EVT-201 (Research Benzodiazepine) Fact Sheet & Harm Reduction Guide
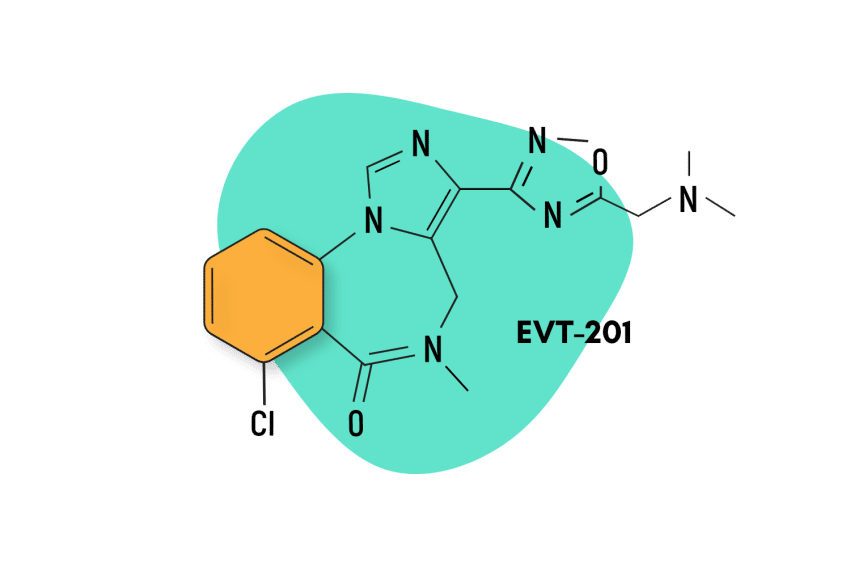
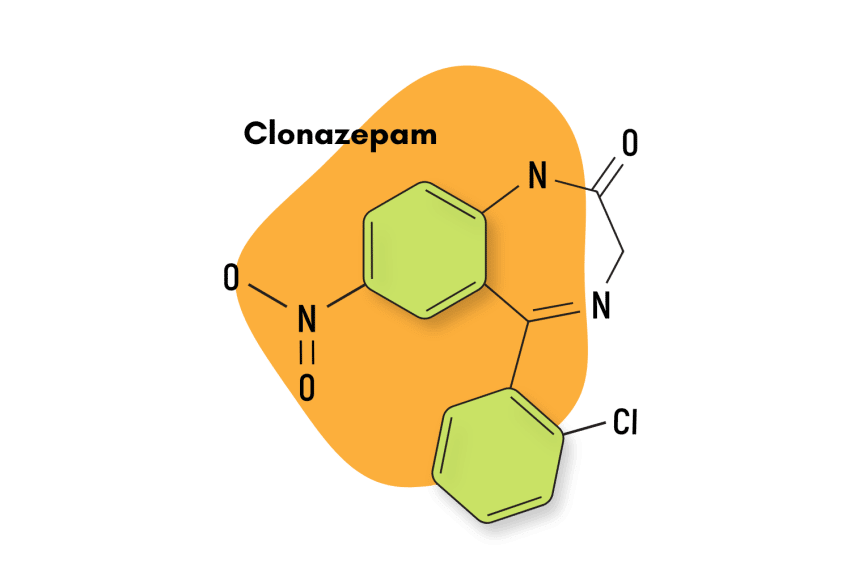
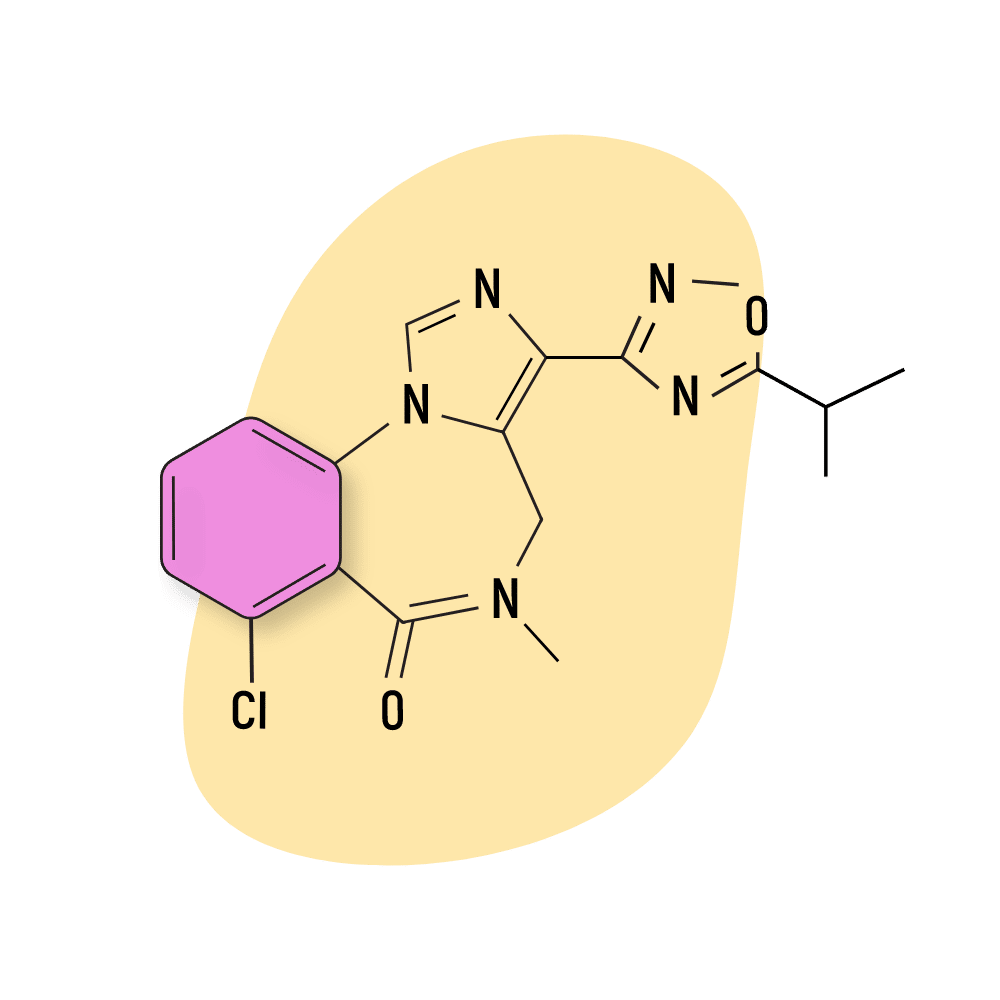
EVT-201 is a benzodiazepine drug belonging to the imidazobenzodiazepine subclass. It was initially developed for use as a non-sedating anxiolytic, but clinical trials revealed the drug had significant hypnotic effects.
At the moment, EVT-201 is undergoing clinical trials to determine its efficacy as a hypnotic medication, as there is evidence to believe it could be a safer option for elderly patients than most other benzodiazepine hypnotics.
This drug is not officially available, but some reports suggest it’s already circulating on the designer drug market.
Here you’ll learn how EVT-201 works, how it compares to other benzodiazepines, how to stay safe while using it, and more.
EVT-201 Specs
| Status | Undergoing phase II clinical testing |
| Common Dosage | Unspecified |
| PubChem ID | 9885841 |
| CAS# | 308239-86-3 |
IUPAC Name
7-chloro-3-[5-[(dimethylamino)methyl]-1,2,4-oxadiazol-3-yl]-5-methyl-4H-imidazo[1,5-a][1,4]benzodiazepin-6-one
Metabolism
The metabolism of EVT201 is mediated by tyrosine monoxides and cytochrome CYP2D6 to produce several metabolites, including Ro46-1927 and Ro18-5528 [2]. More research is still needed to determine the exact metabolic pathway of EVT-201.
Duration of Effects
The elimination half-life of EVT201 ranged from three to four hours [2].
Benzodiazepine Dosage Equivalency Calculator
**Caution:** Benzodiazepines have a narrow therapeutic window. Dose equivalents may not be accurate in higher doses.
This calculator does not substitute for clinical experience and is meant to serve only as a reference for determining oral benzodiazepine equivalence.
Please consult a medical practitioner before taking benzodiazepines.
How Does EVT-201 Work?
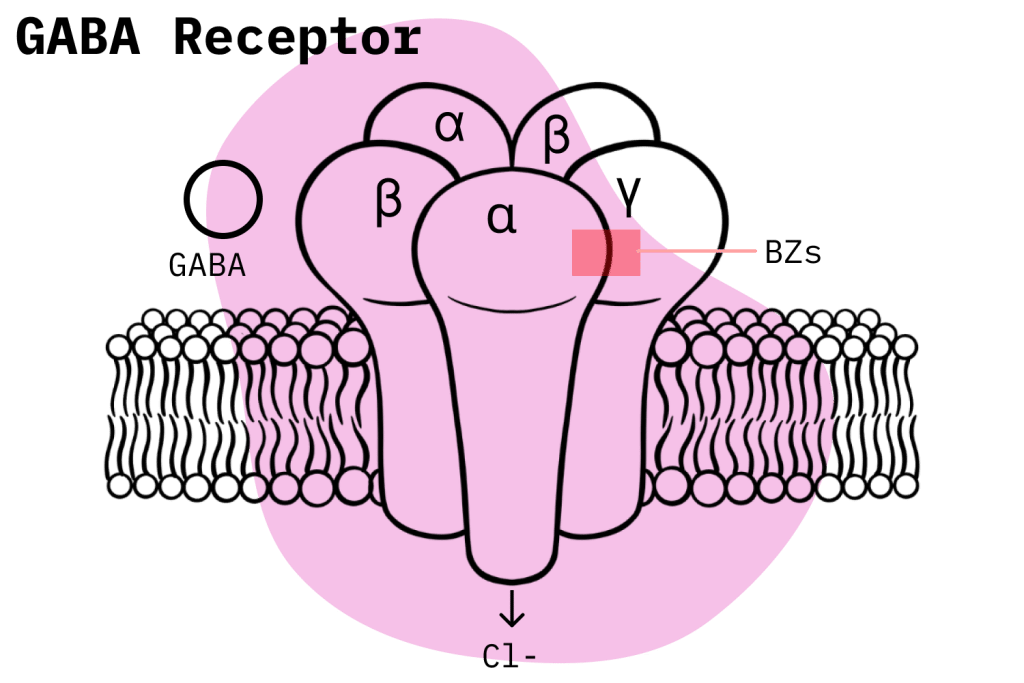
EVT-201’s pharmacology is mediated by the standard GABA-mediated pathway used by most benzodiazepines. Benzodiazepine molecules bind to GABA receptor sites and exert an allosteric effect to potentiate the naturally inhibitory properties of GABA and produce the traditional range of effects associated with benzodiazepines.
However, there are still meaningful differences in how benzodiazepines utilize this pathway, and these particular qualities have a significant role in mediating their effects profile.
In the case of EVT-201, we know that this compound is a partial allosteric modulator, which means that, in contrast to full agonists, EVT-201 only has partial efficacy at the GABA-A receptor site. This implies a couple of things — mainly that EVT-201 is less potent than other benzodiazepines that are full agonists and, because of this, likely has a reduced incidence of side effects.
And in terms of pharmacokinetics, the three to four-hour elimination half-life of EVT-201 gives it some meaningful benefits over traditional short-acting benzodiazepine hypnotics. First, it has a longer elimination half-life than the short-acting BzRAs and thus sustains a longer sleep time than the latter. However, it sustains a weaker residual side effect and less risk of tolerance than other long-acting benzo hypnotics drugs whose average half-lives are over six hours [2].
Is EVT-201 Safe? Risks & Side Effects
As EVT-201 is still in clinical trials, more research needs to be done to safely conclude its risk potential, but there seems to be some encouraging evidence for it. The lowered potency of EVT-201 is thought to result in a more benign side effects profile [3]. In fact, this is the main reason the drug is being developed; its makers are interested in an effective hypnotic compound that performs better when it comes to dyskinesia, residual side effect, tolerance, drug-drug interaction, and memory impairment.
Side Effects of EVT-201
The reduced side effects profile of EVT-201 has not yet been confirmed through peer-reviewed studies. However, even if this were so, EVT-201 would still produce the traditional range of benzodiazepine-related side effects; it would just do it to a lesser degree.
With some differences here and there, all benzodiazepines produce a common set of side effects.
The most common side effects of benzodiazepines include the following:
- Blurred vision
- Confusion
- Constipation
- Dizziness
- Drowsiness
- Dry mouth
- Light-headedness
- Memory problems
- Muscle weakness
- Nausea (feeling sick)
- Slurred speech
- Unsteadiness (especially in older people, who may fall and experience injuries)
Some less common side effects of benzodiazepines include:
- Changes in sexual desire
- Difficulty urinating
- Digestive disturbances
- Headaches
- Incontinence (loss of bladder control)
- Increased saliva production
- Low blood pressure
- Rashes
- Sight problems, such as double vision
- Tremors (shaking)
Benzodiazepine Withdrawal & Dependence
Although to differing degrees, all benzodiazepines have the potential to cause physical dependence and withdrawal symptoms among their users. Indeed, the potential of developing a physical dependence is one of the primary risks that doctors have to contend with when prescribing benzodiazepines.
Users might think that dependence only comes about as a result of benzodiazepine misuse, but this is a mistaken belief. In fact, many benzodiazepines are only prescribed for durations of two to four weeks in order to limit this possibility, and others are only recommended for a maximum duration of seven to 10 consecutive days.
Harm Reduction: EVT-201
There are two primary harm reduction considerations that users have to keep in mind when dealing with all prescription drugs, not just benzodiazepines.
Firstly, prescription drug users must take extreme pains not to engage in any misuse, especially if the medication they’re taking has properties that tend to induce these sorts of behaviors, such as a high potency or short elimination half-life.
And secondly, unless there are no other treatment options available, prescription drug users should never resign themselves to being on a given prescription drug for all their lives. This type of relationship to a drug is all but bound to guarantee the formation of physical and mental dependence and will undoubtedly cause adverse effects in the long run. When dealing with prescription drugs, users obviously should look to fix whatever ails them, but they should also be concerned about getting off said medication as soon as possible. In this sense, the two most important factors to limit are the amount that is taken (go for the minimum effective dose) and the duration of the treatment.
Benzodiazepine Harm Reduction Tips
- 🥣 Don’t mix — Mixing benzodiazepines with other depressants (alcohol, GHB, phenibut, barbiturates, opiates) can be fatal.
- ⏳ Take frequent breaks or plan for a short treatment span — Benzodiazepines can form dependence quickly, so it’s important to stop using the drug periodically.
- 🥄 Always stick to the proper dose — The dosage of benzos can vary substantially. Some drugs require 20 or 30 mg; others can be fatal in doses as low as 3 mg.
- 💊 Be aware of contraindications — Benzodiazepines are significantly more dangerous in older people or those with certain medical conditions.
- 🧪 Test your drugs — If ordering benzos from unregistered vendors (online or street vendors), order a benzo test kit to ensure your pills contain what you think they do.
- 💉 Never snort or inject benzos — Not only does this provide no advantage, but it’s also extremely dangerous. Benzos should be taken orally.
- 🌧 Recognize the signs of addiction — Early warning signs are feeling like you’re not “yourself” without the drug or hiding your habits from loved ones.
- ⚖️ Understand the laws where you live — In most parts of the world, benzodiazepines are only considered legal if given a prescription by a medical doctor.
- 📞 Know where to go if you need help — Help is available for benzodiazepine addiction; you just have to ask for it. Look up “addiction hotline” for more information where you live. (USA: 1-800-662-4357; Canada: 1-866-585-0445; UK: 0300-999-1212).
EVT-201 Drug Interactions
Benzodiazepines should never be mixed with potent pharmacological compounds unless it’s with the approval of a doctor. This is especially true when it comes to drugs that depress the central nervous system (CNS) like alcohol, barbiturates, opioids, or other benzodiazepines. Concomitant CNS-depressant drug use often winds up in severe respiratory depression, which is the leading cause of death among drug overdoses.
Additionally, the metabolism of EVT-201 appears to be at least partially mediated by a CYP enzyme, which means users must take care not to ingest compounds that have the potential to interfere with said enzyme, as this will affect the proper metabolic process for the elimination of EVT-201.
EVT-201 Contraindications
Benzodiazepines share a common set of contraindications. We’ll remind you what those are here:
- Bronchitis
- Chronic obstructive pulmonary disease (COPD)
- Conjunctive use of barbiturates, opiates, or those suffering from alcoholism
- Intellectual disabilities due to frequent paradoxical reactions
- Major depression
- Myasthenia gravis
- Over the age of 65 (high risk)
- Personality disorders
- Sleep apnea
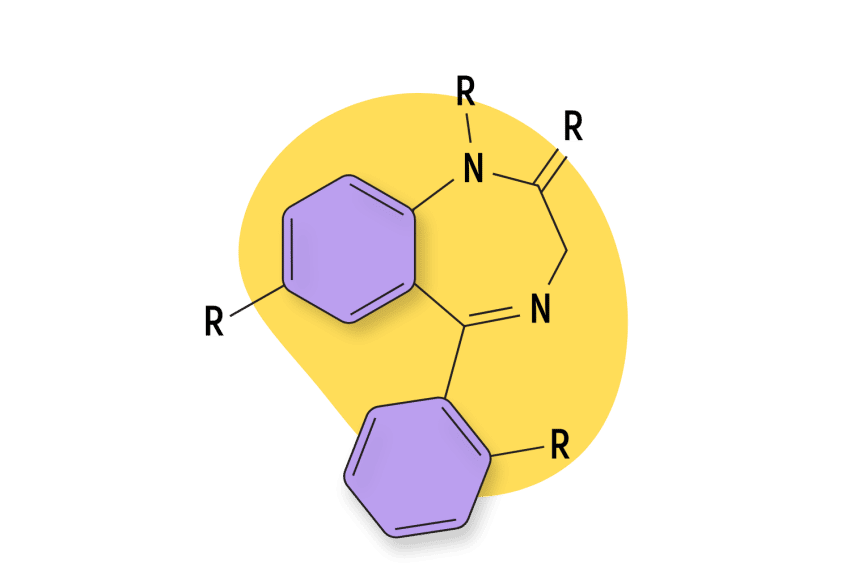
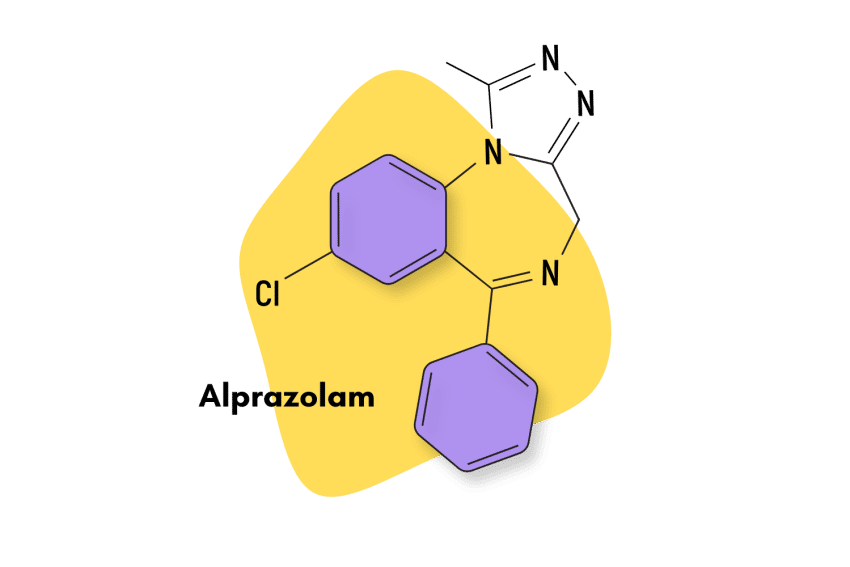
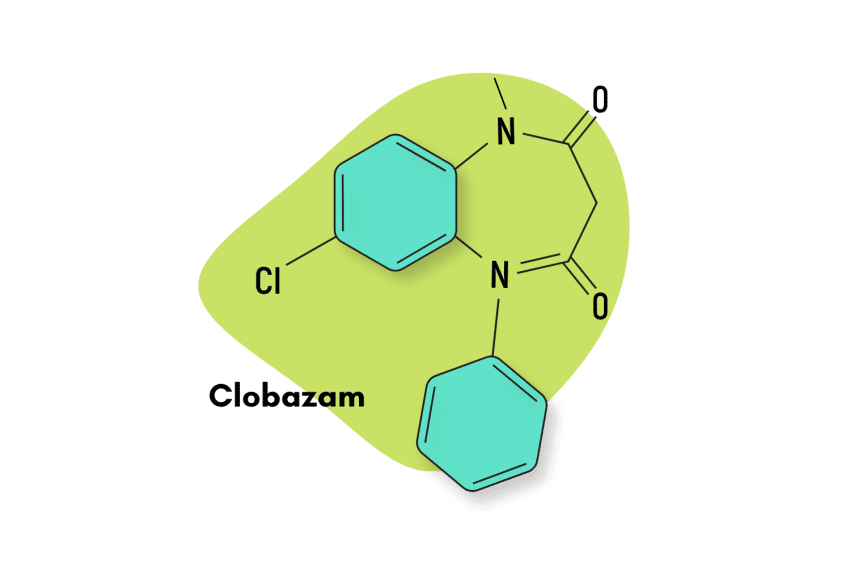
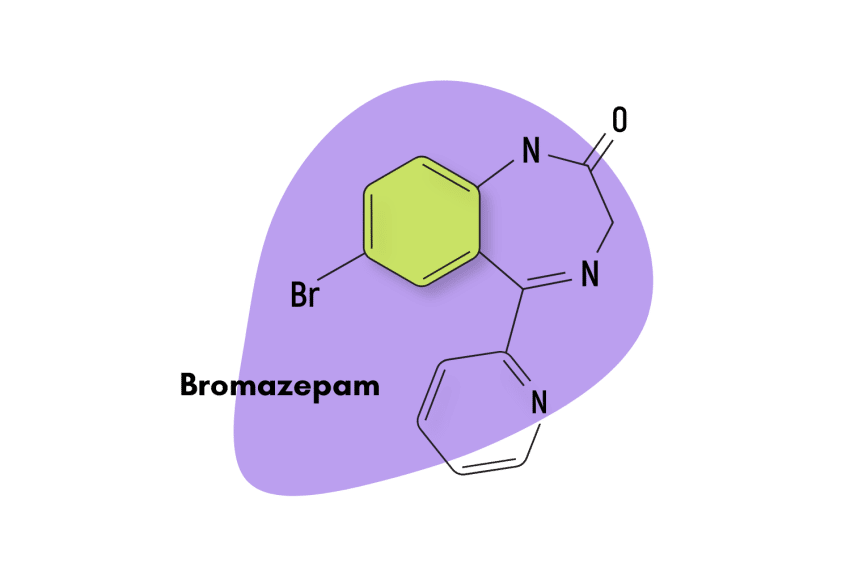
Similar Benzodiazepines
Seeing as EVT-201 is not available yet, here are some benzodiazepine compounds with comparable characteristics.
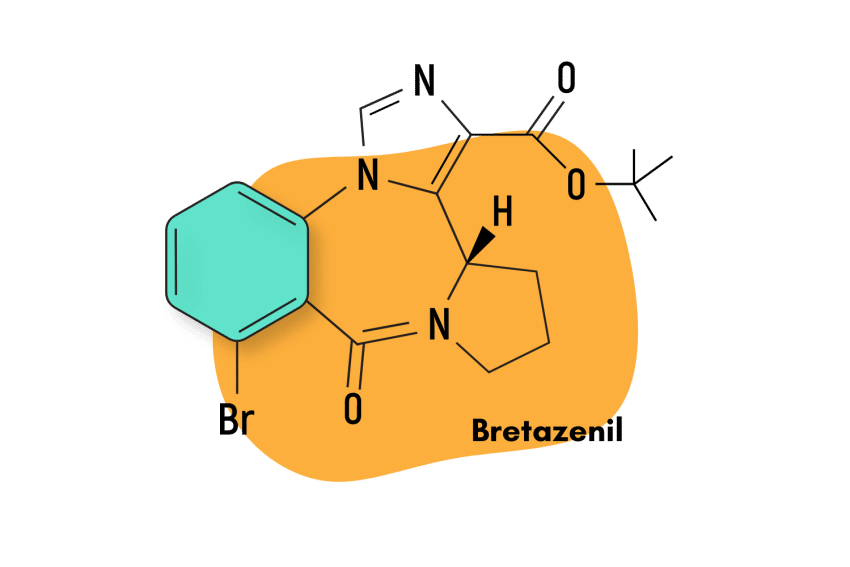
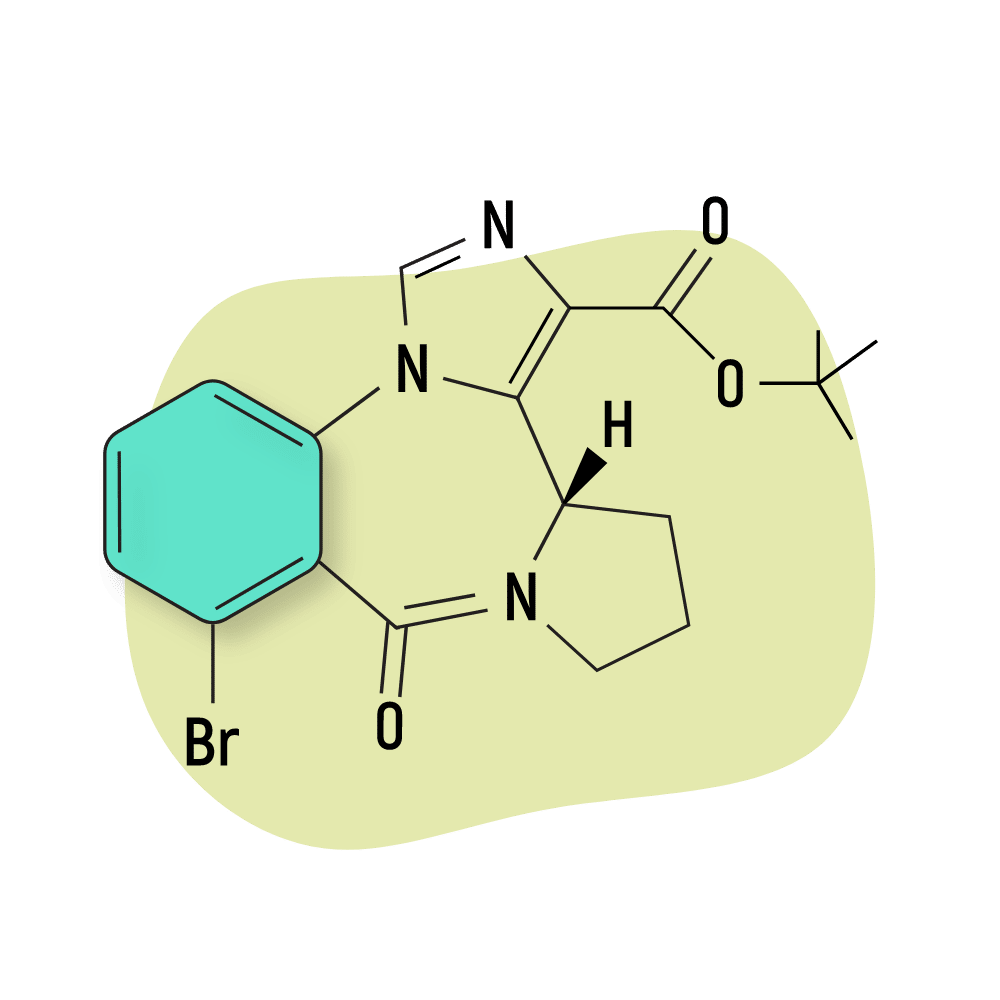
Bretazenil
Bretazenil, like EVT-201, is also an imidazobenzodiazepine, and thus the two have an almost identical chemical structure. As members of the same sub-class, they’re thought to share pharmacological traits like a reduced tendency for side effects as well as physical dependence.
FG-8205
FG-8205 is another imidazobenzodiazepine compound. It is most similar to bretazenil, and like EVT-201, it has not yet been approved as a medication. Not much is known about this compound, but the scant evidence that exists suggests that, like other benzodiazepines in its class, it has less of a marked tendency towards sedation and side effects.
Alternatives to Benzodiazepines
As more natural alternatives to benzodiazepines keep gaining popularity, replacing your benzo prescription with a safer, natural alternative is now more viable than ever!
Kava
The kava plant (Piper methysticum) is a tropical plant species with proven anxiolytic and sedative benefits [4]. The kava plant also interacts with GABA-A receptors but does so in a different way than benzodiazepines. And like all-natural compounds, kava’s side effects profile is less risky.
Kratom
Kratom (Mytragana speciosa) is another plant species with effective pharmacological benefits. However, kratom’s effects are more varied than kava. Depending on the dosage, kratom can produce stimulant and euphoric benefits, or, on the other hand, it can give rise to anxiolytic and sedative properties [5].
EVT-201 FAQs
What company is developing EVT-201?
EVT-201 was originally developed by Roche, but it was sold to Evotec, which is now developing it.
What are EVT-201’s GABA-A subunit affinities?
EVT-201 displays two to four times more affinity for the α1 subunit relative to the α2, α3, and α5 subunits.
References
- Zhang, P., Zhang, W., Liu, R., Harris, B., Skolnick, P., & Cook, J. M. (1995). Synthesis of novel imidazobenzodiazepines as probes of the pharmacophore for” diazepam-insensitive” GABAA receptors. Journal of medicinal chemistry, 38(10), 1679-1688.
- Zhou, C., Cai, X., Zhang, Y., Pan, C., Wang, C., Zhai, S., … & Zhang, X. (2020). Accurate quantification of EVT201 and its two metabolites in human urine using UHPLC-MS/MS method with solid phase extraction. Journal of Analytical Science and Technology, 11(1), 1-11.
- Monti JM, Pandi-Perumal SR, Möhler H (28 September 2010). GABA and Sleep: Molecular, Functional and Clinical Aspects. Springer Science & Business Media. pp. 50–51. ISBN 978-3-0346-0226-6.
- Sarris, J., Stough, C., Bousman, C. A., Wahid, Z. T., Murray, G., Teschke, R., … & Schweitzer, I. (2013). Kava in the treatment of generalized anxiety disorder: a double-blind, randomized, placebo-controlled study. Journal of clinical psychopharmacology, 33(5), 643-648.
- Eastlack, S. C., Cornett, E. M., & Kaye, A. D. (2020). Kratom—Pharmacology, clinical implications, and outlook: a comprehensive review. Pain and therapy, 9(1), 55-69.