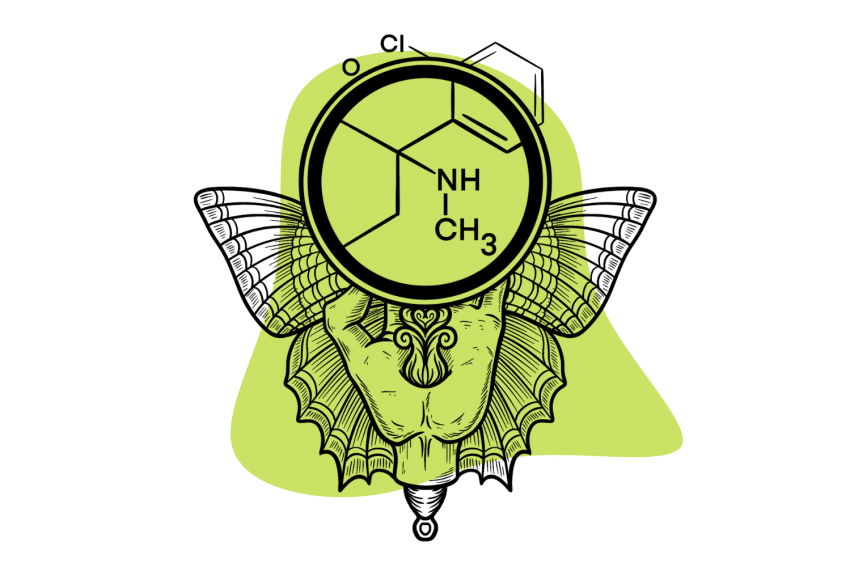
Could Ketamine be a New Treatment for OCD?
Ketamine’s efficacy in treating OCD has yet to be proven effective. However, many have claimed the drug has brought unquestionable relief, and research has opened the door for new, never-before-explored approaches to this debilitating condition.
It seems there’s a new headline every day touting ketamine as a miracle cure for a new, deeply complex mental health condition. When it comes to treating OCD, however, don’t expect to hear that anytime soon.
While some have found relief from their debilitating symptoms, only a small percentage — of a small sample size of patients — have found it helpful. When it was, the effects rarely seemed to last beyond the duration of ketamine, ranging up to a week at most.
This doesn’t mean there isn’t something to ketamine, though.
Below, we’ll cover everything you need to know on the topic, including:
- Ketamine’s Efficacy In Treating OCD
- What is OCD
- Neurological Markers and Causes of OCD
- Pharmacological Mechanisms for Ketamine Treating OCD
- Therapeutic Benefits of Ketamine Treatment for OCD
- When Ketamine Therapy for OCD is Most Effective
- Current Treatment Options for OCD
While the studies don’t feel as conclusive as the other potential options for ketamine, its unique pharmacology and effects still provide relief to some.
Is Ketamine An Effective Treatment for OCD?
While ketamine therapy has shown rapid, short-lived effectiveness for several mental health concerns, obsessive-compulsive disorder (OCD) is still uncertain. Some studies show a “clinically significant” — usually 35% — reduction, often returning to baseline within a week [1].
One survey from 2023 reviewed over 14 studies, revealing how uncertain the results are:
- One study found “8 of 12 participants had no ketamine response, and none of the participants showed significant” improvement by the 6-week follow-up.
- Another open-label study found “no clinical improvement” for any of its 10 participants.
- Over 50% of participants in randomized controlled trials (RCTs) reported a reduction in “obsessive and intrusive symptoms,” but it was a similar result to the placebo group.
- One RCT involving 15 participants and two 40-minute infusions found that 50% of the ketamine group had a reduction in symptoms compared to the placebo group after a week.
- Case studies involving individual reports show ketamine can provide rapid, potentially long-term relief for some, but not all.
While some results show promise, others raise more questions than they answer. Much of this boils down to the complex causes of OCD and the ways ketamine might help.
Since the severity of OCD symptoms can vary so greatly, each case is unique — as is the efficacy of ketamine treatment. Furthermore, the importance of therapy in treating OCD may be more important than any pharmacological measure.
Most research on OCD treatment revolves around how well new measures improve therapeutic outcomes. If ketamine does help, it is unlikely to do so without other interventions into the root causes of the condition.
What is OCD?
Obsessive-compulsive disorder (OCD) represents itself in a few different ways, but the commonality is obsessive thought patterns and compulsive actions. In severe cases, this can be a debilitating experience, leaving the person unable to break free from their actions or thoughts.
These might manifest as repeatedly checking, organizing, cleaning, or moving things around or as a crippling fear of death, embarrassment, germs, and more. A variation of OCD — obsessive-compulsive personality disorder (OCPD) — may manifest as an obsession with organization and cleanliness.
People suffering from OCD are almost always aware of the compulsiveness of their actions and thought patterns but cannot break free from them. Living with OCD is incredibly difficult, even as the severity of symptoms begins to decrease with medication and therapy.
Therapeutic interventions along with a selective serotonin reuptake inhibitor (SSRI) like escitalopram or fluoxetine (name brands Lexapro and Prozac) [2]. These interventions take time, are effective for 60–75% of patients, and rarely result in a complete remission of symptoms.
An instant cure — something companies often position ketamine as — would be tremendously helpful. Even a recent study on the experimental partial NMDA receptor agonist, d-cycloserine, largely discusses its ability to bolster the effects of talk therapy [3].
Sadly, there doesn’t seem to be an option for immediately reliably relieving symptoms, partially due to the pharmacological reasons for OCD symptoms.
What Causes OCD?
OCD is a condition with a wide range of severity and is due to various causes, from genetic to environmental. The condition affects serotonin, dopamine, glutamate, and gamma-aminobutyric acid (GABA) [1].
It’s uncertain whether these neurological markers are a result of OCD or the way it manifests, but they seem to play a significant role. Here’s how each of these seems to contribute to OCD symptoms (according to limited research):
- Dopamine — High levels of this transmitter can lead to over-activity and involuntary movements (tics) OCD patients often suffer from [4].
- Serotonin — Responsible for regulating mood, communicating with the brain, and a host of other functions, patients with OCD seem to have lower levels of serotonin compared to baseline [5].
- Glutamate — This neurotransmitter is responsible for exciting the brain into action and occurs in significantly higher quantities in patients with OCD [6].
- GABA — The reverse of the above, GABA brings rest and inhibition to the brain and shows up in lower concentrations for patients with OCD [7].
These are responsible for many of the symptoms of OCD, though we still don’t know what causes it. Ketamine also interacts with each of these and may help temporarily restore balance to some of them — emphasis on “temporary.”
Research suggests there’s potential to hand the condition down genetically, but there may be psychological or traumatic reasons underlying it. These may be all symptoms themselves of a greater cause and, with the variability of how symptoms present in people with OCD, each case — and treatment — is unique.
Ketamine and OCD: Pharmacological Mechanisms
Ketamine’s influence on similar pathways responsible for many of the symptoms of OCD has led many to think it could be beneficial. While confirmation is a long way off, some studies have shown promise for ketamine’s potential to raise GABA levels without elevating glutamate, potentially bringing some ease to symptoms [8].
Benefits seem to be higher for patients who have OCD along with depression, which may point to ketamine’s antidepressant effect more than anything. Studies have yet to look into the varying forms of ketamine therapy or dosing regimens, but it seems:
- Single doses of ketamine rarely provide relief from OCD symptoms lasting beyond the effects of the ketamine (sometimes not even that)
- Repeated doses may help elevate GABA over time without elevating glutamate over time
- High doses of ketamine can result in an acute surge of glutamate, potentially worsening symptoms during administration [9]
Ketamine’s pharmacological importance may be a jumping-off point for other NMDAR modulators in the future. It seems there may be a benefit to ketamine for a percentage of people with OCD, but it’s far from perfect.
Other drugs have sought to build off the novel mechanism ketamine employs but have yet to find significant success. Part of this may come from the other benefit ketamine offers — the trip itself — which they often try to remove.
Ketamine and OCD: Therapeutic Mechanisms
Like other forms of psychedelic-assisted psychotherapy, ketamine has a much higher rate of success alongside qualified mental health care. Cognitive behavioral therapy (CBT) — which aims to redirect malignant thought patterns — alongside ketamine has shown tremendous potential in small sample sizes [10].
This has been the default treatment for OCD for a long time, but paired with ketamine, it may become much more powerful.
In high doses, ketamine makes users feel detached from their bodies, thoughts, and emotions, which can feel relieving for anyone with OCD. As the drug wears off and symptoms return, however, it’s easy to settle back into a routine and not integrate the experience into your life.
Off-label clinics and telehealth providers often do very little in this regard, so it’s important to have a qualified professional you trust. Through CBT, patients can take the moments of relief from ketamine and use them to remap thought patterns to provide new tools for dealing with symptoms.
There’s a lot of debate right now on whether the trip is more important than the pharmacological elements of psychedelics. As one review of the topic put it, the pharmacological effect “cannot be divorced from the psychomimetic and dissociative effects [8].”
The truth is, it’s likely both go into a successful result, and the dissociative effects of ketamine may embolden the therapeutic value. Without improving a patient’s mental health through therapy, these mental concerns will never truly dissipate.
When is Ketamine Therapy Most Effective for OCD?
While ketamine research has shown a mixture of results, there do appear to be some forms of OCD for which it is better suited. Namely, OCD with high levels of anxiety and depression may receive a greater benefit due to ketamine’s anti-anxiety and antidepressant effects.
However, this could come from the relief of depression or anxiety alone, making OCD symptoms easier to manage. Due to the number of bodily systems OCD impacts — not to mention the mental, emotional, and environmental factors — treating it is complex.
Speculation surrounds ketamine’s capability to modulate glutamate since it’s a major factor in OCD. However, research has yet to definitively show its effectiveness, and some studies conclude it wasn’t helpful for their sample size.
When it is beneficial for OCD symptoms, treating any mental health disorder will typically require extensive therapy. Though we can identify neurological markers for a condition, treating the psychological underpinnings thereof takes work.
This means ketamine therapy will always be more effective when patients pair it with extensive behavioral and emotional therapy. Mental health always requires more than a single pill, drug, or substance to work through, and a trained professional can help you get to a far healthier place.
Current Treatments for OCD
The National Institute of Mental Health (NIMH) lists several treatment options, mostly revolving around psychotherapy. While antidepressants, anti-anxiety medications, or other pharmaceutical approaches may help ease symptoms, they mostly aim to make talk therapy more effective.
Cognitive Behavioral Therapy (CBT) focuses on the underlying “learned” behaviors we form as a defense to our surroundings and forming new mechanisms for dealing with them. There are various ways to go about this, but the main thing is re-visiting your triggers, understanding what causes them, and creating tools to work through them.
The two main routes OCD treatment takes involve:
- Exposure and Response Prevention Therapy (ERP) — “Exposure therapy,” as people commonly call it, involves intentionally confronting your triggers and learning how to move past them.
- Repetitive Transcranial Magnetic Stimulation (rTMS) — Magnetic pulses directed at specific areas of the brain to stimulate the nerves and reportedly improve mental health symptoms.
These have varying levels of efficacy but have shown promise for a variety of mental health concerns.
Other, more drastic measures like Electroconvulsive Therapy (ECT) or Deep Brain Stimulation (DBS) require surgery or anesthesia and are typically a last resort.
Ketamine’s Impact On the Future of OCD Treatment
Ketamine’s efficacy is drastically lower than CBT with medication, but it still raises some interesting questions. For all the concerns surrounding ketamine as a treatment for OCD, it is undeniably helpful for some — which has researchers looking at how ketamine works.
As a result, several new pharmaceutical candidates aim to inhibit, activate, and modulate the NMDA receptor and glutamate [11]. Nothing too exciting has come onto the scene yet, but ketamine’s unique pharmacology has the pharmaceutical manufacturing industry abuzz.
Ketamine uses completely different mechanisms of action from other interventions aimed at treating the same mental health concerns people are turning to it for. Perhaps, with time, we’ll look back on ketamine as opening the door to an entirely new class of treatment options.
In the meantime, we won’t overstate how effective ketamine is in treating OCD — while its mechanisms are exciting, they’re far from perfect.
Frequently Asked Questions: Ketamine Therapy for OCD
Here are some of the common questions people ask about ketamine therapy to treat OCD:
1. Is Ketamine An Effective Treatment for OCD?
Ketamine treatment has been useful for a low percentage of participants in a small amount of research. It appears to be more beneficial for people with severe OCD or co-morbidities of depression or anxiety, but talk therapy is still the best treatment option for OCD.
Ketamine’s benefit may come from a temporary relief from debilitating symptoms, but patients shouldn’t expect the effect to last beyond a week — and often far less. Even new medications aiming to treat OCD mostly focus on how well they assist therapeutic measures.
2. What Are Some Other Psychedelic Therapies for OCD?
Psychedelic-assisted psychotherapy involves a lot of potential mechanisms, but the therapeutic component seems most critical. In a pleasant environment, with a professional a person trusts, and with foundational therapeutic work beforehand, it’s incredibly likely psychedelics could help treat most mental health conditions.
The main trap to avoid is the risk of “pharmacological determinism” — the idea of treating every problem with a pill. Psychedelics on their own and without critical support and infrastructure may do more harm than good.
Still, small case studies have shown a remarkable amount of efficacy for magic mushrooms [12] and LSD [13], among others, along with therapy.
3. Can You Treat OCD With Ketamine at Home?
No pill, drug, or other substance will reliably cure a condition as complex as OCD, and ketamine (along with other psychedelics) can worsen symptoms in some instances. Even in controlled clinical trials, small-to-moderate percentages of participants feel a beneficial effect.
When they do work, it’s almost always for less than 3-7 days. Self-medication with ketamine opens the risk of a negative experience impacting your symptoms along with the addictive escape of a quickly-dissolving ketamine experience.
Additionally, it’s possible to wind up in a paranoid state with crippling anxiety on ketamine. In a therapeutic context, patients can potentially work through and understand these settings, but it requires professional support.
4. Is Ketamine a Safe Treatment Option for OCD?
Generally speaking, reasonable doses of ketamine intermittently are unlikely to lead to complications. However, ketamine’s rapid effect and short duration of alleviating symptoms often mean people have to return for frequent sessions.
Ketamine’s toxicity on the liver and urinary tract makes this dangerous, potentially leading to medical complications. As the compounds build up in the system, serious conditions can develop and may require medical intervention.
While it’s unlikely for this to happen in an off-label clinic, telemedicine also leaves the door open for unsafe behaviors before, during, and after. Offering little-to-no therapeutic oversight, ketamine telehealth companies leave the powerful drug in the hands of people at home.
Within all of this, there are wise and unwise times to reach for ketamine. If you have OCD (or any other social or depressive condition), consider an off-label clinic or discuss it with a mental health professional — preferably one not employed by the telehealth company.
Subscribe to Tripsitter: Newsletter & Podcast
Unlock Your Mind: Subscribe for Expert Insights on Psychedelics 🍄🌵
References
- Ferguson, A. A., Khan, A. I., Abuzainah, B., Chaudhuri, D., Khan, K. I., Al Shouli, R., Allakky, A., & Hamdan, J. A. (2023). Clinical Effectiveness of N-Methyl-D-Aspartate (NMDA) Receptor Antagonists in Adult Obsessive-Compulsive Disorder (OCD) Treatment: A Systematic Review. Cureus, 15(4), e37833. https://doi.org/10.7759/cureus.37833
- Goodman, W. K., Storch, E. A., & Sheth, S. A. (2021). Harmonizing the Neurobiology and Treatment of Obsessive-Compulsive Disorder. The American Journal of Psychiatry, 178(1), 17–29. https://doi.org/10.1176/appi.ajp.2020.20111601
- Rosenfield, D., Smits, J. A. J., Hofmann, S. G., Mataix-Cols, D., de la Cruz, L. F., Andersson, E., Rück, C., Monzani, B., Pérez-Vigil, A., Frumento, P., Davis, M., de Kleine, R. A., Difede, J., Dunlop, B. W., Farrell, L. J., Geller, D., Gerardi, M., Guastella, A. J., Hendriks, G.-J., … Otto, M. W. (2019). Changes in Dosing and Dose Timing of D-Cycloserine Explain Its Apparent Declining Efficacy for Augmenting Exposure Therapy for Anxiety-related Disorders: An Individual Participant-data Meta-analysis. Journal of Anxiety Disorders, 68, 102149. https://doi.org/10.1016/j.janxdis.2019.102149
- Koo, M.-S., Kim, E.-J., Roh, D., & Kim, C.-H. (2010). Role of dopamine in the pathophysiology and treatment of obsessive-compulsive disorder. Expert Review of Neurotherapeutics, 10(2), 275–290. https://doi.org/10.1586/ern.09.148
- Lissemore, J. I., Sookman, D., Gravel, P., Berney, A., Barsoum, A., Diksic, M., Nordahl, T. E., Pinard, G., Sibon, I., Cottraux, J., Leyton, M., & Benkelfat, C. (2018). Brain serotonin synthesis capacity in obsessive-compulsive disorder: Effects of cognitive behavioral therapy and sertraline. Translational Psychiatry, 8, 82. https://doi.org/10.1038/s41398-018-0128-4
- Karthik, S., Sharma, L. P., & Narayanaswamy, J. C. (2020). Investigating the Role of Glutamate in Obsessive-Compulsive Disorder: Current Perspectives. Neuropsychiatric Disease and Treatment, 16, 1003–1013. https://doi.org/10.2147/NDT.S211703
- Brain Gamma-Aminobutyric Acid (GABA) Concentration of the Prefrontal Lobe in Unmedicated Patients with Obsessive-Compulsive Disorder: A Research of Magnetic Resonance Spectroscopy. (n.d.). Shanghai Archives of Psychiatry, 28(5), 263–270. https://doi.org/10.11919/j.issn.1002-0829.216043
- Martinotti, G., Chiappini, S., Pettorruso, M., Mosca, A., Miuli, A., Di Carlo, F., D’Andrea, G., Collevecchio, R., Di Muzio, I., Sensi, S. L., & Di Giannantonio, M. (2021). Therapeutic Potentials of Ketamine and Esketamine in Obsessive–Compulsive Disorder (OCD), Substance Use Disorders (SUD) and Eating Disorders (ED): A Review of the Current Literature. Brain Sciences, 11(7), Article 7. https://doi.org/10.3390/brainsci11070856
- Abdallah, C. G., De Feyter, H. M., Averill, L. A., Jiang, L., Averill, C. L., Chowdhury, G. M. I., Purohit, P., de Graaf, R. A., Esterlis, I., Juchem, C., Pittman, B. P., Krystal, J. H., Rothman, D. L., Sanacora, G., & Mason, G. F. (2018). The effects of ketamine on prefrontal glutamate neurotransmission in healthy and depressed subjects. Neuropsychopharmacology, 43(10), 2154–2160. https://doi.org/10.1038/s41386-018-0136-3
- Rodriguez, C. I., Wheaton, M., Zwerling, J., Steinman, S. A., Sonnenfeld, D., Galfalvy, H., & Simpson, H. B. (2016). Can Exposure-Based CBT Extend IV Ketamine’s Effects in Obsessive-Compulsive Disorder? An Open-Label Trial. The Journal of Clinical Psychiatry, 77(3), 408–409. https://doi.org/10.4088/JCP.15l10138
- Pittenger, C. (2015). Glutamate modulators in the treatment of obsessive-compulsive disorder. Psychiatric Annals, 45(6), 308–315. https://doi.org/10.3928/00485713-20150602-06
- Moreno, et al. (n.d.). Safety, Tolerability, and Efficacy of Psilocybin in 9 Patients With Obsessive-Compulsive Disorder. https://doi.org/10.4088/jcp.v67n1110
- Zghoul, T., & Blier, P. (2003). Enhancing action of LSD on neuronal responsiveness to serotonin in a brain structure involved in obsessive–compulsive disorder. International Journal of Neuropsychopharmacology, 6(1), 13–21. https://doi.org/10.1017/S1461145702003218