Is Ketamine An Opioid?
The opioid crisis has everyone on edge about anything that looks like an opioid. While ketamine is not one, it has risks of its own.

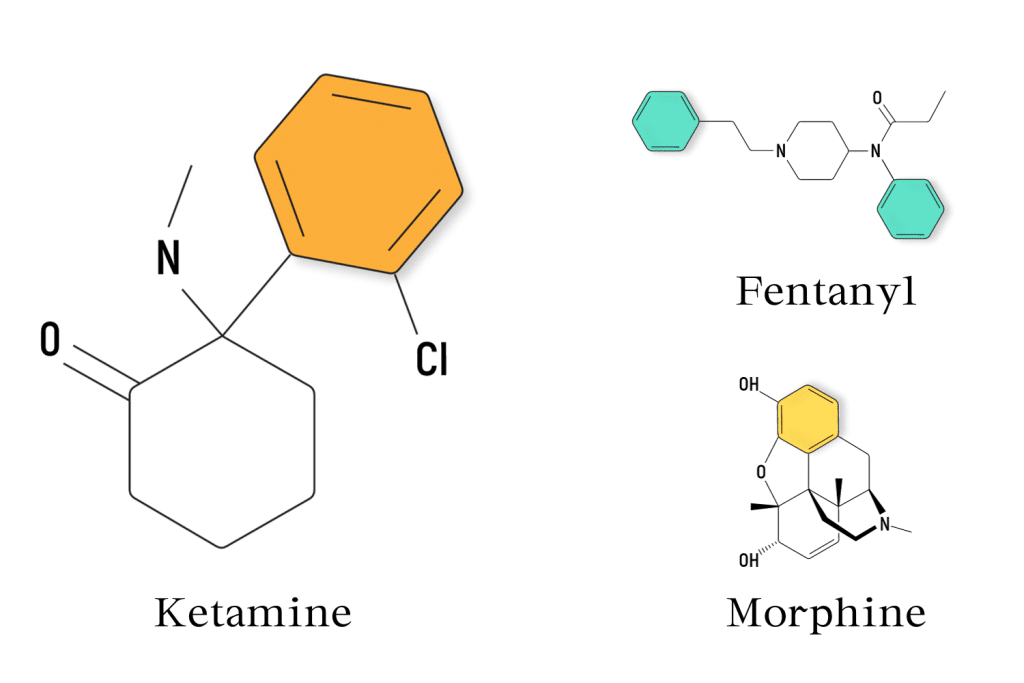
Ketamine isn’t an opioid like oxycodone, fentanyl, or heroin. However, its potent analgesic properties make it a formidable contender for treating pain and depression.
Ketamine’s classification is confusing because it can tango with opioid receptors, but its primary dance partner is the NMDA receptor. And unlike opioids, it doesn’t depress the central nervous system.
Ketamine can alleviate pain for cancer patients who can’t stand opioids — but that’s not all. It’s also making waves in the world of psychedelic exploration, offering users profoundly transformative experiences in navigating mental health.
But before diving into how ketamine exerts its effects, let’s start with a crash course in its history to explore this misconception of ketamine as an opioid.
Why Do People Think Ketamine Is An Opioid?
Rewind to 1970. Ketamine made its commercial debut under the name “Ketalar.” Its label read “rapidly acting, nonbarbiturate general anesthetic,” hinting at its potential for short medical procedures.
The drug quickly found its place in emergency medicine and battlefield scenarios due to its unique properties, such as maintaining stable heart and lung function during anesthesia, a significant advantage over other anesthetic agents.
The misconception that ketamine is an opioid likely came from its analgesic effects and sedative nature, which can produce a trance-like state. However, the underlying mechanisms of action between ketamine and opioids are quite distinct.
As research evolved, we discovered that ketamine might potentially reduce opioid use, especially for managing pain and some mental health challenges.
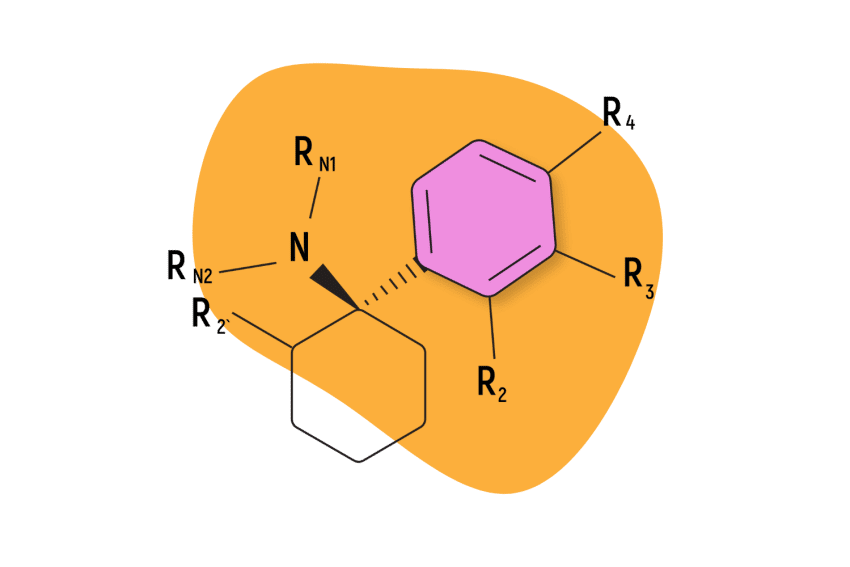
Mechanism of Action: How Ketamine Works
Ketamin may interact with the opioid system, but it’s not as pronounced or addictive as the bond opioids form with these receptors. Its main action is on the NMDA receptors.
NMDA receptors are crucial for the brain’s communication, with signals constantly zipping between nerve cells (or neurons). These signals are the reason we think, feel, and act.
When ketamine steps in, it temporarily “blocks” some of this communication.
This NMDA receptor blockade is like hitting the mute button on the television, reducing the volume of signals in the brain. By doing this, ketamine can alter our sensations, perceptions, and even emotions. This action is why it’s so effective as an anesthetic — it can “mute” or “dull” certain signals, causing a loss of sensation.
But that’s not the whole story, which is why ketamine’s use extends past pain management into mental health.
Traditional antidepressants target serotonin or dopamine, but researchers noticed something exciting with ketamine — its ability to provide rapid relief from depressive symptoms.
By blocking the NMDA receptor, ketamine may encourage the growth of new synaptic connections between neurons, helping the brain “reset” in some ways and even relieving those who haven’t responded to conventional treatments [1].
Ketamine also flirts with other systems in the brain, such as the monoamine, cholinergic, and adrenoreceptor systems, which influence neurotransmitter receptors involved in mood, motivation, memory, learning, and even the fight-or-flight response. These interactions add layers to ketamine’s effects, making its profile diverse.
What Does Ketamine Feel Like?
Ketamine is a unique substance whose effects vary depending on the dose, the individual, and the setting. Let’s take a look at some common themes:
- Dissociation: The “K-hole” is often likened to an ‘out-of-body’ experience. Many users feel detached as if floating above or apart from their physical selves. This disconnection can stretch further, making the familiar world around them feel distant or unreal.
- Visual and Auditory Changes: Colors may become more vibrant, sounds might seem distant or distorted, and perceptions of time feel altered. Some describe it as being submerged underwater, where everything feels and sounds far away.
- A Sense of Peace or Tranquility: Despite its intense dissociative properties, many find a sense of peace while under ketamine’s influence, where the mind’s incessant chatter seems to fade, and in its place, a profound stillness emerges.
- A Feeling of Weightlessness: As the drug takes hold, limbs might feel light or lose awareness of their body altogether. It’s as if gravity loosens its grip, leaving users floating in an expansive space.
- Euphoria: Not everyone, but some, describe a rush of euphoria, a sweeping warmth, or a burst of uncontrollable laughter.
- Spiritual or Mystical Experiences: Some people recount profound revelations or feelings of interconnectedness similar to experiences from deep meditative states at higher doses, especially in controlled, therapeutic settings.

Side Effects and Risks of Ketamine Use
Like any drug, ketamine isn’t without risks.
Some might experience mild side effects like dizziness, while others grapple with more severe implications like dependence or cerebrovascular diseases. And if you’ve got issues like psychosis, severe liver disease, or even glaucoma, tread cautiously — ketamine might not be your friend.
Over time and with repeated use, there’s a risk of developing a psychological dependence on ketamine, which can negatively affect mental health and brain function.
It’s also worth noting that consuming large doses of ketamine or mixing it with other substances can lead to an overdose. At the mild end, you could lose consciousness, and in severe cases, you could lose your life.
What Is a K-Hole?
The term might sound ominous, but a k-hole is an intense dissociative experience users might have after taking a hefty dose of ketamine.
It’s been described as a state of profound detachment from reality, akin to an out-of-body experience. It’s fascinating but not for the faint of heart, as feeling disconnected from your body can be frightening.
What Does Ketamine Feel Like?
Ketamine is a dissociative drug and can give ‘out-of-body’ experiences. Many users say they feel detached as if floating above or apart from their physical selves.
At lighter dosages, the world can take on a dreamy haze. Colors may appear more vibrant, and sounds may seem distorted or distant. With dissociative drugs, it’s common for one’s perception of time to feel altered, and thinking can become laborious or disjointed. Some report feeling as though their thoughts are fragmented or viewing the world through a new, often perplexing, lens.
Despite its intense dissociative properties, many find a sense of serenity while under ketamine’s influence. The mind’s incessant chatter might quieten, and a profound stillness can emerge.
Some people describe a rush of euphoria, a sweeping warmth, or a burst of uncontrollable laughter.
At higher doses, especially in controlled therapeutic settings, some people recount profound revelations or feelings of interconnectedness akin to those described by mystics or during deep meditative states.
Confusion or disorientation tends to happen during the onset of or coming down from ketamine. Users may feel disoriented or have difficulties processing their surroundings.
Related: Curious About Ketamine? Here’s the Rundown on What to Expect

What Is Ketamine Used for In Medicine?
Ketamine is most known as an anesthetic, but its uses go far beyond that.
1. Local or Regional Anesthesia
When doctors need to numb just a part of the body, like during stitches, they often use ketamine, even for kids.
Given in low doses, it ensures the patient is relaxed but also remains safe, partly because it can boost the body’s circulatory response [2].
2. Anesthesia for Surgery
Ketamine acts quickly after administration; its recovery time is generally shorter than many other anesthetics.
Another notable feature of ketamine for surgical use is its ability to maintain protective airway reflexes, making it less risky, especially in places with limited medical infrastructure.
3. Treatment for Burns
Changing dressings or grafting skin on serious burns is excruciating. Ketamine can be applied topically as a gel or a cream to smaller burns or wounds, offering direct, localized comfort.
Oral ketamine can also be prescribed for long-term pain management for patients who require extended care.
4. Prevention of Shivering Post-surgery
Waking up from anesthesia, some patients might feel super cold and start shivering. It’s not just uncomfortable, but it can also be risky for the cardiovascular system.
For shivering prevention, intravenous ketamine is administered in sub-anesthetic doses for a smoother post-operative recovery.
5. Chronic Pain Management
Ketamine has shown promise in treating various forms of chronic pain, like neuropathic pain (nerve-related pain), pain from phantom limbs (when amputees feel pain in a limb that isn’t there), and even the widespread pain of conditions like fibromyalgia.
In clinical settings, low-dose ketamine infusions might be administered, or patients may receive an oral ketamine prescription for long-term chronic pain management. Even nasal sprays are available for enhanced bioavailability, which may be better suited for conditions like chronic migraines.
6. Cancer Pain
For patients in palliative care who focus on comfort, ketamine is a valuable teammate to opioids, ensuring pain is kept at bay.
There’s some evidence suggesting that ketamine may amplify the effects of opioids, which may allow patients to have lower doses of opioids alongside ketamine to achieve the same pain relief. These are administered in intravenous infusions at the hospital or as oral ketamine, which tends to be less common.
Ketamine & Psychedelic-Assisted Therapy
In higher doses, especially in controlled therapeutic settings, ketamine can induce states of dissociation. Again, this is largely thanks to how ketamine acts on the NMDA receptor, altering the usual flow of signals in the brain.
This “out-of-body” sensation offers some patients a new perspective, allowing them to address traumatic or deeply entrenched negative thought patterns. By distancing patients from their usual thought processes, identifying and challenging problematic patterns may become easier, leading to meaningful insights and resolutions.
Under the guidance of trained professionals, these experiences can be channeled into positive therapeutic breakthroughs.
While traditional antidepressants may take weeks to show effects, some patients experience relief within hours to days after ketamine treatment. For those grappling with severe, even suicidal thoughts, this rapid response can be life-saving.
Is Ketamine Legal In the United States & Canada?
In the U.S., ketamine is a Schedule III controlled substance restricted to medical purposes for anesthetic, pain management, and treating psychiatric disorders. Depending on the state, illegal possession can lead to severe penalties like fines or imprisonment.
In Canada, ketamine is a Schedule I drug, placing it under strict regulation with similar consequences for illicit use. Even with stricter controls, ketamine is recognized for its medical applications as an anesthetic. However, illegal drug possession can result in hefty fines and even imprisonment.
Related: Four Good (And Not So Good) Ways to Get Ketamine
The Takeaway: Ketamine Is Not An Opioid
Mistaking ketamine for an opioid is an oversimplification. While ketamine and opioid drugs manage pain, they operate very differently.
Medically, ketamine wears many hats, from its role as a surgical anesthetic to treating severe depression and chronic pain. It’s also being explored for its profound psychedelic experiences alongside professional therapeutic intervention, which may be promising for treatment-resistant depression.
Appreciating ketamine’s unique properties and distinct identity from opioids can guide its safe and effective use.
Subscribe to Tripsitter: Newsletter & Podcast
Unlock Your Mind: Subscribe for Expert Insights on Psychedelics 🍄🌵
References
- Duman, R. S., Li, N., Liu, R. J., Duric, V., & Aghajanian, G. (2012). Signaling pathways underlying the rapid antidepressant actions of ketamine. Neuropharmacology, 62(1), 35-41.
- Kurdi, M. S., Theerth, K. A., & Deva, R. S. (2014). Ketamine: current applications in anesthesia, pain, and critical care. Anesthesia, essays and researches, 8(3), 283.