Ketamine for Dogs: Applications, Safety Concerns, Common Dosing
Ketamine is often used in veterinary medicine, but for what, and how safe is it really?
You may also be familiar with ketamine as a recreational drug, but veterinarians have used it for its anesthetic properties, though it’s also helpful for pain control in specific scenarios like post-operative pain or, in some cases, cancer. When administered correctly and in the right context, ketamine is considered safe for canines.
In this article, we’ll take a closer look at the use of ketamine for dogs.
But before jumping in, we want to clarify that this article is for educational purposes only. You should never administer or share ketamine or any drug with your pets without a veterinarian’s guidance.
With that out of the way, let’s start with the basics.
What Is Ketamine?
Ketamine was first synthesized in the 1960s, and six years later, the first clinical study of ketamine in humans was published. It highlighted ketamine’s ability to induce an unusually altered state of consciousness that distorts perceptions of sight and sounds and produces a feeling of detachment from the environment and oneself.
Researchers and practitioners began referring to ketamine as a “dissociative anesthetic,” capturing the essence of its dual capability to both anesthetize and alter consciousness.
What sets ketamine aside from many anesthetics is its nature to provide pain relief and unconsciousness without significantly depressing the central nervous system. This means that essential functions, like breathing, remain unaffected, reducing the need for mechanical ventilation, which is especially valuable when respiratory support isn’t readily available.
However, outside these medical contexts, ketamine’s reputation takes on a different tone. It’s been recognized, and at times criticized, for its popularity as a recreational drug.
Despite this, while its recreational use has been controversial in the medical world, ketamine continues to be used for a variety of therapeutic applications, from psychedelic-assisted therapy for treating disorders such as depression, PTSD, and anxiety [1] to pain management and as an opioid alternative in human and veterinary medicine.
Related: Medicine for the Mind — Psychedelics for Mental Illness
What Do Vets Use Ketamine for?
Ketamine can be found in various forms suitable for intramuscular and intravenous injections.
These methods allow for a rapid onset of action. Depending on the scenario, a veterinarian might use ketamine alone or combine it with other sedatives or anesthetics to achieve the desired clinical effect.
Here’s a look at some of the ways a vet might use ketamine for dogs:
1. Surgical Anesthesia
One of the primary uses of ketamine in dogs is as an anesthetic agent for surgeries. Ketamine doesn’t depress the cardiovascular system as much as other anesthetics might, making it a preferred choice for veterinary professionals. However, because of its short duration, it’s not often used on its own and has been found to amplify the effects of opioids.
2. Pain Management
Ketamine, especially at lower doses, is an analgesic. It’s occasionally administered for post-operative pain or treating certain chronic pain conditions.
3. Induction Agent
Before administering another anesthetic that can’t be injected directly, vets sometimes use ketamine to initiate the anesthesia. Once the dog is anesthetized with ketamine, the vet can transition it to an inhalant anesthetic for the remainder of the procedure. This technique is often used for longer surgeries as ketamine is known to have a shorter duration.
4. Euthanasia
No pet owner ever wants to consider this topic. In certain situations, ketamine can be part of the drug cocktail for humane euthanasia.
Because ketamine is such a powerful drug, it’s rarely part of a home pain management plan.

How Does Ketamine Work?
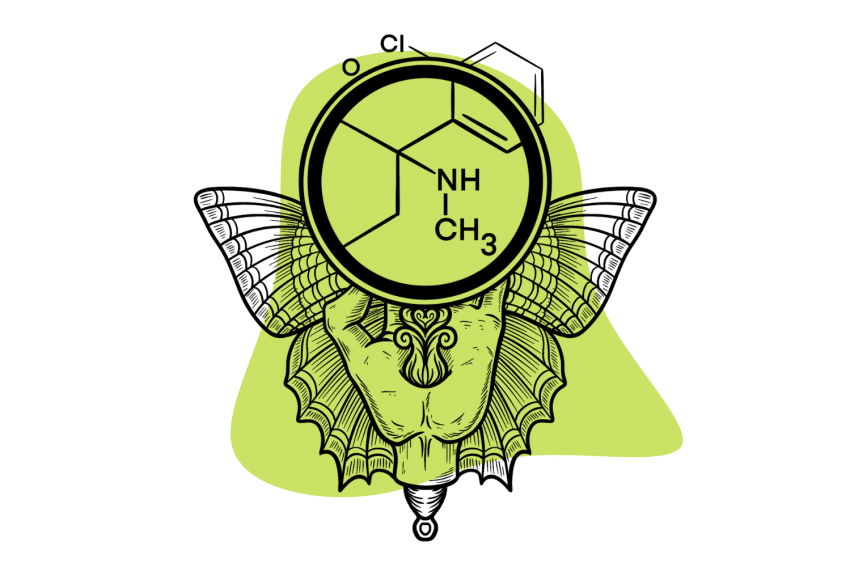
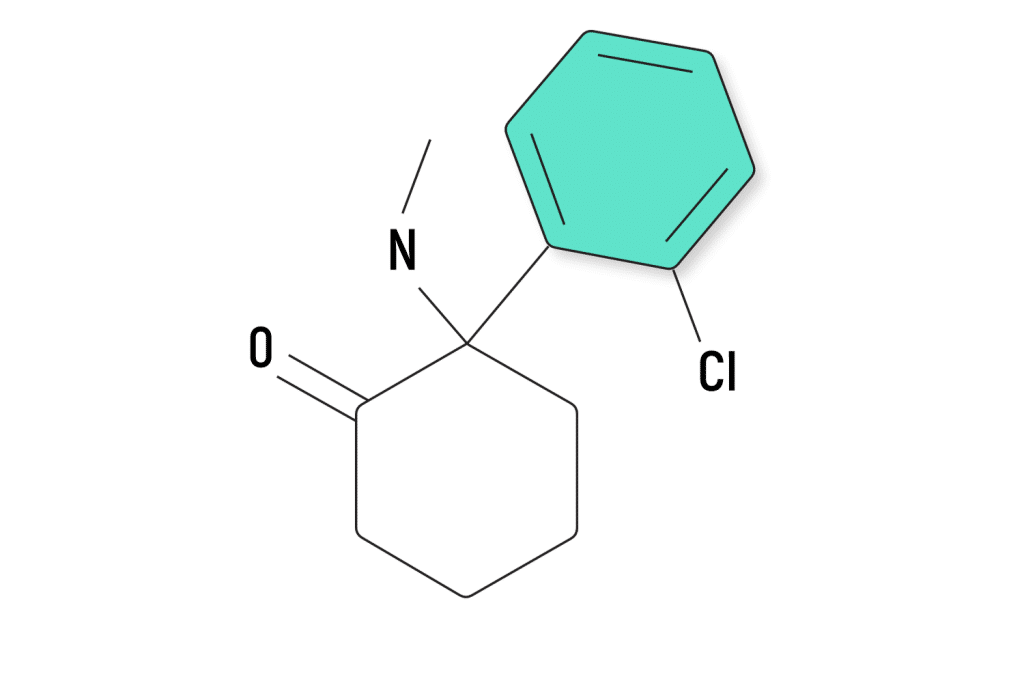
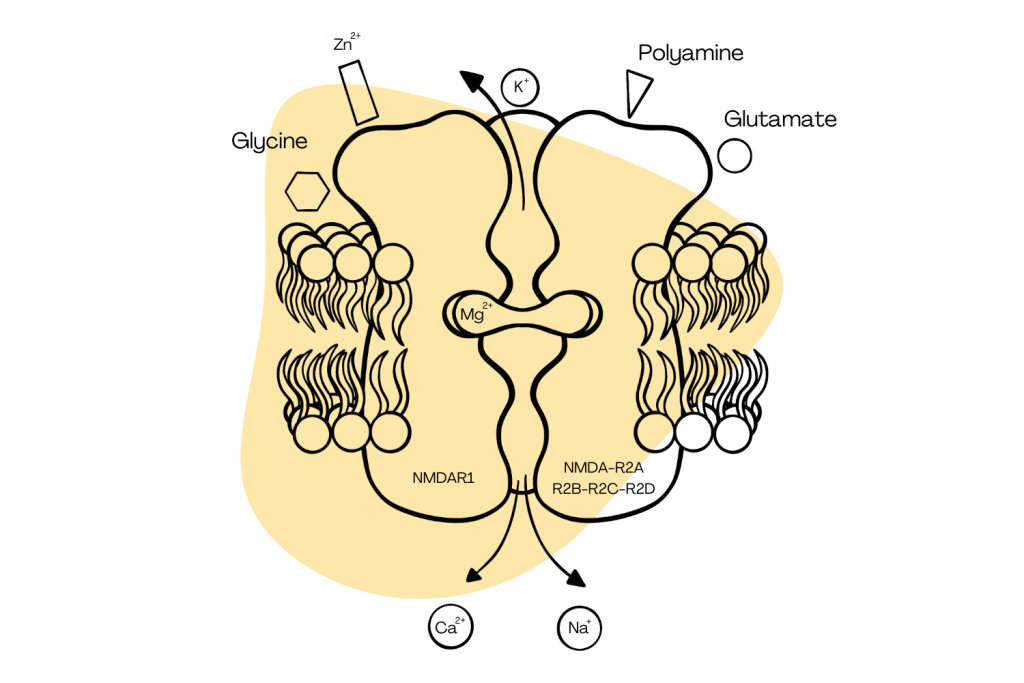
Ketamine operates mainly on the brain and spinal cord’s NMDA (N-methyl-D-aspartate) receptors [2].
NMDA receptors modulate brain plasticity and memory function, among other neurological processes. When ketamine enters the system, it blocks these NMDA receptors, disrupting pain perception and inducing anesthesia in higher dosages — all of this can happen within a minute of dosage.
By interfering with the transmission of signals between nerve cells in the brain and spinal cord, ketamine creates an altered state of consciousness, producing its hallmark dissociative effects.
In lower doses, ketamine doesn’t entirely block these receptors but does change their activity. This modulation provides analgesic effects, offering pain relief without inducing full anesthesia or a total loss of consciousness.
Dogs, like humans, possess NMDA receptors in their central nervous system, making ketamine an effective anesthetic and analgesic agent for them. However, the metabolism, dose-response, and side-effect profile can vary between species, meaning how dogs react to ketamine might differ from humans.
Ketamine for Dogs: Administration and Dosage
We want to underscore the importance of not self-prescribing your pet for their safety.
While the internet can have some great information, it doesn’t replace the expertise of a trained and licensed veterinarian. Only they have the knowledge and experience to prescribe the correct dosages, especially for something as potent as ketamine.
Ketamine is typically administered to dogs in dosages of 6-10 mg/kg through injections directly into the bloodstream via the veins (intravenous fluids) or the muscles (intramuscular). However, for those dogs that are particularly challenging to restrain or handle, there’s an alternative method: spraying ketamine directly into the eyes or mouth.
Just like in humans, the reason for administering ketamine dramatically affects the amount given.
Anesthetic dosages are generally higher than for simple pain relief. For surgeries, a dog might get a higher dose to ensure they remain unconscious, whereas the doses are often much smaller for post-operative pain or chronic pain management.
Age, weight, health history, and current health status also influence how a dog responds to ketamine. For instance, an older dog or one with liver issues might metabolize drugs differently than a young, healthy puppy.
However, for an educational context, research has shown that ketamine dosages for dogs can vary based on the purpose (anesthesia vs. pain relief), the dog’s health status, and other concurrently administered drugs.
Ketamine & Pain Management Post-Surgery
When dogs (or humans) have surgery or suffer from injuries, the affected area can, understandably, be painful. But something more complex can also happen in the nervous system, which makes the road to recovery much more challenging.
This phenomenon is called “central sensitization.”
When an area of the body gets hurt, like during surgery, the nerve endings in that area send more “pain signals” to the brain. Typically, once the injury heals, these signals should be reduced, and the pain should subside.
However, with “central sensitization,” something goes a bit haywire. The constant pain signals from the injury can make the brain and spinal cord more sensitive and overly responsive. This is where ketamine may help protect against hypersensitization.
A study investigated six dogs given different doses of ketamine to see how it affected their pain levels and how much ketamine was in their blood. They also combined ketamine with another drug, lidocaine, in one of the tests.
The right amount of ketamine in a dog’s blood to help with pain is between 100 and 200 units (ng/mL), and all the doses they tested in this study helped reduce pain.
They found that at certain times, the amount of ketamine in the dogs’ blood was different based on the dose they were given. The pain levels returned to normal about 20 minutes after they stopped giving the drug, showing how short-lived ketamine is for dogs.
With these dosages of ketamine, the researchers didn’t observe any harmful side effects, but we need more tests to understand how ketamine may control pain in dogs after surgery [3].
Risks of Using Ketamine for Dogs
Just like humans, our companion animals can react differently to medications. While some may undergo procedures with ketamine or pain treatment plans without a hitch, others might experience some adverse effects.
When researchers gave ketamine at doses of 10 mg/kg intravenously, they found the following reactions that could pose complications:
- Their heart rate, blood pumping capacity, and blood pressure increased. This heightened activity could be risky, especially in dogs with pre-existing health conditions.
- They used more oxygen, produced more carbon dioxide, and breathed slower for a short period. These changes could be concerning, especially when there’s not adequate ventilation.
- The dogs’ body temperature went up after being given ketamine. Elevated body temperatures, if prolonged, can result in heat-related illnesses or complications.
- The study found that oxygen levels in the dogs’ blood temporarily decreased while carbon dioxide levels increased. This can lead to complications if not monitored.
- The effects of ketamine were rapid, but they didn’t last long. This short duration of effects might mean that repeated doses are required.
- A clear sign that the drug influenced the dogs’ muscular system was evident in their stiff muscles and uncontrolled muscle movements. Additionally, the dogs drooled excessively, which might indicate discomfort or a side effect of the drug [4].

Taking Care of Your Dog Post-Operation
After an operation or if your dog has been given a ketamine dosage, your top priority is their safety and comfort, so you’ll want to provide a calm environment. Like humans, dogs can be sensitive to sensory stimulation when on certain medications or recovering from an operation.
If your dog isn’t passed out from drowsiness, they may be unsteady or disoriented. To prevent injuries, limit their activity and closely monitor your dog to ensure they’re breathing normally and not showing signs of distress.
Offer water in small amounts frequently to ensure they stay hydrated. As for food, wait a few hours after the procedure or post-ketamine administration, then offer a small amount of their usual food. If they appear agitated or in pain, call your vet.
While your dog is recovering, it’s best to keep them separated from other pets. This ensures they get the rest they need and prevents any accidental injuries.
The Takeaway: Ketamine for Dogs
Ketamine is often mixed into controversies because of recreational use. However, despite this, it has proven to be a significant asset in human and veterinary medicines. Ketamine’s interactions with NMDA receptors offer a blend of anesthesia and pain relief that can be useful in a number of pivotal treatments for dogs.
However, like all drugs, it comes with risks, so you should never self-administer or share your personal stash of ketamine or any medication with your pets.
Subscribe to Tripsitter: Newsletter & Podcast
Unlock Your Mind: Subscribe for Expert Insights on Psychedelics 🍄🌵
References
- Smith-Apeldoorn, S. Y., Veraart, J. K., Spijker, J., Kamphuis, J., & Schoevers, R. A. (2022). Maintenance ketamine treatment for depression: a systematic review of efficacy, safety, and tolerability. The Lancet Psychiatry, 9(11), 907-921.
- Zhang, Y., Ye, F., Zhang, T., Lv, S., Zhou, L., Du, D., … & Zhu, S. (2021). Structural basis of ketamine action on human NMDA receptors. Nature, 596(7871), 301-305.
- Kaka, U., Saifullah, B., Abubakar, A. A., Goh, Y. M., Fakurazi, S., Kaka, A., … & Chen, H. C. (2016). Serum concentration of ketamine and antinociceptive effects of ketamine and ketamine-lidocaine infusions in conscious dogs. BMC veterinary research, 12(1), 1-10.
- Haskins, S. C., Farver, T. B., & Patz, J. D. (1985). Ketamine in dogs. American Journal of Veterinary Research, 46(9), 1855-1860.