Nasal Ketamine: Effects, Dosage, & Safety
In the past, snorting ketamine was the go-to for most recreational users — but the tides are shifting, and nasal ketamine is working its way into the medical system.
Ketamine (AKA “special K”) is a type of dissociative drug developed in the 1960s as a replacement anesthetic for phencyclidine (PCP) — which at the time was the standard anesthetic used during surgery.
Today, ketamine is used for far more than just anesthesia. It’s one of the most popular (and only legal) psychedelic substances used in a conventional medical setting.
Millions of people around the world use ketamine recreationally too. In lower doses, it produces feelings similar to being drunk on alcohol, while higher doses are profoundly psychedelic (see our piece on K-holing on ketamine for more information).
The most common way of using ketamine recreationally is via insufflation — which is just a fancy way of saying, “you snort it.”
Insufflation has always had a negative connotation because of its link to the illegal drug world. But things are changing.
Johnson and Jonson recently launched a new ketamine nasal spray designed to treat depression and other mood disorders. They call it Spravato.
Here, we’ll explore why snorting ketamine has been stigmatized and why researchers and doctors alike are reintegrating this practice into the modern medical model.
Nasal Ketamine: Applications, Benefits, & Characteristics
The areas where nasal ketamine’s benefits have been meaningfully explored are the following: treatment-resistant depression, anxiety disorders, acute pain management, adjunct anesthesia medication, and palliative care.
Let’s review each of these fields in order to understand ketamine’s benefits and assess the state of the research.
Treatment-Resistant Depression & Anxiety Disorders
The potential of formerly maligned psychoactive drugs, like psychedelics, dissociatives, and empathogens, to meaningfully alleviate and even cure depressive and anxiety-related symptoms is one of the most exciting frontiers in modern medicine.
Many of these compounds are now being researched for their therapeutic potential, and when it comes to ketamine, the body of evidence is becoming increasingly difficult to deny.
Hundreds of primary studies as well as systematic meta-analyses, have now confirmed ketamine’s significant ability to improve depressive symptoms in patients who exhibit treatment-resistant depression (TRD) [1]. Due to the nature of TRD, this is an extremely encouraging development, as many of these patients have had no meaningful response to other forms of treatment.
These benefits are also present for other mood-related ailments like generalized anxiety disorder (GAD), social anxiety disorder (SAD), and even bipolar disorder [2].
The research highlights the fast-acting response of ketamine’s benefits but also points out its transient nature. Patients feel improved symptoms in less than four hours, but after a 7-day period, they tend to report diminished benefits. These results suggest that multiple doses of ketamine might be more effective than single-dose treatments, but more research is still needed.
Most papers also mention the fact that long-term research on ketamine’s safety and efficacy is sorely lacking, which means they’re hesitant to call for ketamine’s mainstream adoption until more is known.
At this point, it’s clear that ketamine research needs to focus on producing long-term data, the benefits and characteristics of single-dose vs. multiple-dose treatments, how to make ketamine’s benefits more long-lasting, and the viability of combining ketamine with other medications and forms of treatment like, for example, therapy.
IV ketamine infusions are still an ‘off-label’ treatment when it comes to mood disorders, but a nasal ketamine product has been given the green light by the FDA and is now commercialized under the name Spravato.
However, Spravato is only indicated in conjunction with a more traditional oral antidepressant, like an SSRI, for example, and cannot be taken home. It can only be utilized in a medical facility under the presence of a doctor.

Pain Management
The analgesic potential of ketamine is more widely accepted than its mood-based benefits, and the FDA has approved ketamine for pain management purposes.
The evidence for ketamine’s analgesic benefits is quite substantial. However, because the pain response is quite complex and many different types of pain exist, it’s important to understand the subtleties in the clinical literature.
Ketamine is most effective at reducing pain-related symptoms in conditions of chronic pain, especially neuropathic chronic pain, but when it comes to acute and non-surgical pain, it has proved less effective [3].
At the moment, there is no nasal ketamine-based product for pain management. Ketamine for pain is almost exclusively utilized through intravenous infusions in medical settings like a hospital or specialized clinics and under the supervision and management of medical professionals.
In fact, the research on nasal ketamine applications for pain seems to be quite sparse when compared to other areas of interest, although there is evidence for nasal ketamine’s potential application in pain management [4].
The general conclusions that can be found in the literature are similar to those in depression and anxiety-related studies. Ketamine has a fast-acting and robust effect on pain symptoms. The transient nature of the effects is still present, but some patients do experience sustained pain relief after only one session. There appears to be a high variability when it comes to the number of ketamine sessions needed to experience long-term relief.
A secondary point, though no less important, has been the suggestion that ketamine’s pain management benefits should be given more consideration in light of the many problems that arise due to the use of opioid painkillers. As the opioid epidemic has laid out in a disastrous fashion, these medications carry considerable risk, both in the development of addictive behaviors and in the likelihood of severe side effects like respiratory depression.
It’s likely that a nasal ketamine product might soon be developed, but we can’t speculate with any degree of certainty.
Adjunctive Anesthesia
Nasal ketamine is used as an adjunct medication for anesthesia in certain situations, especially when IV administration is not feasible or preferred, such as in pediatric patients with difficult venous access or other specific situations.
After it was originally rolled out, the medical community began to move away from ketamine as an anesthetic agent primarily due to its propensity to depress the nervous system, an effect that can lead to dangerous conditions such as respiratory depression.
However, recent research has demonstrated that when ketamine is used in conjunction with other anesthetic agents, its safety profile improves, and it becomes a lot better suited to handle certain situations.
Research has found that intranasal ketamine assists doctors with a variety of preinduction measures related to pediatric surgery. For example, nasal ketamine leads to better cooperation on the part of the child and allows for a more pleasant and rapid separation from the parents. It also does not cause significant delays in postanesthetic recovery or delayed discharges home [5].
In general, it has been found that ketamine, by itself or with another medication like midazolam, provides excellent conditions for the induction of anesthesia in pediatric patients.
Palliative Care
Palliative care refers to the many different types of medical interventions designed to provide relief from symptoms and improve the quality of life of patients with serious, often terminal, illnesses.
The specific benefits and uses of nasal ketamine in the context of palliative care will be highly dependent on the individual patient’s conditions and symptoms. Nasal ketamine could, for example, be utilized as a way to reduce depressive feelings in the face of a terminal diagnosis or to help manage pain symptoms arising out of painful medical procedures like chemotherapy.
Nasal Ketamine vs. IV Ketamine
The two formulations which take up the breadth of medicinal ketamine research are nasal and intravenous infusion. Both methods of administration have been proven effective and have different strengths and weaknesses.
Here are some of the benefits of nasal ketamine when compared to IV ketamine:
Ease of Administration
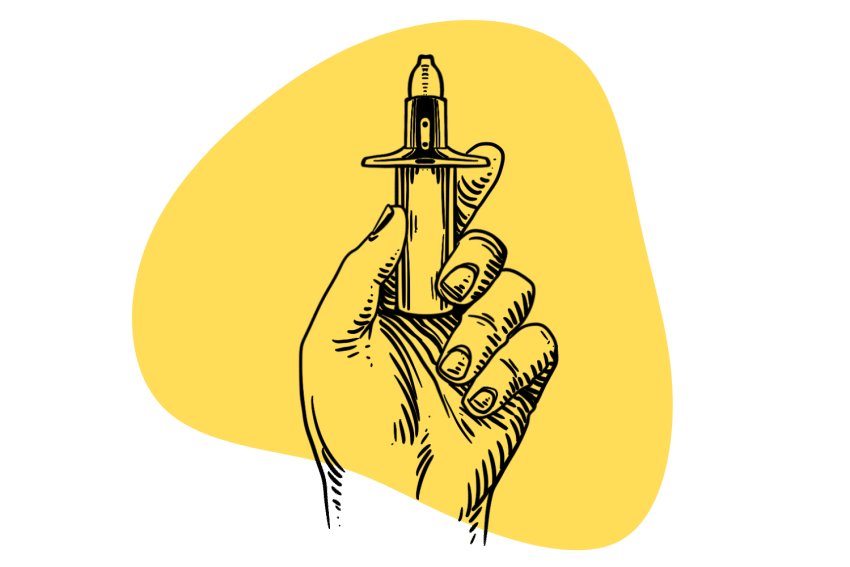
Nasal ketamine is administered as a spray or mist that goes into the nasal passage. This is a fairly simple method that pretty much anyone can do, even children or the elderly. In certain situations, IV access can be difficult to achieve, and easier methods like nasal ketamine may be required.
Reduced Risk of Complications
IV infusions always carry the potential to develop certain complications like infection of the injection site and other such things. Nasal ketamine sidesteps these problems altogether.
Potential for Self-Administration
As stated before, IV ketamine infusions require the presence of medical staff and are almost exclusively carried out in specialized medical settings. This can prove to be a significant hassle as patients have to move locations, and IV ketamine infusions can last for hours. Nasal ketamine allows patients to access ketamine’s benefits without so much trouble.
Potential for Titration
Nasal ketamine may be more amenable to titration, or adjustment of dosage, compared to IV ketamine, as it can be administered in smaller incremental doses. This may allow for more precise dosing and optimization of the treatment regimen for individual patients.
Lower Cost
In some cases, nasal ketamine therapy may be more cost-effective compared to IV ketamine therapy, as it may require less equipment and monitoring and may not necessitate the presence of a healthcare professional for administration.
Nasal Ketamine: FAQs
Answering the most common questions we receive around the intranasal application of ketamine.
1. How Does Ketamine Work?
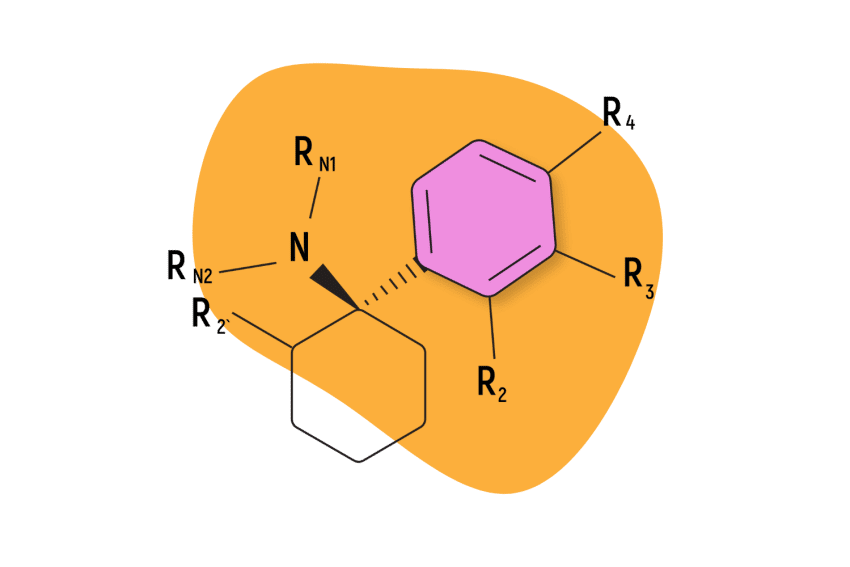
Ketamine works by interacting with various receptors in the brain and central nervous system, primarily N-methyl-D-aspartate (NMDA) receptors, which are involved in the transmission of pain signals and play a role in the regulation of mood, cognition, and perception.
Ketamine is thought to exert its effects through a complex mechanism of action, which includes blocking NMDA receptors and inhibiting the reuptake of certain neurotransmitters such as glutamate, dopamine, and norepinephrine. This leads to a decrease in excitatory neurotransmission and an increase in inhibitory neurotransmission, resulting in the characteristic dissociative and analgesic effects of ketamine.
Additionally, ketamine has been found to have unique effects on the default mode network (DMN) in the brain, which is a network of brain regions involved in self-referential thinking and rumination. Ketamine has been shown to transiently disrupt the normal activity of the DMN, leading to alterations in perception, consciousness, and subjective experience.
The exact mechanisms by which ketamine produces its antidepressant effects, which have been observed in some clinical settings, are not yet fully understood and are an active area of research.
2. What are the Side Effects of Ketamine?
Ketamine is a potent medication that can produce a range of side effects.
Common side effects of ketamine include dissociation, which can involve a feeling of detachment from one’s surroundings, altered perception of time, space, and self, and sensory distortions. Ketamine can also cause sedation and drowsiness, and many users also complain of headaches.
Dizziness, vertigo, and nausea are also common ketamine side effects, particularly during or shortly after administration.
Ketamine can cause an increase in blood pressure and heart rate, which may be a concern in patients with pre-existing cardiovascular conditions but is otherwise considered normal.
3. Is Spravato a Prescription Drug?
Yes, Spravato (esketamine) is a prescription medication that requires a valid prescription from a qualified healthcare professional. It’s an FDA-approved nasal spray formulation of esketamine, which is a type of ketamine, for the treatment of the major depressive disorder (MDD) in adults who have not responded adequately to other antidepressant treatments.
Spravato is a controlled substance and is only available through a restricted distribution program called the Spravato REMS (Risk Evaluation and Mitigation Strategy) due to its potential for abuse and adverse effects.
It should only be used under the supervision of a healthcare professional in approved healthcare settings.
4. How Much Does Nasal Ketamine Therapy Cost?
The costs associated with nasal ketamine therapy, such as Spravato, can vary depending on several factors. One of the main costs is the medication itself, which may be priced per dose or per treatment session and can vary depending on the dosage and frequency of administration.
Additionally, there may be administration costs, which include fees charged by the healthcare professional or clinic for administering the medication, as well as any associated monitoring, assessments, or procedures.
Other medical costs may also be incurred, such as pre-treatment evaluations, follow-up visits, laboratory tests, and other medical services that may be required as part of the treatment protocol.
It’s important to note that insurance coverage for nasal ketamine therapy can vary depending on the specific insurance plan, and patients are encouraged to check with their insurance provider to understand their coverage and potential out-of-pocket costs. Some clinics may offer financial assistance programs, discounts, or payment plans to help make the therapy more affordable for patients.
5. Will I Get High if I Use Nasal Ketamine for Pain or Depression? What Are the Effects?
The use of nasal ketamine for pain or depression, when administered under the supervision of a qualified healthcare professional and according to approved protocols, is typically aimed at therapeutic effects rather than recreational use. Also, the dose typically utilized for recreational purposes is significantly higher than the therapeutic doses utilized in ketamine therapy.
As such, if dissociative effects do appear, they are typically less intense than those that a recreational user might experience. In order to hedge against this possibility, the dosage and administration of nasal ketamine will be carefully controlled by professional medical staff.
However, it’s important to understand that the subjective effects produced by ketamine are highly subject to individual variation. What feels like an incredibly overwhelming experience might, to someone else, be far more tolerable or even enjoyable. Ketamine is a highly popular recreational drug, after all.
The ketamine high is referred to as ‘dissociation’ because users often feel disconnected from themselves and the world, even from their own thoughts and sensations.
Another notable effect is euphoria, which is marked by an uplifted mood, increased sociability, and an overall sense of well-being. Users may feel more relaxed, carefree, and uninhibited.
Ketamine can also induce visual and auditory distortions, leading to changes in perception, such as altered colors, shapes, and patterns. Sounds may become distorted, distant, muted, or echoed.
Physical sensations can be affected as well, with ketamine causing a numbing effect where users may feel disconnected from physical sensations, including pain. Additionally, ketamine can impair motor coordination, resulting in a loss of balance, unsteady movements, and difficulty speaking or moving.
6. Is Ketamine Addictive?
As a dissociative psychedelic compound, ketamine displays a very limited potential for addictive behavior. This is a general attribute that extends to all psychedelics in general. For a variety of reasons, these compounds are far less addictive than stimulant or depressant drugs like cocaine and alcohol, respectively.
The nature of psychedelic experiences, which can oftentimes be incredibly overwhelming and emotionally draining, has consistently shown itself to have very little correlation with addictive behavior. This, of course, does not mean that a person cannot become psychologically addicted to psychedelics, especially if they’re using these compounds as a means to escape their real-life problems.
However, the widely held conclusion is that psychedelics do not cause symptoms of physical dependence, nor are they the type of drugs that encourage people to develop unhealthy habits based on reward and pleasure.
Subscribe to Tripsitter: Newsletter & Podcast
Unlock Your Mind: Subscribe for Expert Insights on Psychedelics 🍄🌵
References
- Marcantoni, W. S., Akoumba, B. S., Wassef, M., Mayrand, J., Lai, H., Richard-Devantoy, S., & Beauchamp, S. (2020). A systematic review and meta-analysis of the efficacy of intravenous ketamine infusion for treatment-resistant depression: January 2009–January 2019. Journal of Affective Disorders, 277, 831-841.
- Glue, P., Neehoff, S. M., Medlicott, N. J., Gray, A., Kibby, G., & McNaughton, N. (2018). Safety and efficacy of maintenance ketamine treatment in patients with treatment-refractory generalized anxiety and social anxiety disorders. Journal of Psychopharmacology, 32(6), 663-667.
- Jonkman, K., Dahan, A., van de Donk, T., Aarts, L., Niesters, M., & van Velzen, M. (2017). Ketamine for pain. F1000Research, 6.
- Andolfatto, G., Innes, K., Dick, W., Jenneson, S., Willman, E., Stenstrom, R., … & Benoit, G. (2019). Prehospital analgesia with intranasal ketamine (PAIN-K): a randomized, double-blind trial in adults. Annals of Emergency Medicine, 74(2), 241-250.
- DIAZ, J. (1997). Intranasal ketamine preinduction of pediatric outpatients. Pediatric Anesthesia, 7(4), 273-278.