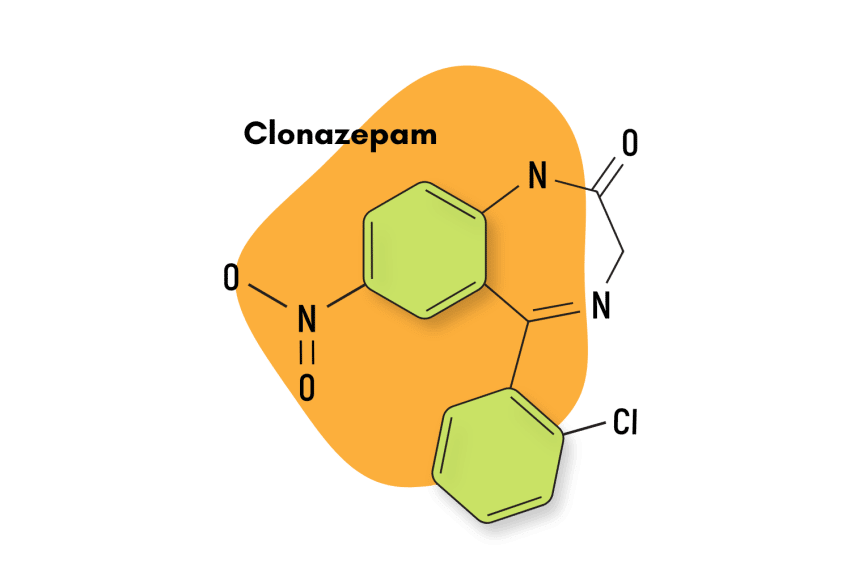
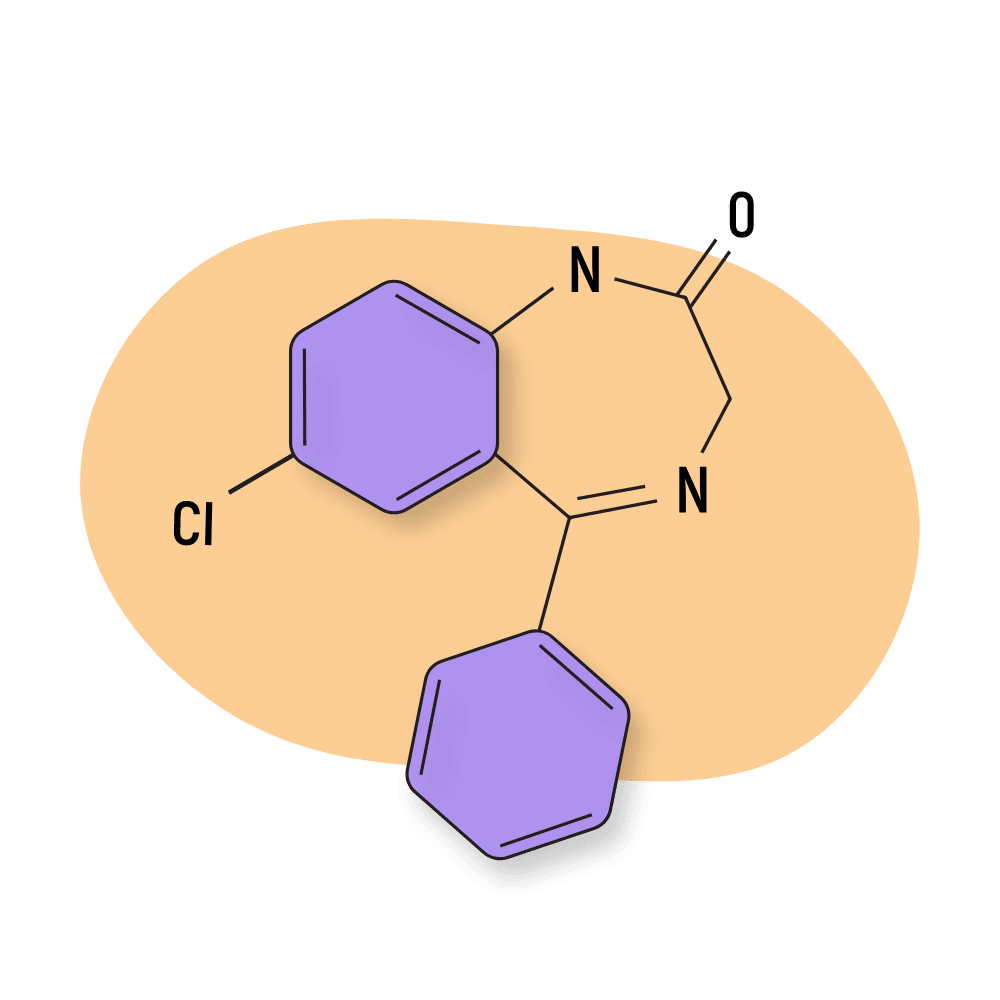
An analog to nordiazepam, delorazepam — also known as EN and Dadumir — is a traditional 1,4-benzodiazepine compound sold in Italy for treating anxiety and insomnia. It’s actually one of the few benzodiazepines that occur in nature.
That’s right; delorazepam can be extracted from three separate plant species: Solanum tuberosum (a type of potato), Triticum aestivum (common wheat), and Artemisia dracunculus (tarragon).
In terms of its individual properties, delorazepam is quite potent, being roughly ten times as strong as diazepam, and is known to be a long-lasting compound, a characteristic feature of the 1,4-benzodiazepine subclass.
Delorazepam Specs
IUPAC Name: 7-chloro-5-(2-chlorophenyl)-1,3-dihydro-1,4-benzodiazepin-2-one
Other Names: EN, Dadumir
Metabolism: Delorazepam is metabolized at a relatively slow pace by the liver. The major metabolite (15-34% of the parent drug) is lorazepam. Older patients metabolize delorazepam slower than younger patients.
Duration of Effects: Delorazepam has a long elimination half-life, roughly around 60-140 hours. This value can be vastly extended in those with liver disease.
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does Delorazepam Work?
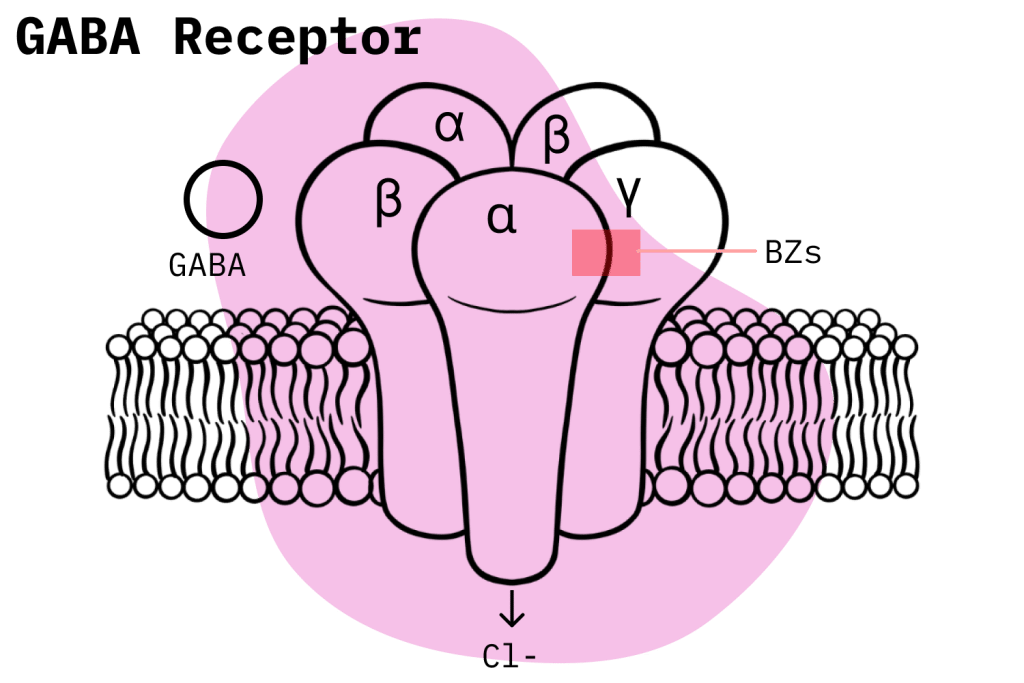
As is the norm for 1,4- benzodiazepines, delorazepam exerts its effects through the classical GABA-mediated pathway. This means that benzodiazepine receptors bind to specific GABA-A subunits and produce what is known as an “allosteric effect,” which then, in turn, enhances the natural inhibitory function of GABA receptors to produce a generalized depressive effect on the brain and central nervous system (CNS).
This depressive effect is the proximate cause for the pharmacological profile of benzodiazepines, and it’s what gives delorazepam its anxiolytic, muscle relaxant, hypnotic and anticonvulsant properties.
Given the fact that most benzodiazepines have this standard mechanism of action, what sets them apart from each other, pharmacologically speaking, mostly comes down to individual characteristics in regards to things like their specific affinity for the different GABA-A subunits, pharmacokinetic qualities such as bioavailability and elimination half-life, and the presence of secondary mechanisms of action [1].
In this sense, it’s quite important to try and understand how these characteristics factor into the pharmacological profile of a given benzodiazepine.
For instance, we know that delorazepam’s long elimination half-life is an important reason for its clinical success as an anxiolytic [2]. Additionally, delorazepam demonstrates a fast absorption rate, reaching peak plasma levels within 1-2 hours.
Another critical factor is the fact that delorazepam produces pharmacologically active metabolites, with its most significant byproduct being the popular benzodiazepine lorazepam, which represents about 15-24 percent of the parent drug (delorazepam) [3]. Also, delorazepam is itself a metabolic byproduct of diclazepam and cloxazolam.
Is Delorazepam Safe? Risks & Side Effects
The FDA has not approved delorazepam, but it does have a Schedule IV designation under the Controlled Substances Act. This implies that United States authorities do consider the compound to have legitimate medical uses but also recognize that it carries with it the potential for misuse and physical dependence. The vast majority of benzodiazepines also share in this classification.
When used correctly, benzodiazepines are reasonably safe, but the possibility of misuse always has to be factored into the equation. If a benzodiazepine is misused, the risk level rises considerably. For example, the vast increase in benzodiazepine and opioid-related deaths in the United States result from misuse due to an explosion in polydrug abuse. As such, users should always stick carefully to the instructions given out with their prescriptions.
In the case of delorazepam, we know that benzodiazepines that exhibit a long elimination half-life have less of a possibility of causing physical dependence and/or misuse. This is because compounds with short elimination half-lives can sometimes induce inter-dose withdrawal symptoms and, in general, have an increased potential for inducing habits that lead to misuse [4].
However, we know that due to its slow metabolism, delorazepam tends to accumulate inside the body, which raises the risk of adverse effects. This accumulative effect is much more pronounced in elderly patients, and side effects also tend to be more pronounced in the higher age groups [3].
Side Effects of Delorazepam
According to Italian authorities, delorazepam’s side effects, if they occur, are usually seen at the start of treatment and generally decrease in intensity or disappear as therapy progresses or the dosage is reduced.
The side effects listed for delorazepam may include the following:
- Ataxia
- Confusion
- Decreased alertness
- Drowsiness
- Dulling of emotions
- Sedation
- Tachycardia
Rarer side effects of delorazepam may include:
- Agranulocytosis
- Alopecia
- Blood alkaline phosphatase increases
- Blood bilirubin increases
- Blurred vision
- Diplopia
- Disinhibition
- Euphoric mood,
- Extrapyramidal disorders (including tremors, dizziness, headache, dysarthria/speech difficulties, amnesia, and coma)
- Hypotension
- Incontinence
- Jaundice
- Pancytopenia
- Rashes
- SIADH (syndrome of inappropriate antidiuretic hormone secretion)
- Suicidal ideation / suicide attempts
- Thrombocytopenia
- Transaminases increases
Benzodiazepine Withdrawal & Dependence
Benzodiazepines withdrawals are not an uncommon occurrence among those who use benzodiazepines. The Schedule IV designation of most benzodiazepines leads many to believe that if they avoid misuse, they will not likely become physically dependent. Unfortunately, this is a common misconception.
The potential for benzodiazepines to cause physical dependence is extremely prominent, even if there is no misuse on the part of the patient. In fact, the standard medical practice when prescribing benzodiazepines is to try and limit them for the shortest time frame possible without significantly affecting the treatment’s probability of success.
Studies have attempted to look at this problem to contextualize the potential for benzodiazepines to cause a physical. One study examined the likelihood of developing dependence in patients who took benzodiazepines for longer than four weeks and found that one-third of participants developed dependence and consequent withdrawal symptoms after completing treatment [5].
Developing a benzodiazepine dependence implies that, to get off them safely, users must go through a long and drawn-out procedure known as drug tapering. Basically, drug tapering implies that over four to 16 weeks, depending on the severity of the dependence, users slowly reduce the amount of benzodiazepines consumed until they can finally cease taking them.
Benzodiazepine withdrawals are a very serious matter, and users should seriously weigh the risks of exposing themselves to dependence before they begin a benzodiazepine treatment. Along with alcohol, only benzodiazepine withdrawals have the potential to turn deadly if left untreated. However, this is a rare occurrence.
Harm Reduction: Delorazepam
One of the goals of this article is for benzodiazepines users —and that includes recreational users —to have more conceptual tools that allow them to make safer choices when using benzodiazepines. With this goal in mind, the following section will go over some general rules that, although common sense, are the most effective at reducing risk and harm.
Firstly, potential benzodiazepine users should always ask themselves if a benzodiazepine treatment is even necessary in the first place. For those looking for anxiolytic relief, for example, there are a vast number of behavior-related solutions like exercise or therapy that often have great results. They could also combine their efforts with natural, plant-based medications like kratom or kava.
Too often, users will start taking a dangerous prescription drug without even attempting other alternatives beforehand.
Users should also be honest with themselves about their ability to correctly handle a benzodiazepine prescription. The single most significant risk factor when taking benzodiazepines is misuse, and if someone is likely to abuse their prescription, then they shouldn’t have it in the first place. For example, it is known that patients with a history of drug or alcohol abuse are more likely to misuse a prescription drug.
Another important rule of thumb, once a patient is already on benzodiazepines, is to try their hardest to limit the drug’s quantity —preferably to the lowest effective dose possible —and the duration of treatment. Reducing both these factors is the most effective strategy to hedge against the risk of physical dependence. Remember: the more a drug is consumed and the longer its consumed, the larger the chance a physical dependence will form.
Regarding recreational users, there are also a couple of simple rules that will allow them to reduce their risk. However, it should be considered that recreational use is inherently dangerous, and we do not condone it.
Mainly, recreational users should try their hardest to resist the temptation to combine benzodiazepines with other drugs, as this will raise their risk levels substantially. They should also try to procure flumazenil and learn how to use it; harm reduction organizations are usually the best resource for this. Flumazenil is a benzodiazepine antagonist and can work to revert the effects of benzodiazepine-related overdoses.
Benzodiazepine Harm Reduction Tips:
- 🥣 Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- ⏳ Take frequent breaks or plan for a short treatment span — Benzodiazepines can form dependence quickly, so it’s important to stop using the drug periodically.
- 🥄 Always stick the proper dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- 💊 Be aware of contraindications — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- 🧪 Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- 💉 Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- 🌧 Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- ⚖️ Understand the laws where you live — In most parts of the world, benzodiazepines are only considered legal if given a prescription by a medical doctor.
- 📞 Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Look up “addiction hotline” for more information where you live. (USA: 1-800-662-4357; Canada: 1-866-585-0445; UK: 0300-999-1212).
Delorazepam Drug Interactions
Never use benzodiazpines and other CNS depressants in a concomitant fashion. These interactions put users at risk of respiratory depression, which is the leading cause of death among drug overdoses. However, when it comes to prescription drugs, any type of combination that has not been pre-approved by a doctor should be avoided.
Delorazepam Contraindications
According to Italian authorities, the following contraindications are listed for delorazepam:
- Acute intoxication with alcohol, hypnotics, analgesics, or psychotropic drugs
- Hypersensitivity to benzodiazepines
- Myasthenia gravis
- Narrow-angle glaucoma
- Pregnancy and lactation
- Severe liver failure
- Severe respiratory failure
- Sleep apnea syndrome
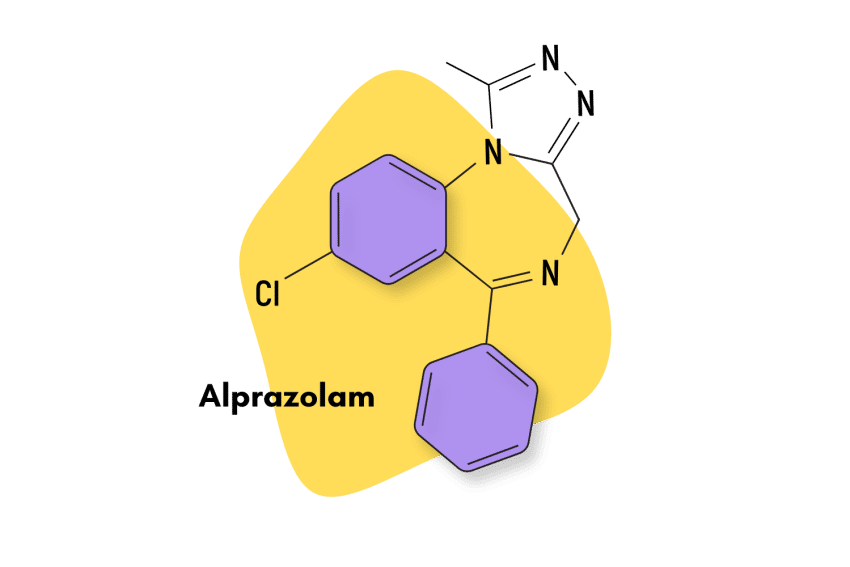
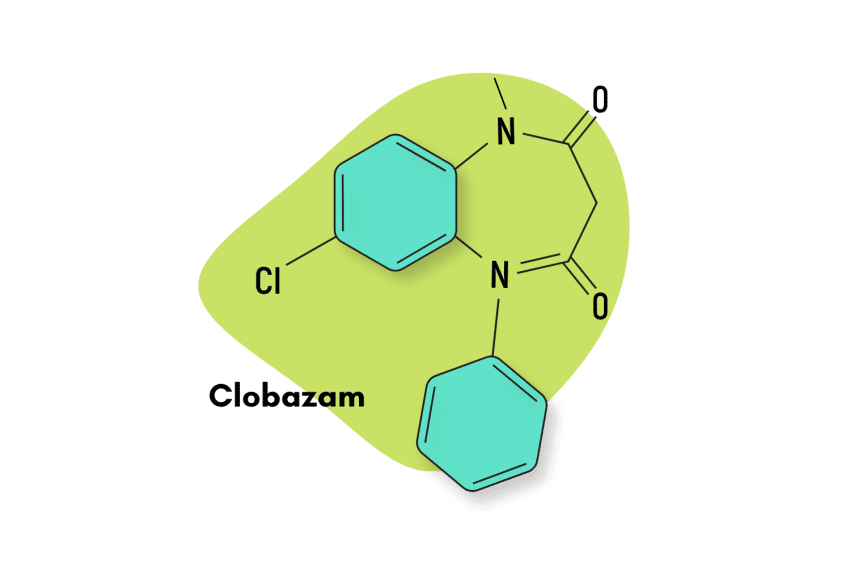
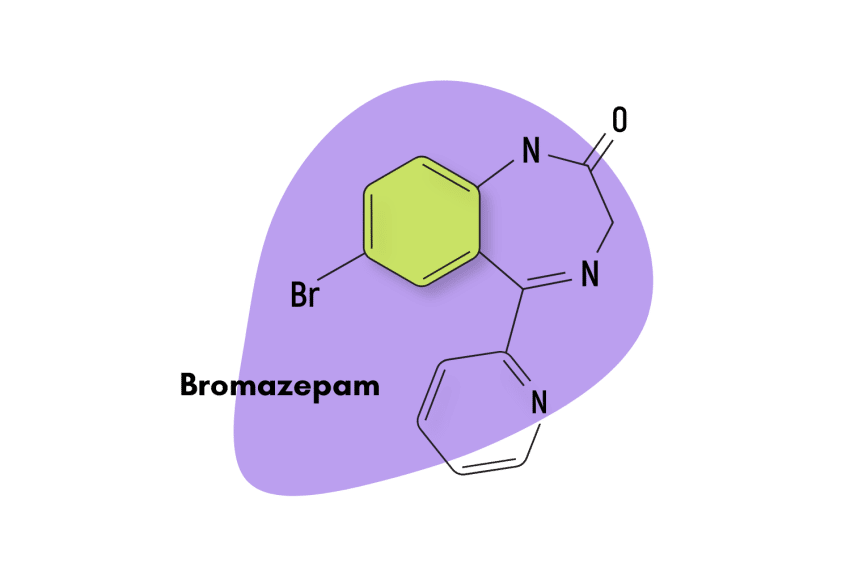
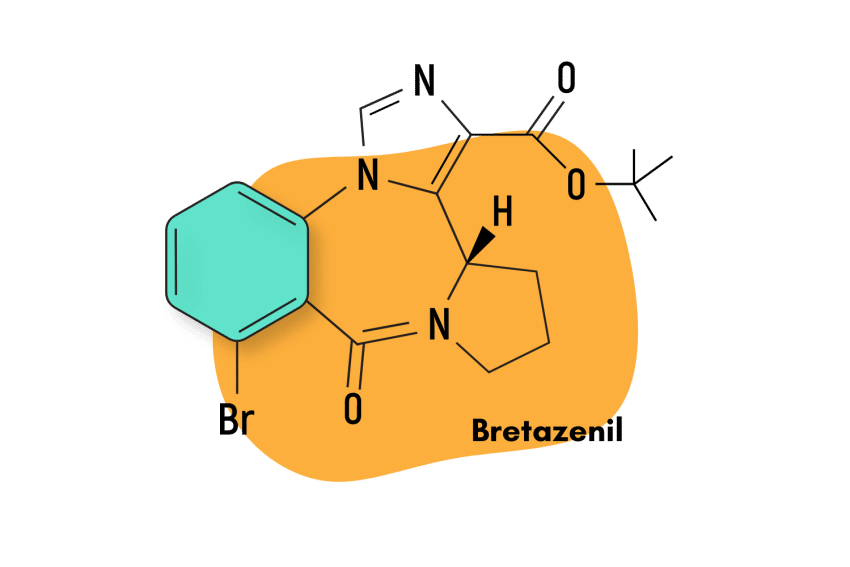
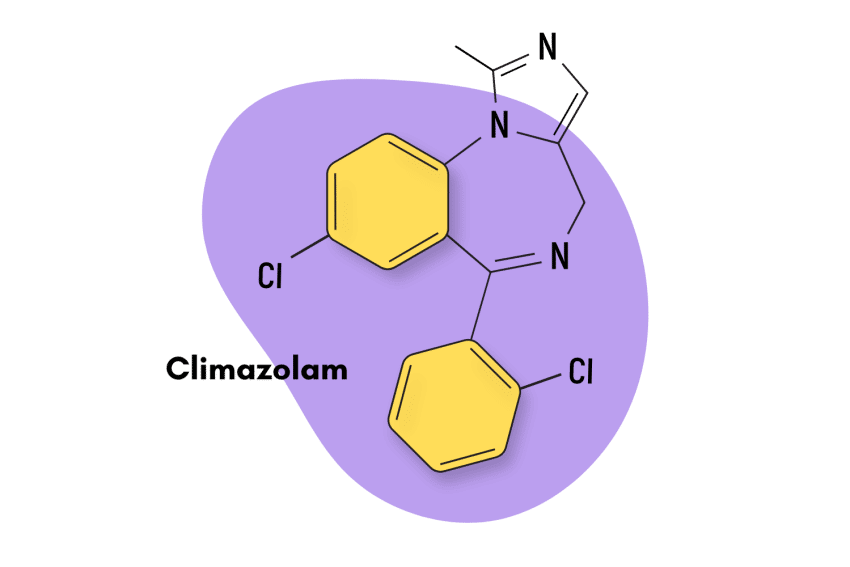
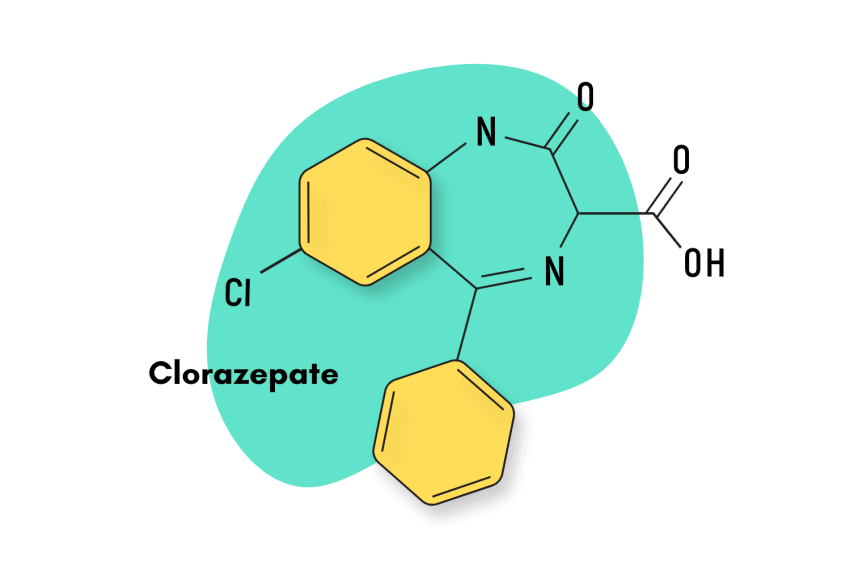
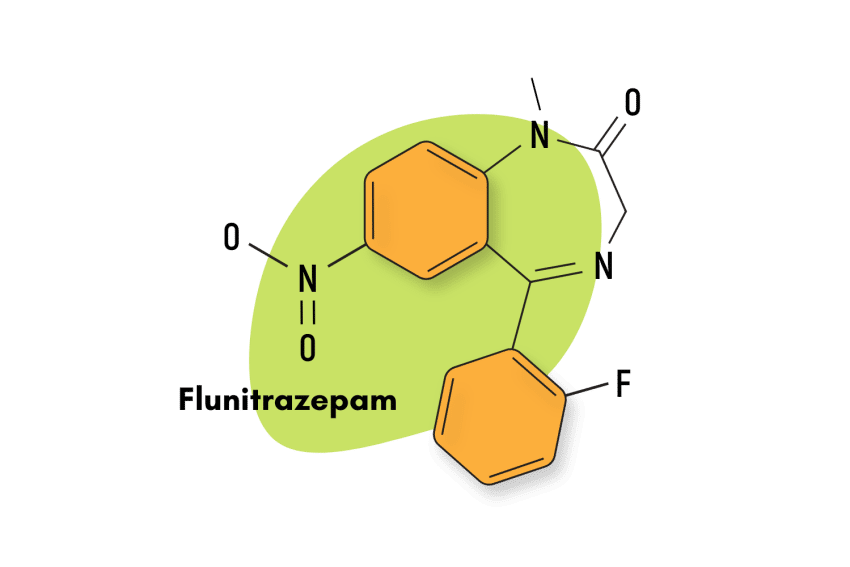
Similar Benzodiazepines
For those interested in similar benzodiazepine compounds, delorazepam has comparable characteristics to many benzodiazepines.
Nordazepam
Delorazepam is an analog compound to nordazepam, so it makes sense that they have comparable structural and pharmacological properties. Both benzodiazepines enjoy a long duration of effects and have the unique characteristic of being naturally occurring in nature.
Mexazolam
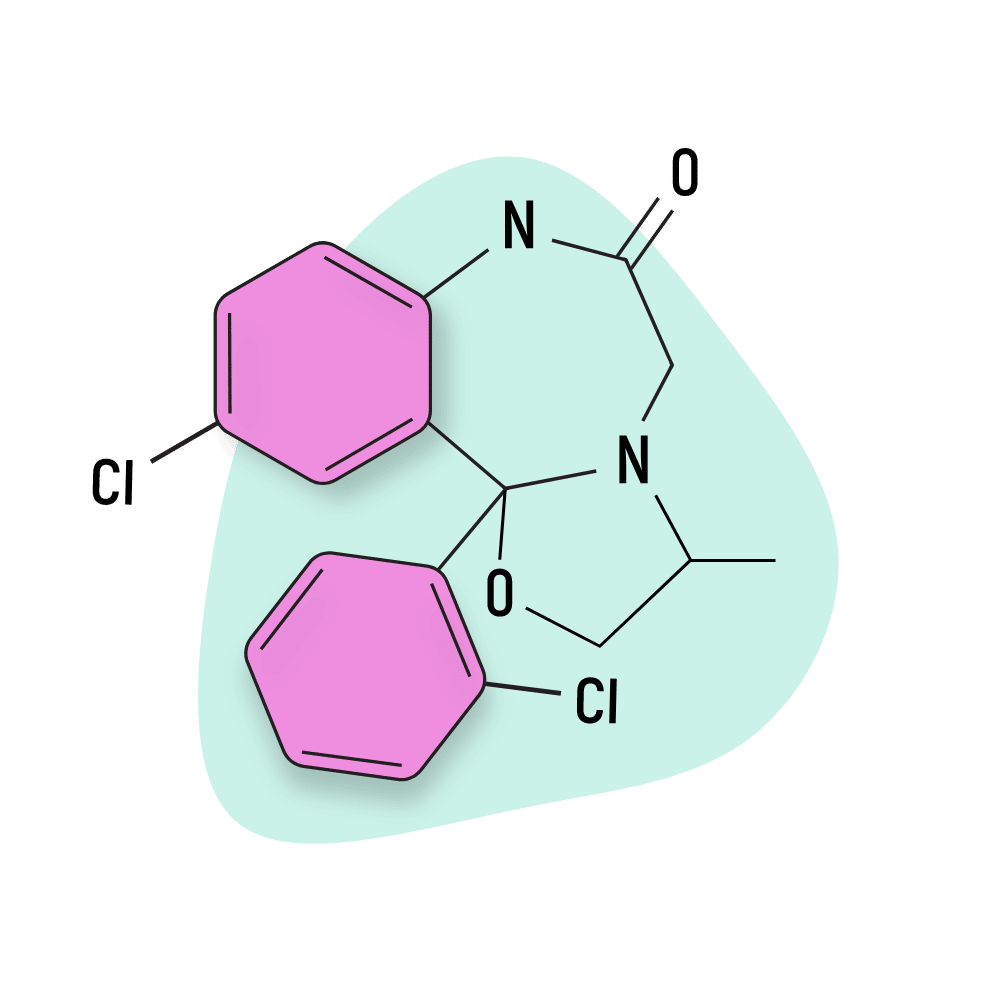
Mexazolam is an approved medication in Portugal, but even so, it is a rare benzodiazepine, and not much is known about it. However, we do know that mexazolam produces delorazepam as one of its two metabolic byproducts. They share comparable pharmacological characteristics like a long-lasting duration of effects and a high potency.
Alternatives to Benzodiazepines
As stated before, many natural alternatives are now available for users who do not wish to expose themselves to the risks associated with pharmacological drugs like benzodiazepines. However, it should be noted that, in general, natural options are not as potent as pharmacological ones.
L-Theanine
L-Theanine, one of the active ingredients in green and black tea, can help users achieve similar anxiolytic and sedative benefits to those found in benzodiazepines. L-Theanine accomplishes these through two primary means.
L-Theanine can work to reduce the effects of glutamate, the brain’s chief excitatory neurotransmitter. In essence, glutamate is the counterpart to GABA. L-Theanine can reduce glutamate’s effects by binding, rather than activating, glutamate receptor sites in the brain [6].
And, like benzodiazepines, L-theanine can also increase GABA activity, although not through an allosteric effect, which leads to feelings of calm and sedation [6].
Kratom
The kratom plant has seen an explosion in popularity due to its wide range of effects and its effectiveness in treating several conditions. One of its most remarkable qualities is that kratom’s properties actually change depending on how much is consumed. At low doses, kratom offers stimulant and euphoric benefits, while at mid-to-high doses, kratom becomes anxiolytic and sedative [7].
However, compared to other natural alternatives, kratom presents a higher risk level. Studies have found that, when consumed in high quantities, kratom can become addictive. Since it is a CNS depressant drug that acts on the body’s opioid receptors, it can become dangerous when mixed with other CNS-depressant compounds like alcohol, benzodiazepines, or opioids.
Delorazepam FAQs
Is delorazepam available in the United States?
No. The FDA has not approved Delorazepam.
What formulations is delorazepam available in
Delorazepam is available in either 0.5 mg, 1 mg, or 2 mg oral tablets and as an oral solution.
What is the bioavailability of delorazepam?
Delorazepam has a high bioavailability of roughly 80%.
What are the indications listed for delorazepam?
According to Italian authorities, delorazepam is indicated for anxiety, tension, and other somatic or psychiatric manifestation associated with anxiety-related disorders and insomnia.
Are there any off-label uses for delorazepam?
Delorazepam has also been known to be used as a treatment for alcohol withdrawal and to relieve anxiety the night before a medical procedure.
References
- Vgontzas, A. N., Kales, A., & Bixler, E. O. (1995). Benzodiazepine side effects: role of pharmacokinetics and pharmacodynamics. Pharmacology, 51(4), 205-223.
- Bertin, I., Colombo, G., Furlanut, M., & Benetello, P. (1989). Double-blind placebo cross-over study of long-acting (chlordesmethyldiazepam) versus short-acting (lorazepam) benzodiazepines in generalized anxiety disorders. International journal of clinical pharmacology research, 9(3), 203-208.
- Bareggi, S. R., Truci, G., Leva, S., Zecca, L., Pirola, R., & Smirne, S. (1988). Pharmacokinetics and bioavailability of intravenous and oral chlordesmethyldiazepam in humans. European journal of clinical pharmacology, 34(1), 109-112.
- Schmitz, A. (2016). Benzodiazepine use, misuse, and abuse: a review. Mental Health Clinician, 6(3), 120-126.
- Riss, J., Cloyd, J., Gates, J., & Collins, S. (2008). Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta neurologica scandinavica, 118(2), 69-86.
- Nathan, P. J., Lu, K., Gray, M., & Oliver, C. (2006). The neuropharmacology of L-theanine (N-ethyl-L-glutamine), a possible neuroprotective and cognitive enhancing agent. Journal of Herbal Pharmacotherapy, 6(2), 21-30.
- Eastlack, S. C., Cornett, E. M., & Kaye, A. D. (2020). Kratom—Pharmacology, clinical implications, and outlook: a comprehensive review. Pain and therapy, 9(1), 55-69.