Can Ketamine Help Bipolar Depressive Disorder?
Research on ketamine for bipolar treatment shows limited potential with varying rates of success, but this doesn’t mean there isn’t some reason for excitement.
Depression is one of the most common reasons people seek out ketamine therapy, but bipolar depression may be a bit more difficult to treat. When ketamine successfully eases symptoms, the benefits rarely last more than a few days.
When ketamine is a tool to bolster therapy, however, it can be tremendously powerful. This is more in line with other forms of psychedelic-assisted psychotherapy, but therapy is often absent or minimal when it comes to ketamine (especially from telehealth providers).
In this article, we’ll cover:
- A Survey of Ketamine Research for Bipolar Depression
- Bipolar Depression’s Potential Treatment With Ketamine
- Ketamine for Bipolar Disorder Typical Dosing Protocol
- What Causes Bipolar Depressive Symptoms
- Whether Ketamine Therapy for Bipolar Treatment is Worth It
- Frequently Asked Questions About Ketamine for Bipolar Depression
Regardless of the route you take, make sure you know about the risks, concerns, and potential of ketamine treatment.
At a Glance: Ketamine Research On Bipolar Disorder
A 2023 review surveyed a total of 235 participants with bipolar depression across all currently available studies and found an average efficacy rate of 48% [1]. These mainly involved “treatment-resistant” patients — meaning other treatments had failed.
Some other key findings include:
- A range of 26–79% success rates across eight studies.
- Single-dose ketamine’s benefit “did not extend beyond the 2-week mark; however…repeated infusions of ketamine over 2 weeks” may help for up to a month.
- Ketamine may have a major impact on suicidal ideation, providing relief within 4 hours of injections, and repeated doses may be able to sustain the impact.
- Researchers excluded 17 studies (more than double the number included) because they didn’t investigate potentially harmful outcomes of ketamine, pointing to a potential problem of bias in research.
- All but one of the studies involve infusions of ketamine; the outlier investigates the proprietary Spravato nasal spray.
- The Spravato study had a response rate of 68.5% after two doses but only 25.5% after one for participants with bipolar depression [2].
As with other forms of mental health or psychedelic-assisted psychotherapies, research is far from conclusive on ketamine for bipolar depression. Studies contain small sample sizes with a dramatic variety of outcomes, but they all seem to agree on ketamine’s short-term benefit.
Within one or two sessions (depending on the study), participants tended to experience an impactful alleviation of symptoms. We don’t have a clear picture of how helpful this is or the best way to extend the effect.
One 2020 study even found that, while ketamine was beneficial for 71% of participants for up to two weeks, symptoms worsened from the starting level after three [3].
Can Ketamine Treat Bipolar Depressive Disorder?
Ketamine seems to have a tremendous — albeit transient — effect on bipolar and unipolar depressive symptoms. While the benefit seems to last a week or two at most, this can still be impactful for episodes of intense anxiety or depression associated with bipolar depression.
Unlike unipolar depression, where patients experience a continual negative effect on mood, bipolar symptoms involve alternating episodes of excitability and depression. Lengthy periods of intense work and attention may give way to days or weeks of finding it difficult to even wake up in the morning.
This destabilization of mood regulation can make life incredibly difficult without treatment and therapeutic intervention. Ketamine will not “cure” any form of depression, and it’s unlikely for any drug to do so, given the traumatic, social, and systemic layers often forming the foundation of the condition [4].
However, the symptoms of depression are often so all-consuming that the deep mental work needed can feel impossible. Ketamine and mental health medications are great for temporarily alleviating those symptoms, making the work easier but not negating the need for it.
Treating bipolar depression — a condition involving extreme swings in mood — can also be dangerous with a drug like ketamine, which alters emotions and perception drastically. The potential for high levels of anxiety or even paranoia makes it unwise to attempt self-treating bipolar depression without medical or psychological oversight.
Most (if not all) studies on ketamine for bipolar depression involve patients dropping out because they had a poor experience with ketamine. This is typically a small percentage of participants, but there’s no way to know how difficult the experience will be ahead of time.
Ketamine Treatment Dosing Schedule for Bipolar Depression
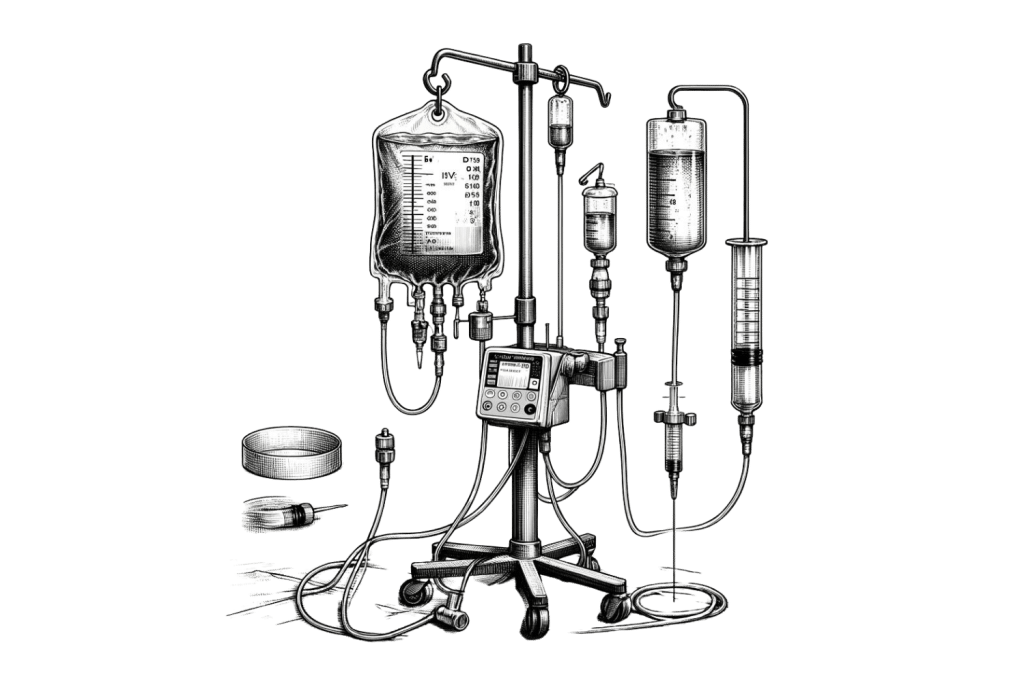
Since ketamine wears off quickly, dosing regimens typically involve multiple doses per month — sometimes per week. Off-label clinics offering infusions or intramuscular shots usually start new patients with two infusions per week for the first month or two before tapering off to lower doses.
Ketamine telehealth companies may follow similar dosing protocols utilizing sublingual lozenges or troches but are more likely to stick to once a week at most. It’s worth noting that telehealth companies offer very little therapeutic support, which can be dangerous when you’re trying to treat any kind of depression.
Johnson & Johnson’s proprietary nasal spray, Spravato, is only technically prescribable for unipolar treatment-resistant depression. Should it ever be an option for bipolar depression, it would likely involve two doses a week along with medication like it currently is for unipolar.
Ketamine for Bipolar Depression: Risks and Concerns
Ketamine therapy involves potentially negative side effects, toxicity concerns, and the potential for serious adverse events.
Some of the common side effects patients can expect to potentially experience on ketamine include:
- Dizziness, nausea, and vomiting
- Blurred vision (potentially lingering for up to an hour after ketamine wears off)
- Loss of coordination or muscle control
- Heavy sedation or body-heaviness
- Cognitive impairment (holes in memory, trouble reasoning or concentrating, etc.)
- Elevated heart rate and blood pressure
- Auditory and visual hallucinations
- Slowed breathing
- Anxiety, paranoia, and agitation
There are also serious concerns surrounding ketamine’s impact on the following:
- Urinary Tract — The most common problem with frequent ketamine use involves damage to the urinary tract, which can lead to problems with urination, infections, and other problems [5].
- Bladder — Untreated urinary problems have the potential to harm the bladder, potentially requiring emergency care if ketamine use continues.
- Liver — Mostly a concern for long-term abuse of ketamine, the liver’s job is filtering out toxins, and overwhelming it can cause infection, dysfunction, and other serious problems [6].
- Heart and Lungs — Though the low impact on the cardiovascular and respiratory system is unlikely to cause severe damage, prolonged stress or prior medical conditions can lead to medical concerns [7].
- Brain — Some research suggests the long-term impact of using ketamine could result in a decline in learning capabilities and reasoning potential [8].
Always discuss ketamine treatment with a mental health care provider — preferably not employed by a ketamine clinic — before starting treatment.
People on anti-psychotic, cardiovascular, respiratory, and sedative/impairing medications or drugs should not take ketamine.
Is Ketamine Therapy for Bipolar Depression Worth It?
Treatment for each person will vary, and, for some, ketamine can lead to dramatic — albeit temporary — relief. However, ketamine therapy is not cheap, and the protocols can call for up to two doses per week, leading to a steep price tag.
Bipolar depression requires therapeutic intervention, and no pharmaceutical approach is likely to bring lasting relief. Depressive symptoms and those of many other mental health conditions have deep psychological roots, and pharmaceutical approaches mostly make it easier to pull them out through therapy.
Depressive episodes can make facing the day difficult, let alone trying to dive deep into a session with a psychologist. The rapid relief of depressive symptoms can provide tremendous relief and help with therapeutic sessions.
While it’s not a “cure,” ketamine may provide hope for many who struggle with bipolar depression in this way. However, it’s worth noting that research on bipolar treatment with ketamine is limited, and the success rate within those studies has a wide range.
For some, the dissociative effects of ketamine can feel overwhelming, potentially even worsening their condition in the long run. Anyone seeking ketamine treatment should discuss it thoroughly with a mental health professional beforehand — especially when going into it with a mental health condition.
What Causes Bipolar Depression?
There are a plethora of “causes” behind all complex mental health conditions, ranging from genetic to social factors. While each person’s root cause for the condition is different, there are some common neurological triggers behind the symptoms (or “pathophysiology”).
Here are the causes, summarized in three parts [9]:
- Neurotransmitter Signaling — Damage to the flow and production of serotonin and dopamine leads to dysregulation in mood and the “reward system.” This makes it hard to find motivation or feel pleasure from accomplishments or beneficial events.
- Abnormal Connections — Through the above (and likely other triggers), areas of the brain begin to couple with other networks they don’t normally interact with. This “dysbalance between networks” is likely behind many of the manic and depressive symptoms.
- Deterioration — “[A]dditional contribution of gray matter alterations and related cognitive deterioration” may occur in some bipolar patients, leading to a decline in learning and impulse control.
Most research agrees that the cascading events above stem largely from the dysfunction of dopamine — which is common in bipolar and unipolar depression [10]. While we think dopamine is purely a “reward,” it also acts as a motivator, giving small amounts in preparation for beneficial tasks like exercise or large projects.
In bipolar depression, there is likely less dopamine production in times of depression and an increased sensitivity to dopamine during manic episodes. While the mechanisms behind this aren’t well understood, long periods of lower dopamine levels may sensitize the receptors to the rewarding sensation during episodes of mania.
Ketamine may help by strengthening the “connections between two brain regions that are involved in the production and regulation of dopamine ” [11]. The effects are temporary but could explain the quick alleviation of depressive symptoms.
FAQ: Ketamine for Bipolar Depressive Disorder
Here are some of the questions people most frequently ask about ketamine treatment for bipolar depression:
1. Can You Take Ketamine While On Medications?
You shouldn’t take ketamine without medical supervision while on medications, but some courses of treatment encourage patients to continue their medication. This largely applies to the depression medication, selective serotonin reuptake inhibitors (SSRIs).
Ultimately, this is a discussion you and your provider should have beforehand, but don’t take ketamine along with the following types of medications:
- Cardiovascular
- Respiratory
- Opiate/Sedative
- Anti-psychotic
- Amphetamines/Stimulants
This is not an exhaustive list, and even some over-the-counter medications can dampen or synergize ketamine’s potency.
2. Is Ketamine Approved to Treat Bipolar Depression?
No — Spravto is the only FDA-approved form of ketamine, with treatment-resistant unipolar depression as the only indication. Several off-label clinics will treat bipolar depression with ketamine to varying effects.
Practitioners largely follow a similar dosing protocol for bipolar depression as for unipolar, but each person is different. Depending on your tolerance to ketamine, how well it affects your symptoms, and more, a clinician will determine the correct dose (at least the dose they think is right) for you.
3. How Long Does Ketamine Relieve Bipolar Symptoms?
Ketamine provides rapid, temporary relief for a short period. For some, the benefits wear off along with the drug, but some outliers have had relief for multiple weeks.
It’s important to separate the condition from the symptoms and recognize that symptom relief can have tremendous benefits, but it’s not the same as a cure.
4. How Does Ketamine Help With Bipolar Depression?
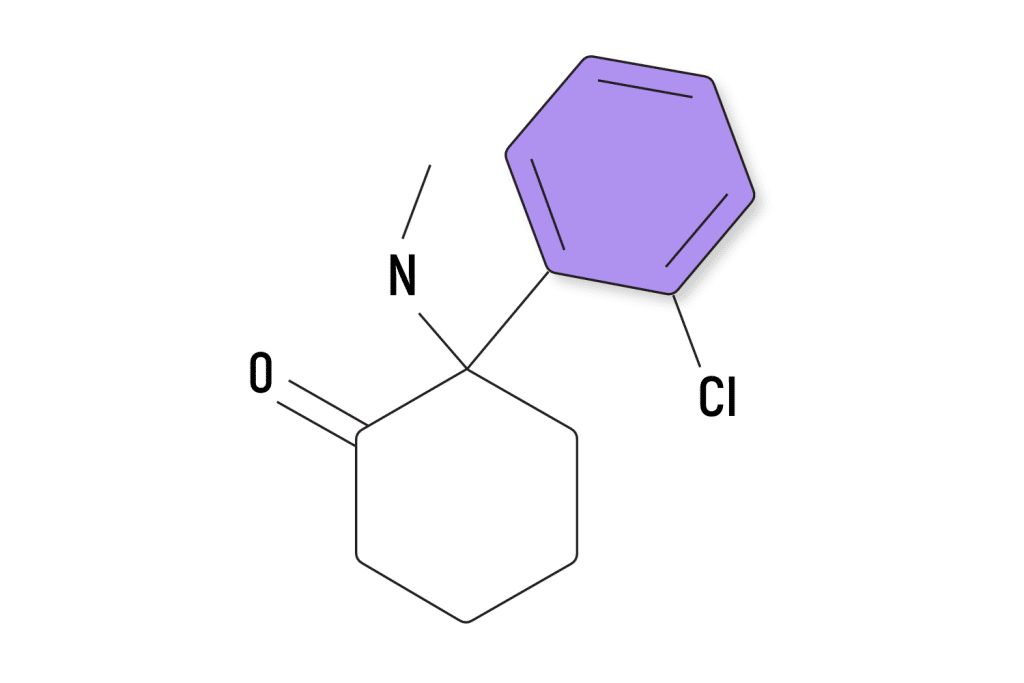
Ketamine is useful for bipolar depression in ways we aren’t fully aware of, but glutamate, dopamine, and serotonin are likely a big part of it. These help with stimulating the brain, mood regulation, emotional control, impulsiveness, memory formation, and a host of other functions that contribute to depressive symptoms.
5. Is Ketamine Better for Bipolar or Unipolar Depression?
Evidence seems to point toward ketamine being more effective for unipolar depression, though research is scarce. This doesn’t mean it can’t help — some studies have a large percentage of participants reporting successes — but its help is limited.
Even perfect candidates for ketamine therapy may find themselves non-responsive to it, and each person’s needs are different.
References
- Fancy, F., Haikazian, S., Johnson, D. E., Chen-Li, D. C. J., Levinta, A., Husain, M. I., Mansur, R. B., & Rosenblat, J. D. (2023). Ketamine for bipolar depression: An updated systematic review. Therapeutic Advances in Psychopharmacology, 13, 20451253231202723. https://doi.org/10.1177/20451253231202723
- Martinotti, G., Dell’Osso, B., Di Lorenzo, G., Maina, G., Bertolino, A., Clerici, M., Barlati, S., Rosso, G., Di Nicola, M., Marcatili, M., d’Andrea, G., Cavallotto, C., Chiappini, S., De Filippis, S., Nicolò, G., De Fazio, P., Andriola, I., Zanardi, R., Nucifora, D., … Group, the R.-E. S. (2023). Treating bipolar depression with esketamine: Safety and effectiveness data from a naturalistic multicentric study on esketamine in bipolar versus unipolar treatment-resistant depression. Bipolar Disorders, 25(3), 233–244. https://doi.org/10.1111/bdi.13296
- Zhuo, C., Ji, F., Tian, H., Wang, L., Jia, F., Jiang, D., Chen, C., Zhou, C., Lin, X., & Zhu, J. (2020). Transient effects of multi‐infusion ketamine augmentation on treatment‐resistant depressive symptoms in patients with treatment‐resistant bipolar depression – An open‐label three‐week pilot study. Brain and Behavior, 10(8), e01674. https://doi.org/10.1002/brb3.1674
- Johnson, S. L., Cuellar, A., & Gershon, A. (2016). The Influence of Trauma, Life Events, and Social Relationships on Bipolar Depression. The Psychiatric Clinics of North America, 39(1), 87–94. https://doi.org/10.1016/j.psc.2015.09.003
- Srirangam, S., & Mercer, J. (2012). Ketamine bladder syndrome: An important differential diagnosis when assessing a patient with persistent lower urinary tract symptoms. BMJ Case Reports, 2012, bcr2012006447. https://doi.org/10.1136/bcr-2012-006447
- Henrie, J., Gerard, L., Declerfayt, C., Lejeune, A., Baldin, P., Robert, A., Laterre, P.-F., & Hantson, P. (2023). Profile of liver cholestatic biomarkers following prolonged ketamine administration in patients with COVID-19. BMC Anesthesiology, 23(1), 44. https://doi.org/10.1186/s12871-023-02006-2
- Szarmach, J., Cubała, W. J., Włodarczyk, A., & Wiglusz, M. S. (2019). Short-term ketamine administration in treatment-resistant depression: Focus on cardiovascular safety. Psychiatria Danubina, 31(Suppl 3), 585–590.
- de Carvalho Cartágenes, S., Fernandes, L. M. P., Carvalheiro, T. C. V. S., de Sousa, T. M., Gomes, A. R. Q., Monteiro, M. C., de Oliveira Paraense, R. S., Crespo-López, M. E., Lima, R. R., Fontes-Júnior, E. A., Prediger, R. D., & Maia, C. S. F. (2019). “Special K” Drug on Adolescent Rats: Oxidative Damage and Neurobehavioral Impairments. Oxidative Medicine and Cellular Longevity, 2019, 5452727. https://doi.org/10.1155/2019/5452727
- Magioncalda, P., & Martino, M. (2022). A unified model of the pathophysiology of bipolar disorder. Molecular Psychiatry, 27(1), Article 1. https://doi.org/10.1038/s41380-021-01091-4
- Satterthwaite, T. D., Kable, J. W., Vandekar, L., Katchmar, N., Bassett, D. S., Baldassano, C. F., Ruparel, K., Elliott, M. A., Sheline, Y. I., Gur, R. C., Gur, R. E., Davatzikos, C., Leibenluft, E., Thase, M. E., & Wolf, D. H. (2015). Common and Dissociable Dysfunction of the Reward System in Bipolar and Unipolar Depression. Neuropsychopharmacology, 40(9), Article 9. https://doi.org/10.1038/npp.2015.75
- Marcus, D. J., & Bruchas, M. R. (n.d.). Where ketamine and dopamine collide. eLife, 10, e70148. https://doi.org/10.7554/eLife.70148