From Anesthetic to Antidepressant: Understanding the Versatility of IV Ketamine
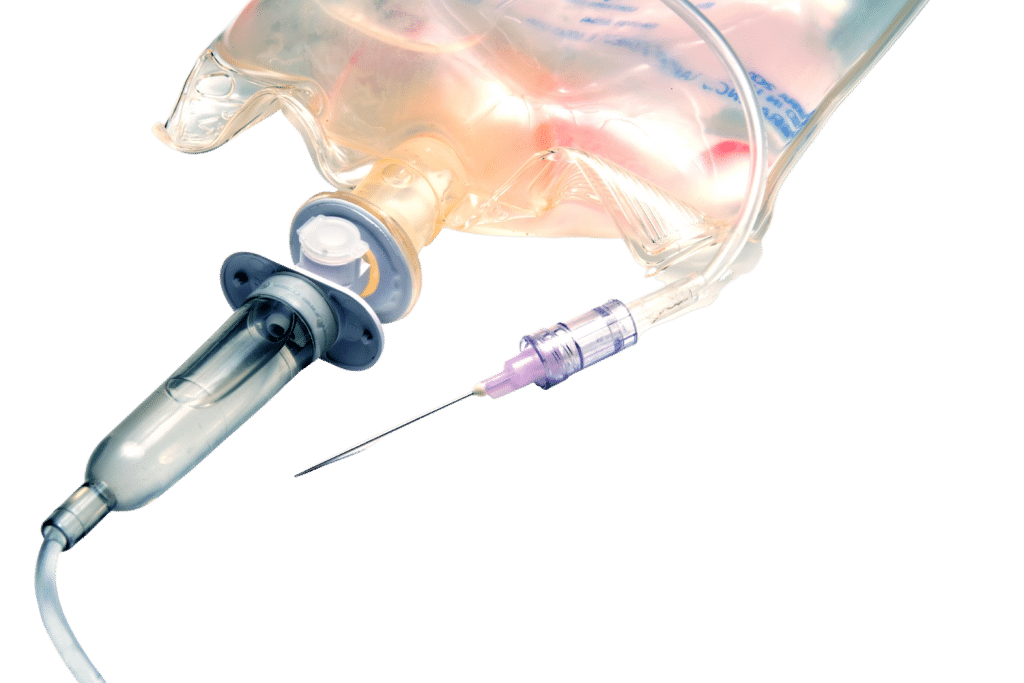
Ketamine clinics have been popping up like flies recently. While some ketamine providers use sublingual or intranasal ketamine, most administer the drug intravenously. This technique produces powerful dissociative effects in seconds — but carries some risk. Here’s what you need to know.
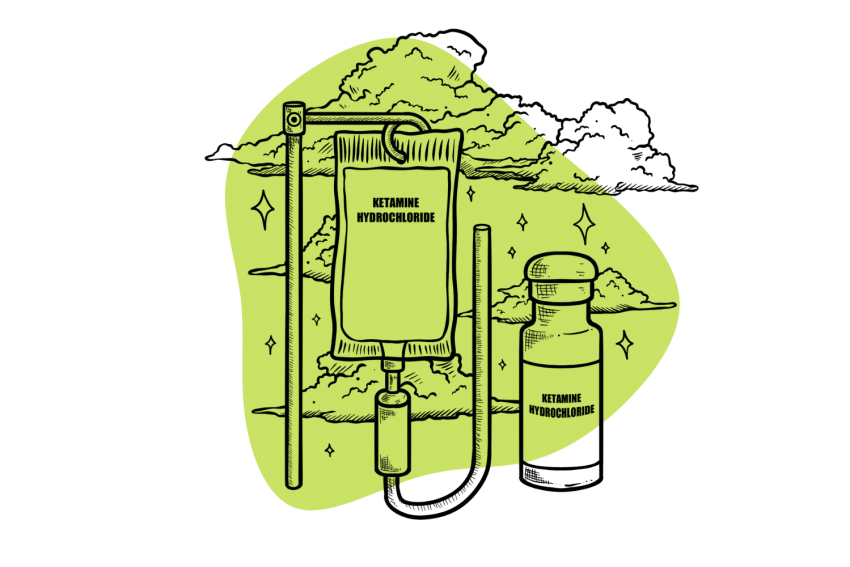
IV ketamine therapy is exactly what it sounds like the medical application of ketamine directly into the bloodstream through an intravenous (IV) line.
IV ketamine treatment usually takes place at a medical facility like a hospital or a specialized clinic and implies the involvement of medical professionals to supervise the therapy and keep an eye on important health measures such as blood pressure, heart rate, oxygen levels, and emotional well-being.
The intravenous ketamine solution is slowly infused into the blood throughout a period that, depending on the condition being treated and the specific needs of each patient, typically lasts just 40 minutes.
In its prevailing form, IV ketamine therapy is mostly utilized for the treatment of these three major ailments:
- Treatment-resistant depression and generalized anxiety disorders
- Post-traumatic stress disorder (PTSD)
- Chronic pain syndromes
- As a form of anesthesia during surgery
Now, to get a handle on the current state of IV ketamine therapy, let’s take a deeper look into these four applications and see what the scientific community has to say.
IV Ketamine For Treatment-Resistant Depression & Anxiety Disorders
A number of clinical studies and systematic meta-analyses have now furnished convincing evidence for the ability of IV ketamine therapy to successfully manage and or/improve the symptoms of treatment-resistant depression (TRD).
For example, let’s take a peek at this 2020 meta-analysis conducted by Marcatoni and Co. and published in the Journal of Affective Disorders.
In order to perform their analysis, the authors conducted a thorough sweep of five medical databases and identified 28 suitable primary studies which attempted to evaluate the effects of a sub-anesthetic dose of ketamine in adults experiencing TRD.
The conclusion of their meta-analysis definitely showed that infusion of ketamine significantly improved the management of depressive symptoms in the observed patients [1], an amazing result for those who have not yet found a suitable treatment for TRD!
More specifically, the authors noted that the beneficial effects of ketamine became apparent in as little as four hours following a single infusion and peaked at 24 hours. This fast-acting response, also identified in other clinical literature, is a significant advantage when ketamine is compared to other drugs used in the treatment of depression, like SSRI antidepressants.
However, the authors also identified the transient nature of ketamine’s benefits. At 7 days post-infusion, patients still felt improved symptoms but found the benefits to be somewhat diminished. As such, the authors state that ketamine infusions have a proven short-term effectiveness in the treatment of TRD but make no definitive conclusions about its long-term effectiveness and safety. On this front, further research is still needed.
Further bolstering the general claim made in this meta-analysis is a robust 2014 primary study with over 200 citations published in the Journal of Psychopharmacology.
This study identified the same fast-acting benefits and found that ketamine infusions can also be safely applied to patients who are currently on antidepressants [2]. However, the authors hedge their claim with a call for increased research as the long-term cognitive effect of multiple ketamine infusions remains significantly understudied. Also, it’s important to note that in certain patients, ketamine therapy produced increased anxiety or did not produce any meaningful improvements in depressive symptoms.
IV Ketamine For Post-Traumatic Stress Disorder (PTSD)
When compared to depression and anxiety disorders, the clinical literature concerning ketamine and its effects on PTSD is considerably more limited. Nevertheless, research-based conclusions for ketamine’s positive effects on PTSD symptoms have certainly been found.
One of the top researchers when it comes to ketamine’s beneficial effects on PTSD symptoms, Adriana Feder (MD), claims that, in a leading study, 67 percent of patients who received ketamine experienced both robust and rapid improvements in their PTSD symptoms [3]. This early result suggests an extremely promising future for ketamine in the treatment of PTSD symptoms.
As with depression and generalized anxiety disorders, researchers were quick to emphasize the fast-acting nature of ketamine, especially when compared to the standard array of drugs used to treat PTSD, which can take weeks or even months to become effective.
The study details how, In a short period of time, IV ketamine infusions allowed several patients to successfully face their trauma-related fears and even completely overcome some of their most debilitating symptoms like, for example, nightmares and flashbacks.
Unfortunately, the benefits of ketamine in PTSD also exhibit the transient nature identified in earlier depression-related studies. As such, the next step in ketamine therapy research is to identify methods that allow for the continued maintenance of symptom management, as well as the plausibility and efficacy of combining ketamine with other forms of treatment, whether medication or therapy-based.
IV Ketamine For Chronic Pain Syndromes
The research for ketamine’s potential applications in the field of pain management is the most robust. This is due to the fact that ketamine was originally developed as an anesthetic medication because of its analgesic and favorable safety profile.
This original application only lasted for a short time, though. After finding its penchant for dissociative effects and cardiovascular stimulation to be too unwieldy, the medical community moved on to more practical anesthetic drugs.
Indeed, ketamine’s analgesic effects have been known for a while. And with the arrival of new research, its potential role as a pain-management medication is looking brighter than ever.
For example, this 2014 study by Niesters and Co. concludes that there is significant evidence for ketamine’s ability to improve chronic pain symptoms in both the long and short term, especially those symptoms with a neuropathic component (related to the nervous system) [4].
A 2019 systematic review and meta-analysis also found evidence for ketamine’s benefits in the treatment of chronic pain conditions [5]. Specifically, they found significant short-term analgesic benefits in refractory chronic pain and some evidence for a dose-response relationship.
The biggest takeaway from these studies is that ketamine appears to show great effectiveness in the treatment of chronic neuropathic pain, even in the long term! The same fast onset of action was identified, and as an important consideration, many researchers highlighted the potential for ketamine to replace the widespread use of opioids as a first-line treatment in pain management. Due to the possibility of addictive symptoms linked to these opioid-based medications is a significant possibility that should be meaningfully explored.
It’s also important to note that results with other types of pain, such as acute and nociceptive (resulting from the activation of pain receptors by noxious stimuli), are less promising.

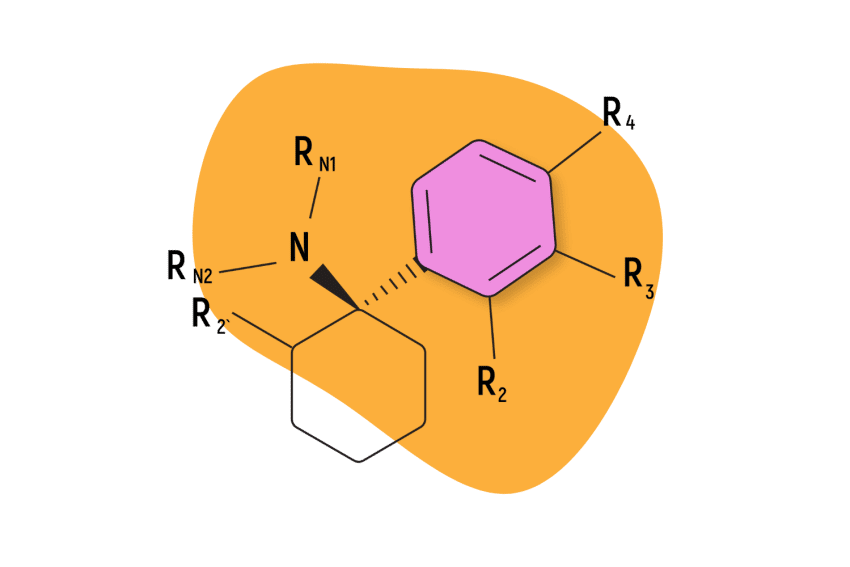
How Does Ketamine Work in the Body?
Ketamine is what’s known as an NMDA receptor antagonist. This means that, in the body, its primary mechanism of action is to bind to NMDA receptors and block their natural pharmacological effects. This operation is largely responsible for ketamine’s properties and applications, but it’s definitely not the only mechanism of action that’s been identified in the dissociative compound.
Some additional mechanisms of action related to ketamine include [6]:
- Sigma-1 receptor modulation — Ketamine can bind to and modulate the sigma-1 receptor, a protein found in various regions of the brain and associated with mood regulation. This quality of ketamine is believed to play a role in its antidepressant effects.
- AMPA receptor modulation — Ketamine has been shown to enhance the activity of alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, which are another type of glutamate receptor in the brain. This enhancement of AMPA receptor activity may contribute to the increased synaptic plasticity and the rapid antidepressant effects of ketamine.
- Dopamine modulation — Ketamine stimulates the release of dopamine in certain brain regions. The full implications of this property are not yet understood, as dopamine has a hand in several different physiological processes, such as reward, motivation, and mood regulation. It is highly likely that dopamine modulation plays a significant part in ketamine’s ability to influence and improve depressive symptoms.
- Serotonin modulation — Ketamine interacts with serotonin receptors (a key neurotransmitter involved in appetite, digestion, sleep, and much else) to produce intense feelings of dissociation, psychedelia, and hallucinations. Other serotonin-based effects are likely also present.
- Immunomodulation — Ketamine has anti-inflammatory properties and has been shown to reduce the production of pro-inflammatory cytokines in the brain. These compounds are involved in the inflammatory response and have been implicated in mood disorders, including bipolar disorder.
What Are the Side Effects of IV Ketamine Therapy?
The overwhelming conclusion in the clinical literature is that ketamine is generally well tolerated.
However, this, of course, does not mean that side effects cannot occur as a result of IV ketamine infusions.
One of the most common side effects of ketamine is the appearance of dissociative symptoms.
Ketamine is also known to increase blood pressure and heart rate. These side effects are normal and rarely something to worry about.
What Is the Current State of IV Ketamine Therapy?
As mentioned in the introduction, the state of IV ketamine therapy is still nascent.
When it comes to research, there is a healthy body of evidence showing ketamine’s effectiveness in dealing with a variety of conditions, but more is still needed in terms of long-term efficacy, safety, and co-administration with other treatments.
At the moment, ketamine is FDA-approved for use as an anesthetic and for the management of acute pain, while its use in chronic pain and mood disorders like TRF and generalized anxiety disorder (GAD) remains off-label.
There is at least one ketamine product that has been approved by the US Food and Drug Administration (FDA) for a specific medical indication. Esketamine, which is the S-enantiomer of ketamine, has been FDA-approved for the treatment of treatment-resistant depression in adults. It is available in the form of a nasal spray and is marketed under the brand name Spravato.

IV Ketamine Therapy: FAQs
Answering some of our most common questions around the intravenous application of ketamine.
1. Is IV Ketamine Covered By Insurance?
Due to the need for professional medical staff to monitor the infusion, yes, IV ketamine therapy can be relatively expensive, and the costs can add up over time, especially if multiple infusions are needed.
Also, because ketamine treatment is still not mainstream within the medical community, many insurance providers can be hesitant and argumentative when it comes to covering the costs of treatment. And when it comes to ‘off-label’ uses such as depression and anxiety, there is even less chance for coverage.
Some insurance plans may have policies that explicitly exclude coverage for off-label use of medications, while others may have more lenient policies that may cover off-label use on a case-by-case basis. It’s important to check with the individual insurance plan and review the specific coverage policies and requirements related to ketamine infusions for the intended indication.
However, it’s not all bad. It’s highly likely that with time ketamine therapy costs will come down, and insurance providers will be more willing to cover it.
2. What Does IV Ketamine Feel Like?
Describing such strange, subjective feelings as those produced by ketamine is not an easy task, and there is a lot of individual variation. But there is a general nature to the dissociative experience that we can try and put into words.
The effects produced by ketamine can include altered perception, changes in thought processes, loss of sense of self, emotional numbing, and dream-like or hallucinatory experiences.
Many people describe feeling detached and disconnected from their thoughts and surroundings, experiencing slowed or disjointed thinking, as well as emotional blunting and vivid dream-like or hallucinatory experiences that may be surreal or fantastical.
Subscribe to Tripsitter: Newsletter & Podcast
Unlock Your Mind: Subscribe for Expert Insights on Psychedelics 🍄🌵
References
- Marcantoni, W. S., Akoumba, B. S., Wassef, M., Mayrand, J., Lai, H., Richard-Devantoy, S., & Beauchamp, S. (2020). A systematic review and meta-analysis of the efficacy of intravenous ketamine infusion for treatment-resistant depression: January 2009–January 2019. Journal of Affective Disorders, 277, 831-841.
- Diamond, P. R., Farmery, A. D., Atkinson, S., Haldar, J., Williams, N., Cowen, P. J., … & McShane, R. (2014). Ketamine infusions for treatment-resistant depression: a series of 28 patients treated weekly or twice weekly in an ECT clinic. Journal of Psychopharmacology, 28(6), 536-544.
- Feder, A., Parides, M. K., Murrough, J. W., Perez, A. M., Morgan, J. E., Saxena, S., … & Charney, D. S. (2014). Efficacy of intravenous ketamine for the treatment of chronic post-traumatic stress disorder: a randomized clinical trial. JAMA psychiatry, 71(6), 681-688.
- Niesters, M., Martini, C., & Dahan, A. (2014). Ketamine for chronic pain: risks and benefits. British journal of clinical pharmacology, 77(2), 357-367.
- Orhurhu, V., Orhurhu, M. S., Bhatia, A., & Cohen, S. P. (2019). Ketamine infusions for chronic pain: a systematic review and meta-analysis of randomized controlled trials. Anesthesia & Analgesia, 129(1), 241-254.
- Mion, G., & Villevieille, T. (2013). Ketamine pharmacology: an update (pharmacodynamics and molecular aspects, recent findings). CNS neuroscience & therapeutics, 19(6), 370-380.